Research Article - Archives of Clinical and Experimental Surgery (2024)
A Comparative Study of Conventional Hemorrhoidectomy vs. Anoderm-Preserving Partial Hemorrhoidectomy after BANANA-Clip Ligation for Grade III-IV Hemorrhoids: Retrospective Study
Dong Wan Kang*, Byoung Soo Kim, Ji Hun Kim, Kyong Rae Kim and Gyong Suk KangDong Wan Kang, Department of Colorectal Surgery, Wellness Hospital, Busan, South Korea, Email: dwkangdr58@gmail.com
Received: 08-Nov-2024, Manuscript No. EJMACES-24-151999; Editor assigned: 11-Nov-2024, Pre QC No. EJMACES-24-151999 (PQ); Reviewed: 25-Nov-2024, QC No. EJMACES-24-151999; Revised: 02-Dec-2024, Manuscript No. EJMACES-24-151999 (R); Published: 09-Dec-2024
Abstract
Background: Chronic non-healing wounds, delayed bleeding, and recurrence are concerns for both patients and physicians following hemorrhoid surgery. Debate continues over which surgical method effectively reduces these side effects in grade III-IV hemorrhoids.
Objective: This study aimed is to evaluate the incidence of chronic non-healing wounds and other complications following anoderm-preserving Partial Hemorrhoidectomy (PH) after BANANA-Clip (BC) ligation, compared to conventional hemorrhoidectomy in patients with grade III-IV internal hemorrhoids.
Design: This was an observational study conducted at a single institution to compare complications between partial hemorrhoidectomy after BANANA-Clip and conventional hemorrhoidectomy in patients with grade III-IV internal hemorrhoids.
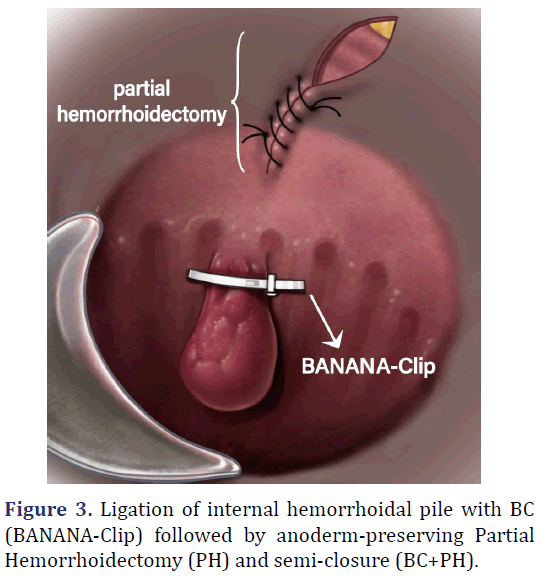
Setting: Partial hemorrhoidectomy after BANANA-Clip involves ligation of the proximal hemorrhoidal pile with BANANA-Clip followed by dissection up to the distal half of the anoderm from the external sphincter border, while preserving the proximal half of the anoderm.
Patients: Study participants consisted of patients who received surgical intervention for grade III-IV hemorrhoids at the Department of Colorectal Surgery, Wellness Hospital, from 1 January 2019 to 30 November 2020.
Main outcome measures: The primary outcome was the incidence of chronic nonhealing wounds.
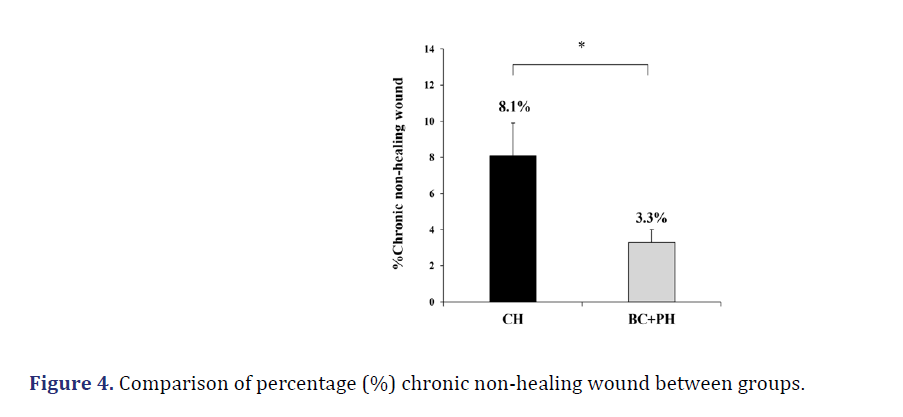
Results: The incidences of chronic non-healing wounds were 8.1% for conventional hemorrhoidectomy and 3.3% for partial hemorrhoidectomy after BANANA-Clip (p=0.002). The adjusted odds ratio for chronic non-healing wounds comparing partial hemorrhoidectomy after BANANA-Clip to conventional hemorrhoidectomy was 0.467 (95% CI (Confidence Interval): 0.240-0.907, p=0.02), after adjusting for other variables.
Limitations: This study had a retrospective design, and data on pain scores were no included.
Conclusion: Patients who underwent partial hemorrhoidectomy after BANANA-Clip demonstrated a significantly lower incidence of chronic non-healing wounds compared to those who underwent conventional hemorrhoidectomy.
Keywords
Partial hemorrhoidectomy; BANANA-Clip; Chronic non-healing wound; Delayed bleeding
Introduction
The stages of wound healing are sequential but overlap with one another. If a postoperative wound fails to progress through stages in a timely and orderly fashion, healing will be delayed. A wound that does not achieve anatomical and functional restoration within three months is classified as a Chronic Non- Healing Wound (CNHW) [1].
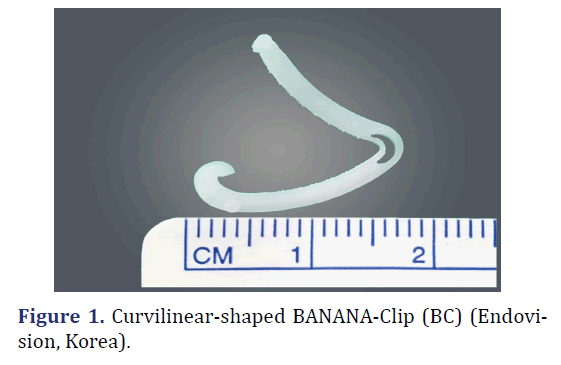
Wounds resulting from Conventional Hemorrhoidectomies (CH) heal by secondary intention. This type of healing means that the wounds are left open to allow new tissue growth, rather than being closed primarily [2]. If the anal wound is left open to granulation, the prolonged time required for complete healing, the considerable discomfort caused by the large raw area and the inevitable scarring can lead to troublesome stenosis [3]. In connection with this, some anal wounds do not heal within three months after hemorrhoidectomy, becoming CNHWs. Grade III-IV hemorrhoids, which prolapse from the distal rectum to beyond the anal verge, are commonly treated with CH resulting in extensive surgical wounds and a higher risk of CNHWs. We hypothesized that a combination of ligation with the BANANA-Clip (BC) (BC; Product License No. 22-4268, Endovision, Korea) (Figure 1), and anoderm-preserving partial hemorrhoidectomy (BC+PH) would be more effective in preventing CNHWs than CH alone.
Materials and Methods
Study design and patients
This retrospective study included 934 consecutive patients who underwent surgical treatment for grade III-IV internal hemorrhoids at Wellness Hospital, Korea, from January 1, 2019, to November 30, 2020. The primary objective was to compare the incidence of chronic non-healing wounds and other significant complications between the surgical methods used (CH group: 234 patients vs. BC+PH group: 700 patients). Additionally, we analyzed confounding factors such as gender, age, grade, and the number of hemorrhoidectomy sites.
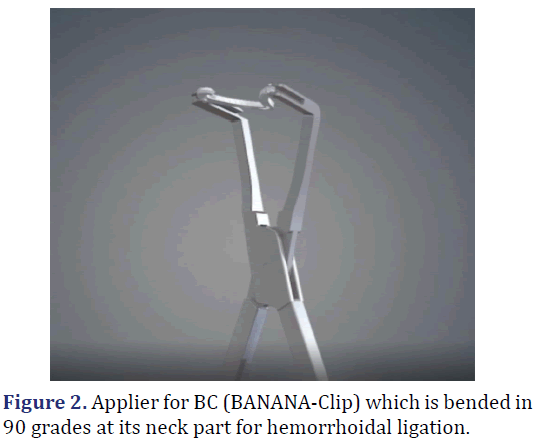
We used the BC instead of Barron’s rubber band, which is currently one of the most frequently practiced treatments for symptomatic internal hemorrhoids6 and has replaced traditional hemorrhoidectomy in 44.8% of cases [4-7]. This approach was based on study results showing that Delayed Bleeding (DB) was statistically significantly lower (0.0%), and stenosis did not occur even when three BCs were ligated in a single session [8]. The BC, named for its banana-like curvilinear shape, induces necrosis of hemorrhoidal tissues and detaches from the rectal wall within one to two weeks, similar to a rubber band. It exits through the anal canal during defecation, almost without causing a foreign body sensation. Even when three clips are applied simultaneously, rectal stenosis does not occur because it only constricts hemorrhoidal tissue longitudinally to the rectal axis if placed 2 cm above the dentate line. The applicator’s head is bent at a 90-degree angle8 to adjust its approach to the neck of the hemorrhoidal pile and to align BC transversely to the anorectal axis (Figure 2).
The study enrolled patients aged 18 years and older with grade 3-4 internal hemorrhoids who had no history of prior anal surgery and had refrained from taking anticoagulant medications for 7 days before surgery. Exclusion criteria included patients with diabetes mellitus and HbA1C levels above 10, those diagnosed with CHILD C cirrhosis, and individuals with a history of coagulation disorders.
Data collection
For this study, medical records from 1 January 2019 to 30 November 2020 were analysed. The data collected were de-identified by removing identifiers such as names, resident registration numbers, patient numbers, addresses, and contact information. Clinical research documents, like case records, were anonymized using pseudonyms instead of subjects’ names. Following this de-identification process, the research was conducted retrospectively. This study was reviewed and approved by the Korean Public Institutional Review Board designated by the Ministry of Health and Welfare (No. P01-202309-01-014). Written informed consent was waived due to its retrospective nature.
Sample size and power calculation
This retrospective study primarily aimed to compare the incidence of chronic non-healing wounds between patients who underwent surgery for grade III-IV internal hemorrhoids using two different surgical methods (CH vs. BC+PH). Preliminary data from a pilot study showed that the incidence of chronic non-healing wounds was 9.0% for CH and 4.0% for BC+PH. Given that the ratio of patients treated with the two methods during the study period was approximately 1:3, a total of 934 patients was required to achieve a significance level of 0.05 and a statistical power of 80% (CH group: 234 patients vs. BC+PH group: 700 patients). The sample size was calculated using nQuery Advisor 7.0 (Statistical Solutions, Saugus, MA).
Data analysis
Variables were summarized by frequency and percentage for categorical data, and by mean ± standard deviation and median (minimum-maximum) for numerical data. Group differences were assessed using the chi-squared or Fisher’s exact tests for categorical data, and the independent t-test or Mann- Whitney U test for numerical data, as appropriate. To verify normal distribution, the Shapiro-Wilk test was utilized. Univariate and multivariate analyses using binary logistic regression were conducted to identify independent prognostic factors related to the primary outcome, which is the incidence of chronic non-healing wounds. For data visualization, an error-bar chart was displayed. All statistical analyses were performed using SPSS 26.0 (IBM Corp., released 2019, IBM SPSS Statistics for Windows, Version 26.0, Armonk, NY: IBM Corp), and p-values less than 0.05 were considered statistically significant.
Surgical procedure and postoperative care
Prophylactic antibiotics were not administered prior to surgery. The CH procedure was performed in the jackknife position using electrocautery under local or spinal anesthesia. Hemorrhoids were excised from the outer edge of the external anal sphincter up to 2 cm above the dentate line. The excised tissue, including the superior hemorrhoidal artery, was then sutured and ligated. Blood vessels in the anal mucosa on both sides of the wound were removed, and the wound itself was sutured to the anal verge using absorbable sutures.
BC+PH was performed in the same manner as CH, using the same anesthesia and patient positioning. After inserting the Ferguson dilator into the anus and securing the surgical field, tooth forceps were used to grasp the proximal part of the internal hemorrhoid. If the hemorrhoid was suitable for ligation with BC, the clip was deployed using an applier with the neck bent at 90 degrees. The distal half of the anoderm was excised, and the external hemorrhoidal mass extending beyond the anal verge was elliptically removed up to the outer edge of the external sphincter and sutured with absorbable sutures, leaving a drainage window open (Figure 3). Patients were administered oral metronidazole and phlebotonics for up to 7 days postsurgery. Pain management was facilitated through an intravenous Patient-Controlled Analgesia (PCA) device. Depending on their condition, patients were discharged 1-2 days post-surgery. Dressings were recommended for approximately 2-3 weeks post-discharge. Wound care and observation were conducted in the outpatient department 7 and 14 days after discharge. At the end of the 2 or 3 outpatient visits, patients were instructed to schedule a follow-up appointment in three months. A wound was considered fully healed if there was complete re-epithelialization or closure without any discharge [9]. If a wound had not healed by this time, characterized by persistent bleeding and mucous discharge, it would be classified as a chronic nonhealing wound. If a patient returns to the outpatient department one year later with symptoms such as bleeding and prolapse originating from the surgical site, this is classified as a recurrence.
Results
This study included 934 patients (CH, 234; BC+PH, 700) who underwent surgical treatment for grade IIIIV internal hemorrhoids between January 1, 2019, and November 30, 2020, at the Department of Colorectal Surgery, Wellness Hospital. Table 1, outlines the patients’ baseline characteristics. The male-to-female ratio was 0.319 (=226/708), and the mean ages were 36.8 years in the CH group and 45.1 years in the BC+PH group (p<0.001). Among the participants, 5.5% (51 patients) were on anticoagulant therapy. The primary symptoms necessitating treatment included prolapse (96.8%), bleeding (56.4%), and pain (41.1%). Although all patients with these grades are expected to report hemorrhoidal prolapse, some reported no prolapse at their initial outpatient clinic visit. Additional symptoms included constipation (23.7%), thrombosis (14.9%), stenosis (11.7%), and pruritus (8.0%). Of the patients, 163 (17.5%) underwent surgery under local anesthesia and 771 (82.5%) under spinal anesthesia. The choice of anesthesia was determined in consultation with the patient and the physician. Of all patients, 377 (40.4%) had grade III and 557 (59.6%) had grade IV hemorrhoids, with a significantly higher incidence of grade IV hemorrhoids in the CH group (70.5%) compared to the BC+PH group (56.0%) (p<0.001). The observed challenges are likely due to the difficulty in ligating large internal hemorrhoids at grade IV with BC and the potential future re-prolapse of the abundant anoderm tissue. In the BC+PH group, an average of 2.0 ± 0.8 hemorrhoids were ligated per session using BC. Of these patients, 296 (42.3%) underwent double ligations, 196 (28.0%) underwent triple ligations, and 6 (0.9%) underwent quadruple ligations, with no cases of stenosis observed. The average number of hemorrhoids treated per session was 2.2 ± 0.8 in CH and 1.9 ± 0.8 in PH, a statistically significant difference (p<0.001). It can be inferred that the number of excision sites in the BC+PH group is lower than in the CH group. This is likely because the external hemorrhoids, typically excised in the CH group, were often reduced in size in the BC+PH group due to the lifting effect after BC ligation, eliminating the need for excision. For instance, the 1-excision rate was 21.8% and the 3-excision rate was 30.3% in the CH group compared to 32.7% and 17.0% in the BC+PH group, respectively. The higher 1-excision rate and lower 3-excision rate in the BC+PH group suggest a decreased need to remove three hemorrhoids due to the reduced size post-ligation. The mean resting and squeezing anal pressures in the high- pressure zone were not significantly different between groups (CH group: 72.4 ± 15.5 mmHg, 132.2 ± 29.8 mmHg; BC+PH group: 71.6 ± 15.6 mmHg, 135.2 ± 31.8 mmHg). The duration from surgery day to the end of outpatient treatment averaged 26.6 ± 39.2 days in the CH group and 22.3 ± 21.9 days in the BC+PH group, showing no significant difference. The percentage of patients who did not attend a follow-up appointment three months post-outpatient treatment was 15.0% (35 patients) in the CH group and 18.3% (128 patients) in the BC+PH group, which was also not significantly different.
| Variable | Overall (n=934) | CH (n=234) | BC+PH (n=700) | p value |
|---|---|---|---|---|
| Gender | ||||
| Male | 226 (24.2) | 27 (11.5) | 199 (28.4) | <0.0013 |
| Female | 708 (75.8) | 207 (88.5) | 501 (71.6) | |
| Age (years) | ||||
| Mean ± SD | 43.0 ± 14.0 | 36.8±12.9 | 45.1 ± 13.7 | <0.0012 |
| median (min-max) | 42.0 (18-85) | 34.0 (18-79) | 45.0 (18-85) | |
| Anticoagulant | ||||
| Yes | 51 (5.5) | 7 (3.0) | 44 (6.3) | 0.053 |
| No | 883 (94.5) | 227 (97.0) | 656 (93.7) | |
| Main symptoms | ||||
| Prolapse | 904 (96.8) | 220 (94.0) | 684 (97.7) | 0.0053 |
| Bleeding | 527 (56.4) | 120 (51.3) | 407 (58.1) | 0.073 |
| Pain | 384 (41.1) | 114 (48.7) | 270 (38.6) | 0.0063 |
| Constipation | 221 (23.7) | 64 (27.4) | 157 (22.4) | 0.133 |
| Thrombosed | 139 (14.9) | 37 (15.8) | 102 (14.6) | 0.643 |
| Stenosis | 109 (11.7) | 21 (9.0) | 88 (12.6) | 0.143 |
| Pruritus | 75 (8.0) | 28 (12.0) | 47 (6.7) | 0.013 |
| Anesthesia | ||||
| Local | 163 (17.5) | 80 (34.2) | 83 (11.9) | <0.0013 |
| Spinal | 771 (82.5) | 154 (65.8) | 617 (88.1) | |
| Grade | ||||
| III | 377 (40.4) | 69 (29.5) | 308 (44.0) | <0.0013 |
| IV | 557 (59.6) | 165 (70.5) | 392 (56.0) | |
| No. of ligations | ||||
| Mean ± SD | 2.0 ± 0.8 | - | 2.0 ± 0.8 | |
| median (min-max) | 2.0 (1-4) | 2.0 (1-4) | ||
| One | 202 (28.9) | - | 202 (28.9) | |
| Two | 296 (42.3) | - | 296 (42.3) | |
| Three | 196 (28.0) | - | 196 (28.0) | |
| Four | 6 (0.9) | - | 6 (0.9) | |
| No. of CH/PH | ||||
| Mean ± SD | 2.0±0.8 | 2.2±0.8 | 1.9±0.8 | <0.0014 |
| median (min-max) | 2.0 (1-6) | 2.0 (1-6) | 2.0 (1-6) | |
| One | 280 (30.0) | 51 (21.8) | 229 (32.7) | |
| Two | 437 (46.8) | 104 (44.4) | 333 (47.6) | |
| Three | 190 (20.3) | 71 (30.3) | 119 (17.0) | |
| Four | 23 (2.5) | 7 (3.0) | 16 (2.3) | |
| Five | 2 (0.2) | 0 (0.0) | 2 (0.3) | |
| Six | 2 (0.2) | 1 (0.4) | 1 (0.1) | |
| Anal pressure | ||||
| Resting pressure of HPZ (n=774) | ||||
| Mean ± SD | 71.8 ± 15.6 | 72.4 ± 15.5 | 71.6 ± 15.6 | 0.482 |
| median (min-max) | 72.9 (31-166) | 73.6 (33-163) | 72.7 (31-166) | |
| Squeezing pressure of HPZ (n=774) | ||||
| Mean ± SD | 134.5 ± 31.3 | 132.2 ± 29.8 | 135.2 ± 31.8 | 0.172 |
| median (min-max) | 132.1 (33-273) | 130.5 (50-249) | 132.5 (33-273) | |
| Length of time from Surgery to end of treatment (days) | ||||
| Mean ± SD | 23.4 ± 27.3 | 26.6 ± 39.2 | 22.3 ± 21.9 | 0.332 |
| median (min-max) | 18.0 (1-437) | 19.0 (2-437) | 17.0 (1-333) | |
| Number of patients who did not do follow up after 3 months | 163 (17.5) | 35 (15.0) | 128 (18.3) | 0.253 |
Note: Data are presented as mean ± SD or number (%), unless otherwise indicated; 1p values were derived from independent t-test; 2p values were derived from Mann-Whitney’s U test; 3p values were derived by chi-square test; 4p values were derived from Fisher’s exact test; CH-Conventional Hemorrhoidectomies; BC- BANANA Clip; PH- Partial Hemorrhoidectomy |
||||
CNHWs occurred in 42 patients (4.5% of the total of 934 patients), 19 patients (8.1%) in the CH group and 23 patients (3.3%) in the BC+PH group, with a statistically significant decrease in the latter (Table 2 and Figure 4). Just as Goligher3 found that any delay in healing was always related to the skin-lined part of the canal below the pectinate line to the perianal skin, in our study chronic non-healing wounds in both groups were located in the distal half of the anoderm. There was no statistical significance when resting anal pressure (70.1 ± 13.6 mmHg) and squeezing anal pressure (129.1 ± 29.2 mmHg) in the high pressure zone of 42 patients with chronic non-healing wounds were compared with resting anal pressure (71.9 ± 15.7 mmHg) and squeezing anal pressure (134.7 ± 31.4 mmHg) of the remaining 892 patients (resting: p=0.37, squeezing: p=0.23, (Supplementary Table 1). The effect of independent variables on CNHWs was analyzed using univariate and multivariate logistic regression analysis (Tables 3 and 4).
| Variable | Overall (n=934) | CH (n=234) | BC+PH (n=700) | p value |
|---|---|---|---|---|
| Chronic non-healing wound | 42 (4.5) | 19 (8.1) | 23 (3.3) | 0.0021 |
| Skin tag | 19 (2.0) | 5 (2.1) | 14 (2.0) | 1.0002 |
| Thrombosis | 16 (1.7) | 5 (2.1) | 11 (1.6) | 0.562 |
| Recurrence (at 1 year after op) | 10 (1.1) | 3 (1.3) | 7 (1.0) | 0.7182 |
| Clip slippage | 7 (0.7) | 0 (0.0) | 7 (1.0) | 0.202 |
| Dysuria | 7 (0.7) | 2 (0.9) | 5 (0.7) | 1.0002 |
| DB | 5 (0.5) | 1 (0.4) | 4 (0.6) | 1.0002 |
| Anal fistula | 5 (0.5) | 2 (0.9) | 3 (0.4) | 0.602 |
| Anal stenosis | 1 (0.1) | 1 (0.4) | 0 (0.0) | 0.252 |
Note: Data are presented as number (%);
1p values were derived by chi-square test;
2p values were derived from Fisher’s exact test;
CH-Conventional Hemorrhoidectomies; BC- BANANA Clip; PH- Partial Hemorrhoidectomy; DB-Delayed Bleeding
In the univariate analysis, 42 patients with CNHWs were younger (38.5 vs. 43.3 years, Odds Ratio [OR]: 0.974, 95% Confidence Interval [CI]: 0.951-0.998, p=0.03) and had a lower rate of BC+PH (54.8% vs. 75.9%, OR: 0.384, 95% CI: 0.205-0.719, p=0.003) than the remaining 892 patients. Patients with CNHWs were associated with female sex, lower grade, and a higher number of hemorrhoidectomy surgery sites; however, these factors were not statistically significant compared with the remaining 892 patients (p>0.05).
In a multivariate analysis, covariates included the surgery method (BC+PH vs. CH) as well as the statistically significant variables in Table 1, such as gender, age, grade, and number of hemorrhoidectomy surgery sites. Multivariable analyses showed that BC+PH was associated with a lower number of CNHWs than CH (Adjusted Odds Ratio [AOR]=0.467, 95% CI: 0.240-0.907, p=0.02) after adjusting for patient gender, age, grade, and number of hemorrhoidectomy surgery sites (Table 3). Patients who underwent CH had a higher grade and a higher number of hemorrhoidectomy surgery sites; after adjusting for all these variables, patients who underwent BC+PH still showed a significantly lower incidence of CNHWs. However, the incidence of CNHW in the CH group, at 8.1%, is significant, indicating that further research is necessary to understand its underlying cause.
| Variable | Chronic non-healing wounds | Others | Univariate analysis odds ratio (95% CI) | P value | Multivariate analysis adjusted odds ratio (95% CI) | p value |
|---|---|---|---|---|---|---|
| N | 42 | 892 | ||||
| Surgical method BC+PH, % | 54.8 | 75.9 | 0.384 | 0.003 | 0.467 | 0.02 |
| (0.205-0.719) | (0.240-0.907) | |||||
| Gender male, % | 14.3 | 24.7 | 0.509 | 0.13 | 0.632 | 0.33 |
| (0.212-1.224) | (0.249-1.602) | |||||
| Age, years (SD) | 38.5 (13.8) | 43.3 (14.0) | 0.974 | 0.03 | 0.982 | 0.17 |
| (0.951-0.998) | (0.958-1.007) | |||||
| Grade IV, % | 59.5 | 59.6 | 0.995 | 0.99 | 0.727 | 0.35 |
| (0.530-1.869) | (0.373-1.418) | |||||
| Number of hemorrhoidectomy surgery sites (SD) | 2.1 (0.8) | 2.0 (0.8) | 1.214 | 0.3 | 1.141 | 0.5 |
| (0.843-1.748) | (0.780-1.669) |
Note: Data are presented as mean ± SD or number (%), unless otherwise indicated.
Of the 42 patients with CNHWs, 32 were treated surgically and the remaining 10 were treated with oral medications such as bulking agents, stool softeners, and anal ointments. One patient in each group received a closed lateral internal sphincterotomy; the rest were treated with wound debridement. Additionally, 4 patients in the CH group and 12 patients in the BC+PH group received botulinum toxin injections of 10 units each on the left and right sides of the internal sphincter muscle.
In addition, there was no significant difference in the complication rates of skin tag, thrombosis, recurrence, clip slippage, dysuria, DB, anal fistula, and anal stenosis between the two groups (Table 3). Although BC ligation was not performed in the CH group, the risk of clip slippage in the BC+PH group was nonetheless statistically not significant. In this study, DB occurred in a total of 5 patients (0.5%) (CH: 1 patient; BC+PH: 4 patients). In one case in the CH group, it was caused by bleeding from the superior hemorrhoidal artery, so it was controlled by suture ligation. In the BC+PH group, in all 4 cases, the bleeding was not at the ligation site with BC, but at the excision site of the anoderm, so the bleeding was controlled by compression. Although the amount of analgesics used can be a criterion for evaluating the outcome of both groups, it was not measured in this study because analgesia was administered to the majority of patients via a Patient- Controlled Analgesia (PCA) pump.
| Variable | Total (n=42) | CH (n=19) | BC+PH (n=23) | p value |
|---|---|---|---|---|
| Anal pressure | ||||
| Resting pressure of HPZ (n=36) | ||||
| Mean ± SD | 70.1 ± 13.6 | 72.5 ± 14.0 | 67.9 ± 13.1 | 0.152 |
| Median (min-max) | 70.0 (42-106) | 76.1 (42-102) | 67.8 (45-106) | |
| Squeezing pressure of HPZ (n=36) | ||||
| Mean ± SD | 129.1 ± 29.2 | 128.5 ± 36.4 | 129.7 ± 21.9 | 0.901 |
| Median (min-max) | 125.4 (67-224) | 115.4 (67-224) | 132.1 (84-170) | |
| Surgical treatment | 32 (76.2) | 13 (68.4) | 19 (82.6) | 0.474 |
| Closed lateral internal sphincterotomy | 2 (4.8) | 1 (5.3) | 1 (4.3) | 1.0004 |
| Botulinum toxin injections | 16 (38.1) | 4 (21.1) | 12 (52.2) | 0.043 |
| Location | 0.604 | |||
| Left | 4 (9.5) | 1 (5.3) | 3 (13.0) | |
| Right anterior | 13 (31.0) | 6 (31.6) | 7 (30.4) | |
| Right posterior | 19 (45.2) | 8 (42.1) | 11 (47.8) | |
| Left, right anterior | 2 (4.8) | 2 (10.5) | 0 (0.0) | |
| Left, right posterior | 2 (4.8) | 2 (10.5) | 0 (0.0) | |
| Right anterior, right posterior | 2 (4.8) | 0 (0.0) | 2 (8.7) | |
| Duration of healing | ||||
| Mean ± SD | 65.6 ± 95.1 | 86.7 ± 114.5 | 48.2 ± 73.6 | 0.092 |
| Median (min-max) | 22.0 (6-437) | 29.0 (6-437) | 19.0 (6-333) |
Note: Data are presented as mean ± SD or number (%), unless otherwise indicated;
1p values were derived from independent t-test;
2p values were derived from Mann-Whitney’s U test;
3p values were derived by chi-square test;
4p values were derived from Fisher’s exact test.
Discussion
CH is a procedure that has been in use since Hippocrates, however it can cause pain, CNHWs [10]. In the 20th century, hemorrhoidectomy such as Milligan-Morgan and Gabriel involved extensive excision of anal tissue, which often led to complications [11,12]. To reduce these complications, Parks, Ferguson, and Takano, have proposed submucosal hemorrhoidectomy, preserving much mucosa followed by suturing the excised anal tissue, or anoderm-preserving hemorrhoidectomy, respectively [13-15]. Our opinion is that the relatively critical aspect of hemorrhoidectomy is the excision of the anoderm which can lead to complications, such as pain, CNHWs, and, in rare cases, stenosis. In 1998, Longo published a study on Stapled Hemorrhoidopexy (SH) for treating grade III and IV hemorrhoids, with the goal of reducing pain while avoiding the excision of the anoderm [16]. However, the American Society of Colon and Rectal Surgeons recommend it as an alternative treatment for fourth-degree hemorrhoids due to the high recurrence rate and the risk of fecal incontinence after SH [17].
CH involves the removal of the perineal skin, the anoderm, and a portion of the lower rectum; however, the anoderm tends to heal less effectively than the other areas. To address this issue, we ligated the hemorrhoidal pile in the rectum with a BC and excised from distal half of the anoderm to outer margin of the external anal sphincter muscle. The redundant proximal half of the anoderm was sutured together with the excised distal wound. The results of the study showed a statistically significant reduction in the risk of CNHWs in the BC+PH group compared to the CH group (8.1% vs. 3.3%). As we previously quoted Goligher, our study also found chronic non-healing wounds only in the distal half of the anoderm [3]. Gender, age, grade of hemorrhoids, and number of hemorrhoidectomy sites may be causes, this study did not show a statistically significant difference. However, this result is likely attributed to the fact that the grade of BC+PH group was lower than that of CH group, resulting in a smaller range of excision. In the proliferative phase of wound healing, collagen formation is based on systemic factors (adequate oxygen supply, nutrients such as amino acids and carbohydrates, and cofactors such as vitamins and trace metals) and local factors such as vascular supply and absence of inflammation, so correcting them is essential for wound healing [1]. Furthermore, it is speculated that another local factor may be that the subcutaneous external anal sphincter muscle, which curves inward toward the center of the anal canal, exerts pressure on the passage of feces. Therefore, in order to reduce the risk of CNHWs, it is recommended to minimize the extent of excision of the anoderm as much as possible. The difference in recurrence rates between the two groups was not statistically significant.
Another complication after hemorrhoidal surgery is DB. DB is characterized by severe rectal bleeding, which has been reported as unpreventable, with an incidence ranging from 2.3% to 4.13% [18,19]. Its causes are known to include local inflammation and fall of hemorrhoidal nodules [18,20,21]. BC was designed to minimize DB. As we published in a previous paper, the frequency of DB was 3.5% with rubber band ligation and 0.0% with BC [8]. The reason for this difference might be the different tightness of ligating materials. After ligation with an elastic rubber band, the soft tissue within the band can serve as a buffer, reducing the possibility of endothelial injury. However, when endothelial injury does occur, tissue factors and underlying collagen are exposed, allowing platelets to adhere to the site of injury and form a platelet plug [22]. Furthermore, vasoconstriction occurs in response to releasing vasoactive substances from platelets (e.g., thromboxane A2 and serotonin) and endothelin from endothelial cells [23-25]. To reduce the incidence of DB after ligation, we hypothesized, based on the aforementioned hemostatic theory, that endothelial injury is crucial for activating the hemostatic sequence at the moment the necrotic hemorrhoidal piles fall. The BC, made of nonabsorbable polymer, is specifically designed to evenly and definitively compress hemorrhoidal soft tissue and the superior hemorrhoidal artery. BC induces necrosis of hemorrhoidal tissue, which then detaches from the rectal wall, similar to a rubber band, approximately one week after application.
As this is a retrospective study conducted at a single institution, the results have inherent limitations. It is therefore recommended that additional studies be undertaken to minimize complications associated with hemorrhoidal surgery.
Conclusion
This retrospective study aimed to compare the incidence of Chronic Non-Healing Wounds (CNHWs) and other complications between two surgical methods for grade III-IV hemorrhoids: Conventional Hemorrhoidectomy (CH) and Partial Hemorrhoidectomy (PH) after BANANA-Clip (BC) ligation. Patients treated with BC+PH exhibited a significantly lower incidence of CNHWs. The BC+PH method effectively removes both internal and external hemorrhoids, and its approach of minimal excision combined with precise suturing promotes better wound healing outcomes.
Acknowledgements
The authors thank Ms. Byeon Tae Joo and Ms. GUI SOON LEE for collecting the medical records, the authors also thank Dr. JIMIN CHOI for conducting the professional statistical analysis.
References
- Brunicardi F, Andersen D, Billiar T, Dunn D, Hunter J, Matthews J, et al. Schwartz's principles of surgery. 10th edn. McGraw-hill; 2014.
- Norman G, Dumville JC, Mohapatra DP, Owens GL, Crosbie EJ. Antibiotics and antiseptics for surgical wounds healing by secondary intention. Cochrane Database Syst Rev 2016;3(3): CD011712.
[Crossref] [Google Scholar] [Pubmed]
- Goligher J. Surgery of the anus rectum and colon. 5th edn. Harcourt College Pub, 1984.
- Barron J. Office ligation of internal hemorrhoids. Am J Surg 1963;105(4):563-570.
[Crossref] [Google Scholar] [Pubmed]
- Barron J, Fallis LS. Non-operative treatment of internal hemorrhoids. Can Med Assoc J 1964;90(15):910.
[Google Scholar] [Pubmed]
- Iyer VS, Shrier I, Gordon PH. Long-term outcome of rubber band ligation for symptomatic primary and recurrent internal hemorrhoids. Dis Colon Rectum 2004;47:1364-1370.
[Crossref] [Google Scholar] [Pubmed]
- Bleday R, Pena JP, Rothenberger DA, Goldberg SM, Buls JG. Symptomatic hemorrhoids: Current incidence and complications of operative therapy. Dis Colon Rectum 1992;35(5):477-481.
[Crossref] [Google Scholar] [Pubmed]
- Kang DW, Kim BS, Kim JH, Kim KR, Kang GS. A comparative study of rubber band ligation versus BANANA-Clip in grade 1 to 3 internal hemorrhoids. Annals of Coloproctology. 2023;39(1):41.
[Crossref] [Google Scholar] [Pubmed]
- Gould L, Li WW. Defining complete wound closure: Closing the gap in clinical trials and practice. Wound Repair Regen 2019;27(3):201-224.
[Crossref] [Google Scholar] [Pubmed]
- Pata F, Gallo G, Pellino G, Vigorita V, Podda M, Di Saverio S, et al. Evolution of surgical management of hemorrhoidal disease: An historical overview. Front Surg 2021;8:727059.
[Crossref] [Google Scholar] [Pubmed]
- Milligan ET, Morgan CN, Jones L, Officer R. Surgical anatomy of the anal canal, and the operative treatment of haemorrhoids. The Lancet 1937;230(5959):1119-1124.
- Gabriel WB. The Principles and Practice of Rectal Surgery. 4th edn. London, 1948.
- Parks AG. The surgical treatment of haemorrhoids. Br J Surg 1956;43(180):337-351.
[Crossref] [Google Scholar] [Pubmed]
- Ferguson JA, Heaton RJ. Closed hemorrhoidectomy. Dis Colon Rectum 1959;2(2):176-179.
[Crossref] [Google Scholar] [Pubmed]
- Takano M. Anoderm-preserving hemorrhoidectomy. Dis Colon Rectum 1980;23(8):544-549.
[Crossref] [Google Scholar] [Pubmed]
- Longo A. Treatment of hemorrhoid disease by reduction of mucosa and hemorrhoidal prolapse with a circular suturing device: A new procedure.. Proceedings world congress endoscop surg 1998.
- Hawkins AT, Davis BR, Bhama AR, Fang SH, Dawes AJ, Feingold DL, et al. The American society of colon and rectal surgeons clinical practice guidelines for the management of hemorrhoids. Dis Colon Rectum 2024;67(5):614-623.
[Crossref] [Google Scholar] [Pubmed]
- El Nakeeb AM, Fikry AA, Omar WH, Fouda EM, El Metwally TA, Ghazy HE, et al. Rubber band ligation for 750 cases of symptomatic hemorrhoids out of 2200 cases. World J Gastroenterol 2008;14(42):6525.
[Crossref] [Google Scholar] [Pubmed]
- Komborozos VA, Skrekas GJ, Pissiotis CA. Rubber band ligation of symptomatic internal hemorrhoids: Results of 500 cases. Dig Surg 2000;17(1):71-76.
[Crossref] [Google Scholar] [Pubmed]
- Hwang DY, Kim YJ, Chung JE, Lee JH, Chang HC, Rhu JH, et al. Analysis of factors influencing secondary bleeding after hemorrhoidectomy. J Korean Soc Coloproctol 2002;18(6):369-372.
- Kunitake H, Poylin V. Complications following anorectal surgery. Clin Colon Rectal Surg 2016;29(01):14-21.
[Crossref] [Google Scholar] [Pubmed]
- Gale AJ. Continuing education course #2: Current understanding of hemostasis. Toxicol Pathol 2011;39(1):273-280.
[Crossref] [Google Scholar] [Pubmed]
- Rucker D, Dhamoon AS. Physiology, thromboxane A2. StatPearls, 2024.
- Frishman WH, Grewall P. Serotonin and the heart. Ann Med 2000;32(3):195-209.
[Crossref] [Google Scholar] [Pubmed]
- Titus A, Marappa-Ganeshan R. Physiolology, endothelin. StatPealrs, 2024.