Research Article - Archives of Clinical and Experimental Surgery (2024)
A Prospective and Comparative Study between Preoperative Intravenous Prophylactic Antibiotic and Intra-Incisional Prophylactic Antibiotic with Ceftriaxone to Reduce Surgical Site Infection
Narayana V, Chandrashekar D*, V Om Pramod Kumar Raja, Koripalli Srija and Megha Kiran GSNarayana V, Chandrashekar D, Department of General Surgery, Vydehi Insitute of Medical Sciences and Research Centre, Bangalore, India, Email: drchandrashekar9@gmail.com
Received: 05-Sep-2024, Manuscript No. EJMACES-24-147371; Editor assigned: 09-Sep-2024, Pre QC No. EJMACES-24-147371 (PQ); Reviewed: 23-Sep-2024, QC No. EJMACES-24-147371; Revised: 30-Sep-2024, Manuscript No. EJMACES-24-147371 (R); Published: 07-Oct-2024
Abstract
Introduction: SSI (Surgical Site Infection) is accounts for 20% of all hospital acquired infections among surgical patients, and are associated with substantial healthcare costs, patient inconvenience and dissatisfaction. Risks factors for SSI are multifactorial which can originate from patient, operative procedure or causative organisms. Initially, the antibiotics were administered post-operatively for treatment of already established SSI. Later the concept of ceftriaxone antibiotic prophylaxis was introduced intraincisional and pre-operative intravenous route. After administration of Intra Venous (IV) antibiotics, it is distribute in systemic pool and into the peripheral pool, which results in low concentration of antibiotic at the site of wound healing. Intra-incisional infiltration of antibiotic, ensures high concentration of antibiotic at the incision site and thus it present in high concentration during the time of healing of the operative wound.
Methods: Source of data-All patients undergoing elective and clean abdominal surgeries in the Department of General Surgery at Vydehi Institute of Medical Sciences and Research Centre, Bengaluru during the period of July 2022 to June 2024. Data was collected from the “Case proforma” pertaining to patient’s particulars, history, clinical examination, investigation, diagnosis and surgical procedures.
Results: Results of this includes Gender distribution, Surgical site infection, Duration of surgery, Organisms isolated by culture, Clean, clean contaminated and contaminated cases in each group, Categories of SSI in each group, Day of occurrence of SSI in each group, SSI develops among diabetes mellitus patients which were clearly mentioned in results section.
Conclusion: This study confirms that the preoperative intra-incisional infiltration of Ceftriaxone has resulted in a significant reduction in SSI rates, which makes a better mode of administration of prophylactic antibiotics.
Keywords
Surgical Site Infection (SSI); Intravenous Administration (IVA); Intra-Incisional Infiltration (III); Intra Dermal Test Dose (IDTD); Pre- Operative Test Dose (POTD)
Introduction
Surgical site infection is defined as infection that occurs at or near the surgical incision, within 30 days after surgery or within one year, if an implant is left in place and affecting planes either superficial, deep or organs space. SSI is accounts for 20% of all hospital acquired infections among surgical patients and are associated with substantial healthcare costs, patient inconvenience and dissatisfaction. Risks factors for SSI are multifactorial which can originate from patient, operative procedure or causative organisms Initially, the antibiotics was administered post-operatively for the treatment of already established SSI. Later the concept of ceftriaxone antibiotic prophylaxis was introduced intra-incisional and pre-operative intravenous route After administration of Intra Venous (IV) antibiotics, it is distributed in systemic pool and into the peripheral pool which results in low concentration of antibiotic at the site wound healing. Intra-incisional infiltration of antibiotic ensures high concentration of antibiotic at the incision site and thus it is present in high concentration during the time of healing of the operative wound.
SSI were categorized into 3 types shown in Figure 1.
1. Superficial incisional site infection
2. Deep incisional site infection
3. Organ space infection
Benefits of subcutaneous administration of antibiotics
• High and sustained concentration at the site of healing
• Limited potential for absorption into systemic circulation
• Half-life of 6-8 h
• Least chance of development of resistance and toxicity
• Minimal adverse effects.
• No first pass metabolism
Aims and objectives
• The aim of the study is to compare the efficacy of pre-operative antibiotic infiltration at the incision site with that of pre-operative intravenous antibiotics in reducing surgical site infections.
• To assess the advantage of intra-incisional antibiotic therapy over intravenous antibiotic therapy.
Materials and Methods
All patients undergoing elective and clean abdominal surgeries in the Department of General Surgery at Vydehi Institute of Medical Sciences and Research Centre, during the period of July 2022 to Jun 2024.
Inclusion criteria and exclusion criteria
Inclusion criteria and exclusion criteria is shown in Table 1.
| Inclusion criteria | Exclusion criteria |
|---|---|
| • Patients of both sexes | • Patients allergic to Ceftriaxone after test dose. |
| • Patients of age more than 18 years. | • All laparoscopic surgeries, because of its small port wound |
| • Patients undergoing elective and clean abdominal surgeries | |
| • Patients who were willing for participation in the study after giving informed consent |
Procedure for collection of data
Data was collected on a “Case proforma” which includes:
• Patient’s particulars
• History taking
• Clinical examination
• Investigations
• Surgical procedure
• Surgical site infection
• Outcome of the study
Prospective and comparative study
Patients randomized into two groups of 50 each.
Group A: Received single dose of intravenous ceftriaxone (1 g)
Group B: Received intra-incisional ceftriaxone (1 g) in subcutaneous plane.
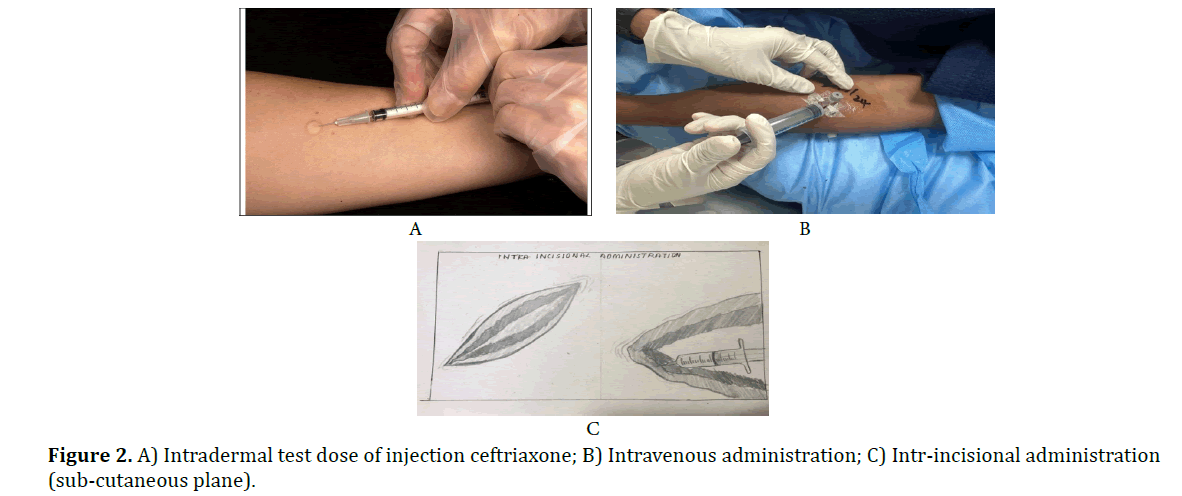
One day prior to the surgery, test dose of ceftriaxone given intradermally to exclude hypersensitivity reactions to all 100 patients in both the groups under Group A and Group B. Intradermal test dose of injection. Ceftriaxone-All 100 patients underwent test dose for Ceftriaxone. None of the patients developed allergy to the intradermal test dose for Ceftriaxone (Figure 2A). Intravenous injection given to 50 patients (Group A) 1 g (Figure 2B). Intraincisional injection given to 50 patients (Group B) at subcutaneous plane during surgery (Figure 2C).
Results
Results of this study shown in below.
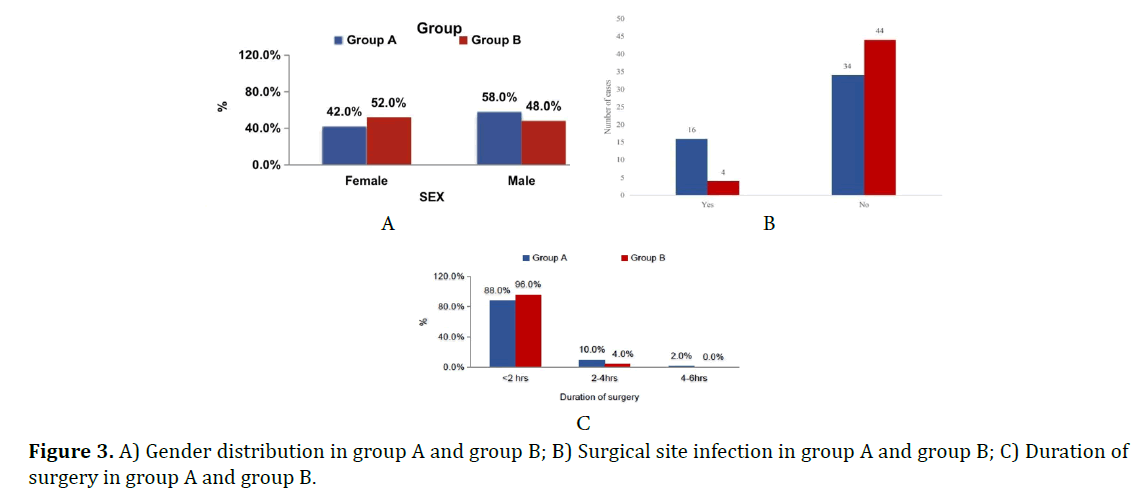
1. Gender distribution (Table 2 and Figure 3A)
Table and bar graph showing distribution of male and female patients. Group A there were 21 (42%)female and 29 (58%) male patients. Group B there were 26 (47%) female and 24 (53%) male patients with p value of 0.423.
| Gender distribution | ||||
|---|---|---|---|---|
| Sex | Group A | Group B | Total | p-value |
| Female | 21(42%) | 26(47%) | 47(47%) | 0.42 |
| Male | 29(58%) | 24(53%) | 53(53%) | |
| Total | 50 | 50 | ||
| Surgical site infection | ||||
| SSI | Group A | Group B | Total | p-value |
| Yes | 16(32%) | 4(8%) | 20 | 0.005 |
| No | 34(68%) | 46(92%) | 80 | |
| 50 | 50 | 100 | ||
| Duration of surgery | ||||
| Duration | Group A | Group B | Total | p-value |
| <2hrs | 44(88%) | 48(96%) | 48(96%) | 0.486 |
| 2-4hrs | 5(10%) | 2(4%) | 7(7%) | |
| 4-6hrs | 1(2%) | 0(0%) | 1(1%) | |
| 50 | 50 | 100 | ||
2. Surgical site infection (Table 2 and Figure 3B)
Table and bar graph showing distribution of SSI development between Group A and Group B. Under Group A there were 16 (32%) patients out of 50 patients developed SSI. Under Group B there were only 4 (8%) patients developed SSI among 50 patients with p value of 0.005.
3. Duration of surgery (Table 2 and Figure 3C)
Table and bar graph showing duration of surgery among group A and group B. In group A, duration of surgery for 44 (88%) patiens was <2 h, for 5 (10%) patients duration was 2-4 h, for 1 (2%) patient it was 4-6 h. In group B, duration of surgery for 48 (96%) patiens was <2 h, for 2 (4%) patients duration was 2-4 h, for none of the patients it was 4-6 h. p value of 0.486.
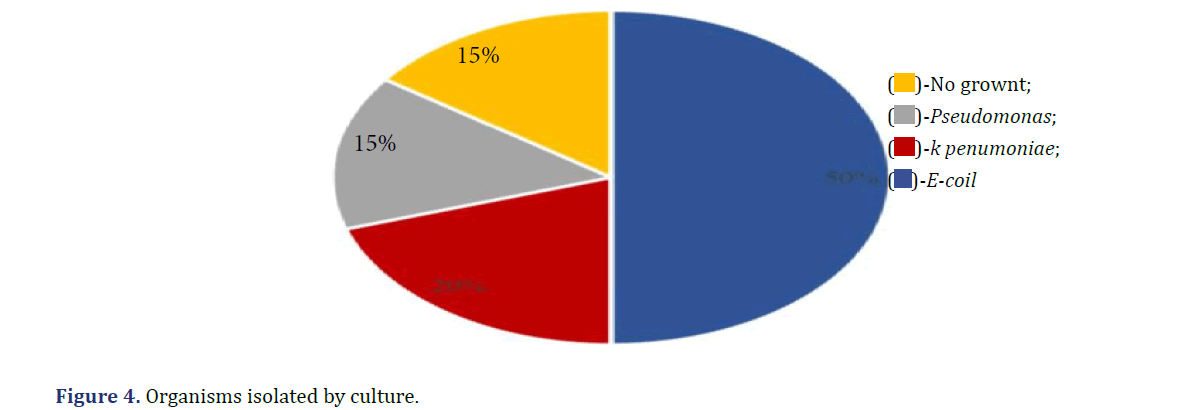
4. Organisms isolated by culture (Table 3 and Figure 4)
| Organism | Group A | Group B | Total |
|---|---|---|---|
| E-coil | 8(50%) | 2(50%) | 10(50%) |
| Klebsiella pneumonia | 4(25%) | 0 | 4(20%) |
| Pseudomonas | 3(18.75%) | 0 | 3(15%) |
| No growth | 1(6.25%) | 2(50%) | 3(15%) |
| 2(50%) | 2(50%) | 20(100%) |
Table and pie chart showing different organisms that caused SSI among Group A and Group B. In group A, 8 (50%) patients showed the infective organism E.coli, 4 (25%) patients showed Klebsiella pneumonia, 3 (18.75%)patients showed Pseudomonas species, no growth was seen in 1 (6.25%) out of 16 patients. In group B, 2 (50%) patients showed the infective organism E.coli, none of the patients showed Klebsiella pneumonia, none of the patients showed Pseudomonas species, no growth was seen in 2 (50%) out of 4 patients.
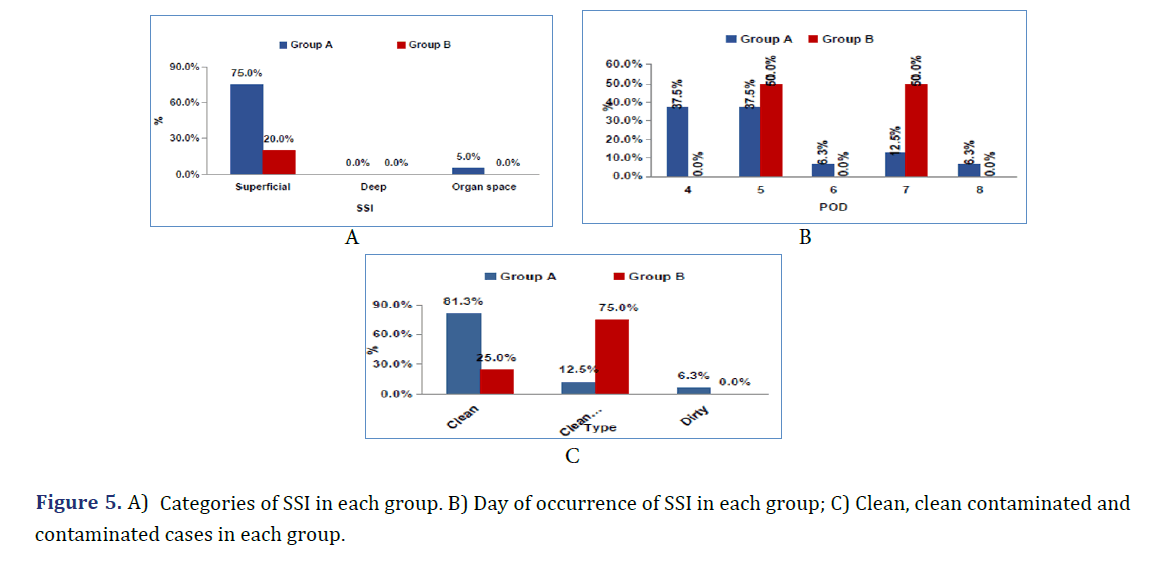
5. Clean, clean contaminated and contaminated cases in each group (Table 4 and Figure 5A)
| Clean, clean contaminated and contaminated cases | ||||
|---|---|---|---|---|
| Group A | Group B | p-value | ||
| Clean | 13(81.3%) | 1(25%) | 0.012 | |
| Clean contaminated | 2(12.5%) | 3(75%) | 0.009 | |
| Contaminated | 1(6.3%) | 0(0%) | ||
| 16 | 4 | |||
| Categories of SSI | ||||
| SSI | Group A | Group B | Total | p-value |
| Superficial | 15(75%) | 4(20%) | 19(25%) | 0.025 |
| Deep | 0 | 0 | 0 | 0.009 |
| Organ space | 1(5%) | 0(0%) | 1(5%) | |
| 16(80%) | 4(20%) | 20(100%) | ||
Table and bar diagram reveals Clean, clean contaminated and contaminated in each group. In Group A, 13 (81.3%) patients had clean wound, 2 (12.5%) patients had clean contaminated wound and 1 (6.3%) patient had contaminated wound out of 16 patients. In Group B, 1 (25%) patient had clean wound, 3 (75%) patients had clean contaminated wound and none of patients had contaminated wound out of 4 patients.
6. Categories of SSI in each group (Table 4 and Figure 5B)
Table and bar diagram showing the category of SSI in both the groups. In group A, 15 (75%)patients had superficial wound SSI. none of the patients had deep wounds SSI, 1 (5%) patient had wound in the organ space SSI out of 16 patients. In group B, 4 (20%) patients had superficial wound SSI, none of the patients had deep wound SSI, 1 (5%)patient had wound in the organ space SSI out of 4 patients. p value of 0.0025.
7. Day of occurrence of SSI in each group (Table 5 and Figure 5C)
| POD | Group A | Group B | Total |
|---|---|---|---|
| 4 | 6(37.5%) | 0(0%) | 6(30%) |
| 5 | 6(37.5%) | 2(50%) | 8(40%) |
| 6 | 1(6.25%) | 0(0%) | 1(5%) |
| 7 | 2(12.5%) | 2(50%) | 4(20%) |
| 8 | 1(6.25%) | 0(0%) | 1(5%) |
| 16(100%) | 4(100%) | 20(100%) |
Table and bar diagram showing the day of occurrence of SSI. In group A, 6 (37.5%) patients had SSI on POD 4, 6 (37.5%) patients had SSI on POD 5, 1 (6.25%) patient had SSI on POD 6, 2 (12.5%)patients had SSI on POD 7 and 1 (6.25%) patient had SSI on POD 8 out of 16 patients. In group B, none of the patients had SSI on POD 4, 2 (50%) patients had SSI on POD 5, none of the patients had SSI on POD 6, 2 (50%)patients had SSI on POD 7 and none of the patients had SSI on POD 8 out of 4 patients.
8. SSI among diabetes mellitus patients (Table 6)
| DM (Diabetes Mellitus) | Group A | Group B | p-value |
|---|---|---|---|
| Yes | 03(18.75%) | 0(0%) | 0.89 |
| No | 13(81.25%) | 4(100%) | |
| 16(100%) | 4(100%) |
Among the 100 patients included in the study, 16 in the Group A and 4 in Group B were diabetic. In Group A, only 3 (18.75%) among the 16 who developed SSI were diabetics and no SSI were noted in diabetic patients of Group B. No association was found between Diabetes and the occurrence of SSI in this study as the p value is 0.89 which is not statistically significant.
Discussion
In this study, Under Group A there were 21 female and 29 male patients out of 50 patients and under Group B there were 26 female and 24 male patients out of 50 patients. Regarding development of SSI between Group A and Group B. Group A there were 16 patients out of 50 patients developed SSI. Group B there were only 4 patients developed SSI among 50 patients. p value of 0.005. Regarding duration of surgery among Group A and Group B, In Group A, duration of surgery for 44 patiens was <2 h, for 5 patients duration was 2-4 h, for 1 patient it was 4-6 h. In Group B, duration of surgery for 48 patiens was <2 h for 2 patients duration was 2-4 h, for none of the patients it was 4-6 h. Duration of the surgery in majority of cases is less than 2 h. There is no association with SSI in relation to duration of surgery. The organisms responsible for SSI, Group A are, 8 patients showed the infective organism E.coli, 4 patients showed Klebsiella pneumonia, 3 patients showed Pseudomonas species, no growth was seen in 1 patient. Group B, 2 patients showed the infective organism E.coli, none of the patients showed Klebsiella pneumonia, none of the patients showed Pseudomonas species, no growth was seen in 2 patients. Most common organism isolated on culture was E. coli (50%), followed by Klebsiella pneumonia and Pseudomonas species. Regarding development of SSI among clean, clean contaminated and contaminated wounds, Group A, 13 patients had clean wound, 2 patients had clean contaminated wound and 1 patient had contaminated wound. Group B, 1 patient had clean wound, 3 patients had clean contaminated wound and none of patients had contaminated wound. Regarding categories of wounds which developed SSI with p value 0.025. Group A, patients had superficial wound s, none of the patients had deep wounds, 1 patient had wound in the organ space. Group B, 19 patients had superficial wound s, none of the patients had deep wounds, 1 patient had wound in the organ space. Regarding SSI development during post of period, In Group A, 6 patients had SSI on POD 4, 6 patients had SSI on POD 5,1 patient had SSI on POD 6, 2 patients had SSI on POD 7 and 1 patient had SSI on POD 8. Group B, none of the patients had SSI on POD 4, 2 patients had SSI on POD 5, none of the patients had SSI on POD 6, 2 patients had SSI on POD 7 and none of the patients had SSI on POD 8. More number of SSI were noted on post-operative day 5, with the earliest SSI being noted on post-operative day 4. Among the 100 patients, 16 in the Group A and 4 in Group B were diabetic patients. Group A only 3 among the 16 who developed SSI. Group B none developed SSI. No co-relation was found between the incidence of SSI and diabetes in this study. The p value is 0.89 which is not statistically significant.
The advantage of using intra-incisional antibiotic prophylaxis are multiple. Since the medicine is delivered locally only into the dermal and subcutaneous layers, only a tiny amount enters the systemic circulation, thereby decreasing the chances of developing antibiotic resistance and drug interaction with other systemic medications and prevent disruption of the intestinal microbiome. The incidence of SSI is gradually being employed as an outcome and surrogate measure for assessing the quality of surgical care. Although SSI is an interplay of modifiable and non-modifiable factors, incorporated evidence-based practice will go a long way in improving patient care and reducing mortality and morbidity [1]. Surgical site infection is very distressing problem. This study confirms that the preoperative intra-incisional injection of a broad spectrum antibiotic (Ceftriaxone) has resulted in a significant reduction in SSI infection rate in all class of wounds [2]. The evolution of intra-incisional antibiotic prophylaxis represents a potential frontier in MOHS surgery, offering a target and localized approach to infection prevention [3]. A study comparing preoperative antibiotic infiltration along the incision site and prophylactic intravenous antibiotic administration for reducing surgical site infection demonstrated that SSI infection rates have decreased in all classes of wounds following preoperative intravenous with an intra-incisional injection of a broad spectrum antibiotic (Ceftriaxone).The intra-incisional approach theoretically achieves larger concentration at the incision site, making it a better method of preventive antibiotic administration [4]. Preoperative intra-incisional antibiotic reduces the rate of SSI in all wound classes. The higher concentration achieved at the incision site by intra-incisional route theoretically makes it a better mode of administering prophylactic antibiotics [5]. Preoperative intra-incisional antibiotics significantly reduces the rate of SSI because of the higher concentration achieved at the incision site and theoretically makes it a better mode of administering [6]. In the present study, there was significant reduction in incidence of SSI in the group, which received preoperative single dose intra-incisonal Ceftriaxone than the other group which received only preoperative intravenous Ceftriaxone. Preoperative intra-incisional antibiotics significantly reduce the rate of SSI because of the higher concentration achieved at the incisional site [7]. In our study, there was a significant reduction in the incidence of SSI in the group, which received both intra-incisionally and intravenous Ceftriaxone preoperatively than the other group which received only intravenous Ceftriaxone. Preoperative intraincisional antibiotics significantly reduced the rate of SSI because of the higher concentration achieved at the incision site [8].
Conclusion
The present study clearly reveals that out of 20 patients who were developed SSI, 16 patients were control group (Group A) who took intravenous preoperative Ceftriaxone and 4 patients are effective Group (Group B) who took intraincisional injection of Ceftriaxone. This results confirmed that the preoperative intraincisional injection of Ceftriaxone has resulted in a significant reduction in SSI. This is because of high concentration of Ceftriaxone at the site of incision which reduce the rate of SSI.
References
- Sophy FJ, Devi RL, Sagayam S, Rohit R. Pre-operative intra-incisional antibiotic infiltration and prophylactic intravenous antibiotic administration for reducing surgical site infection. Int J Acad Med Pharm 2023;5(4):1024-1028.
- Singh A, Salim M, Singh B. A comparative study of preoperative intra-incisional infiltration of ceftriaxone vs. intravenous ceftriaxone for prevention of surgical site infections. Int Surg J 2019;6(5):1686-1692.
- Mukarram M, Rizzo D, Frasier K, Beard A. Optimizing infection prevention in mohs procedures: Efficacy of intra-incisional antibiotic prophylaxis and future research directions. Ameri J Clin Med Re 2024 136:1-6.
- Kumar MS, Balraj G, Sivasankaran. A study comparing preoperative antibiotic infiltration along the incision site and prophylactic intravenous antibiotic administration for reducing surgical site infection. Int J Acad Med Pharm 2023;5(6);46-51.
- Anand S, Batra R, Arora B, Atwal S, Dahiya RS. A comparative study of preoperative intra-incisional infiltration of ceftriaxone vs. intravenous ceftriaxone for prevention of surgical site infections in emergency cases. J Evolution Med Dent Sci 2016;5(64):4537-4531.
- Dogra BB, Kalyan S, Rana KV, Panchabhai S, Kharade K, Priyadarshi S. A study comparing preoperative intra-incisional antibiotic infiltration and prophylactic intravenous antibiotic administration for reducing surgical site infection. Med J Dr. DY Patil University 2013;6(4):405-409.
- Pravindhas A, Navaneetha K, Raja AA, Lakshmana R, Paul NK. Preoperative single dose intraincisional vs. intravenous ceftriaxone in preventing surgical site infection post-hernioplasty conducted at a tertiary care centre at Chengalpattu, Tamil Nadu, India. J Clin Diagn Res 2023;17(5):PF01-PF06.
- Sivachandran K. An experimental study comparing preoperative intra incisional antibiotic infiltration and prophylactic intravenous antibiotic administration for reducing surgical site infection in laparotomy surgeries. Int J Pharma Clin Res 2022;14(7);902-910.