Case Report - Archives of Clinical and Experimental Surgery (2022)
A Case of Large Gastric Perforation due to Bezoar
Hina Gupta1*, Ranjeet Ahirwar1, Avinash Gautam1, Suyog Andhare1 and Ram Mohan Shukla22Department of Pediatric Surgery, M.G.M. Medical College and M.Y. Hospital, Madhya Pradesh, India
Hina Gupta, Department of General Surgery, M.G.M. Medical College and M.Y. Hospital, Madhya Pradesh, India, Tel: +918379949489, Email: guptahina1996@gmail.com
Received: 03-Oct-2022, Manuscript No. EJMACES-22-76492; Editor assigned: 06-Oct-2022, Pre QC No. EJMACES-22-76492 (PQ); Reviewed: 21-Oct-2022, QC No. EJMACES-22-76492; Revised: 28-Oct-2022, Manuscript No. EJMACES-22-76492 (R); Published: 04-Nov-2022
Abstract
Background: A bezoar is a tightly packed collection of partially digested or undigested material found trapped in the gastro-intestinal system, Though, it can occur in other locations in the body as well, the most common location is the stomach. When unrecognized, these habits of eating bezoars can lead to severe complications such as gastric ulceration and even perforation.
Methods: We report a case of 55 year old Indian male who presented to the emergency room with signs and symptoms of acute abdomen. Radiological study revealed bilateral pneumoperitoneum. Personal history revealed depressive symptoms.
Results: An emergency exploratory laparotomy was performed and gastric perforation with 800 gms of gravel stones in the enlarged stomach were present as a content. Anterior gastrojejunostomy with Feeding jejunostomy was performed after removal of stones. Patient was discharged on post-operative day 10 and followed up for post op complications and referred to psychiatry for further therapy.
Conclusion: Acute abdomen with hollow viscus perforation is an emergency where saving the time is crucial to avoid further peritonitis, shock or mortality. Gastrointestinal perforation and peritonitis in association with lithobezoars are rare entities where emergency interventions are must needed. Therefore, in patients with psychiatric behaviour and unusal dietary habits, bezoars as a differential diagnosis needs to be ruled out and managed with further psychiatric therapy.
Keywords
Bezoar; Perforation; Pneumoperitoneum; Exploratory laparotomy; Gastrojejunostomy; Feeding jejunostomy; Gravel
Introduction
Bezoars were introduced to Europe from Middle East during 11th century as medicinal remedies. The word bezoar comes from 18th century derived from the Persian word pad-zahr meaning “antidote”. The physician in west known by the name “Avenzoar” had made earliest description of bezoar stones [1]. For medicinal purposes, the widely used bezoars were Animal bezoars at that time [2]. Bezoars are intraluminal mass formed by accumulation of partially digested or undigested products trapped in the gastrointestinal system of human body. These bezoars can be of different types depending upon content and location. According to the location, they can be esophagus, stomach, large intestine or even trachea. According to the type of content, these can be, food boluses, lactobezoars, pharmabezoars, trichobezoars, phytobezoars [3]. Out of which gastric trichobezoars are commonly encountered.
Bezoars account for reported incidence of 0.07% to 0.4%, usually occur secondary to depressive symptoms, behavioral disorders, abnormal gastric emptying or altered gastrointestinal anatomy [4]. Usually patients have a long history of ingestion of such materials with dull aching pain in abdomen, intermittent vomiting and disturbed bowel habits leading to obstructive symptoms, gastrointestinal bleeding, ileus, ulceration and perforation. We here report a case of perforation peritonitis secondary to gastric bezoar.
Case Presentation
55 years old male presented to the casualty with complaints of pain in abdomen since 2 months which got aggravated in last 3 days associated with multiple episodes of vomiting since 5 days. It was also associated with not passing motion and flatus since 1 day. The patient had history of eating gravels since 5 months. The attenders also gave history of acid ingestion 2 years back. The patient was suffering from depressive and behavioral disorders since 2 years. He had no other comorbidities. He had no previous surgical history.
Examination and investigations
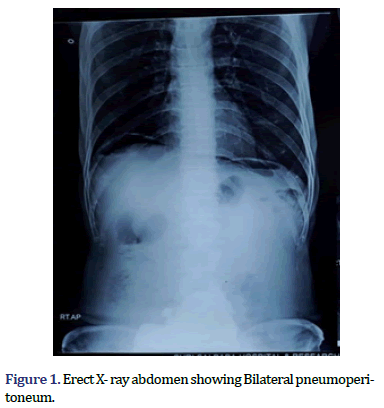
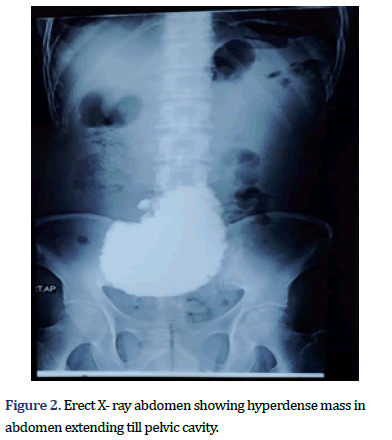
On examination, he was fully conscious and vitally stable. Per abdomen examination revealed distention of abdomen with generalized tenderness, guarding. On per rectal examination fecoliths were present. Blood investigations revealed an elevated leukocyte count. Radio- imaging (X-ray erect) revealed a bilateral pneumoperitoneum and radio-opaque shadow in the shape of stomach extending till pelvic cavity (Figures 1 and 2). Ultrasonography suggested a mild ascites with echoes.
Surgical intervenion
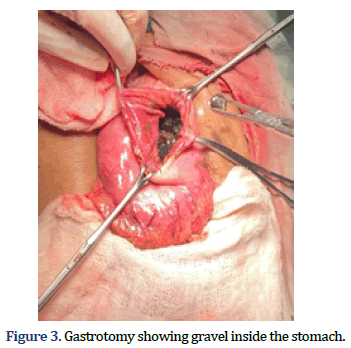
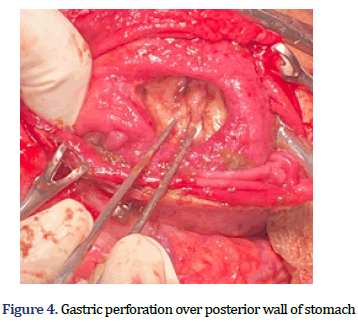
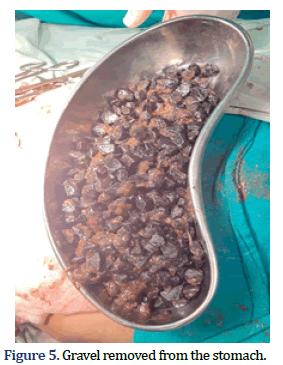
The patient underwent an emergency exploratory laparotomy. Approx. 1.5 L of purulent fluid was found in peritoneal cavity with enlarged stomach of (approx. 10 cm × 8 cm) with 3 cm × 2 cm perforation over the lesser curvature of posterior wall of stomach. Gravel stones present inside the stomach were palpable from the perforation site (Figure 3). Approx. 8 cm of Gastrotomy was performed in the anterior wall and 300 gravel stones weighing 800 gm were removed (Figures 4 and 5). Anterior Gastro-jejunostomy with primary repair of gastric perforation and feeding jejunostomy was performed (Figure 6). Post-operative period was uneventful. The patient was discharged on postoperative day 14 and Feeding Jejunostomy was kept in situ for 2 weeks. Patient was on regular follow-up. Patient recovered well without any complications and is undergoing regular psychiatric treatment.
Results and Discussion
Gastric bezoars were first described during the autopsy of a patient who died from gastric perforation and peritonitis [5]. The condition usually occurs in patients with psychiatric disorders with the incidence estimated to be 0.4 to 1% in the general population. Bezoars are classified as per their composition as phytobezoars (composed of vegetable fibres), trichobezoars (balls of hair or hair like fibres), lithobezoars (fragments of stones), pharmacobezoars (pills), lactobezoars (composed of milk products), plasticobezoars (plastic).
The symptoms depend upon the size of bezoars and the presence of complications. If there is a large bezoar, it is generally retained in the stomach due to presence of pyloric sphincter with symptoms of pyloric obstruction as was seen in our patient. Patients usually present with epigastric pain, nausea and vomiting, hematemesis, weight loss, diarrhea and constipation. In our case, patient presented with pain in abdomen, multiple episodes of vomiting, and obstipation with chronic history of eating gravels. If gastric bezoar is slow growing and left untreated for long time, it increases in size leading to various complications like gastric obstruction, ulceration or perforation which was the case in our patient as he presented to the emergency with perforation peritonitis.
These bezoars are diagnosed by radiological imaging such as x-rays, endoscopy, Computed Tomography scan [6]. Our patient underwent X-ray abdomen in emergency which showed Bilateral pneumoperitoneum and opaque shadow of stomach. Ultrasound of abdomen showed mild as- cites with echoes.
The treatment of bezoars includes removal of the mass and prevention of the recurrence with psychiatric treatment. It can be chemical dissolution, endoscopic removal, surgery or a combination of therapy. Chemical dissolution is mostly preferred for phytobezoars whereas endoscopic removal can be done for those bezoars which fail to dissolve or if the initial diagnosis was done with endoscopy then it is removed in the same sitting. Endoscopic removal is only possible for small bezoars which can be removed with the help of basket or direct suction. It is less effective for large bezoars [7]. Surgical removal of bezoars is done when chemical dissolution and endoscopic removal has failed, patients with complications or for intestinal bezoars, large or solid bezoars leading to perforation or hemorrhage. Since patient presented to the emergency with features of perforation peritonitis, patient was taken for emergency laparotomy. Primary repair of gastric perforation after removal of lithobezoars was done with anterior gastrojejunostomy and feeding jejunostomy was done for the patient. To reduce recurrence, psychiatric treatment and regular follow up in psychiatric OPD are advised.
Conclusion
Bezoars have different ways of presentation. Acute abdomen with hollow viscus perforation is an emergency where saving time is crucial to avoid further peritonitis, shock or mortality. Gastrointestinal perforation and peritonitis in association with lithobezoars are rare entities where emergency intervention is needed. Therefore, thorough history and clinical examination for behavioral disorders with prompt diagnosis, early intervention, and follow up with proper psychiatric evaluation is must for early intervention, good prognosis and prevention of recurrence of such conditions. Hence, in patients with psychiatric behaviors and unusual dietary habits, bezoars as a differential diagnosis needs to be ruled out and managed with further psychiatric therapy.
References
- Williams RS. The fascinating history of bezoars. Med J Aust 1986;145(11-12):613-4.
[Crossref] [Google Scholar] [Pubmed]
- Eng K, Kay M. Gastrointestinal bezoars: History and current treatment paradigms. Gastroenterol Hepatol (N Y) 2012;8(11):776-8.
[Google Scholar] [Pubmed]
- Valenciano JS, Nonose R, Cruz RB, Sato DT, Fernandes FC, Nascimento EF, et al. Tricholithobezoar causing gastric perforation. Case Rep Gastroenterol 2012;6(1):26-32.
[Crossref] [Google Scholar] [Pubmed]
- Akbulut S, Değer KC, Duman M, Yol S. Gastric bezoars. Prz Gastroenterol 2016;11(1):60-1.
[Crossref] [Google Scholar] [Pubmed]
- Hewitt AN, Levine MS, Rubesin SE, Laufer I. Gastric bezoars: Reassessment of clinical and radiographic findings in 19 patients. British J Radiol 2009;82(983):901-7.
[Crossref] [Google Scholar] [Pubmed]
- Iwamuro M, Okada H, Matsueda K, Inaba T, Kusumoto C, Imagawa A, et al. Review of the diagnosis and management of gastrointestinal bezoars. World J Gastrointest Endosc 2015;7(4):336-45.
[Crossref] [Google Scholar] [Pubmed]
- Mao Y, Qiu H, Liu Q, Lu Z, Fan K, Huang Y, et al. Endoscopic lithotripsy for gastric bezoars by Nd: YAG laser-ignited mini-explosive technique. Lasers Med Sci 2014;29(3):1237-40.
[Crossref] [Google Scholar] [Pubmed]
Copyright: © 2022 The Authors. This is an open access article under the terms of the Creative Commons Attribution NonCommercial ShareAlike 4.0 (https://creativecommons.org/licenses/by-nc-sa/4.0/). This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.