Research Article - Archives of Clinical and Experimental Surgery (2022)
A Prospective and Comparative Study on Fistulotomy with Sphincteroplasty or Fistulotomy without Sphincheteroplasty of Partially Damaged Internal Sphincter and Assessment of Incontinence, Recurrence and Patient Satisfaction in the Patient of High Fistula-in-Ano
Sarvagya Jain, Department of Surgery, Mahatma Gandhi Memorial Medical College, Indore, Madhya Pradesh, India, Email: sarvagyajain25@gmail.com
Received: 11-Jan-2022, Manuscript No. EJMACES-22-51195; Editor assigned: 13-Jan-2022, Pre QC No. EJMACES-22-51195 (PQ); Reviewed: 27-Jan-2022, QC No. EJMACES-22-51195; Revised: 01-Feb-2022, Manuscript No. EJMACES-22-51195 (R); Published: 08-Feb-2022
Abstract
Introduction: Surgery is the only mainstay treatment for fistula-in-ano. Fistula-in-ano is known to human for more than 2000 years, but still the surgical treatment remains challenging, due to differences in success, reoccurrence rates and incontinence risks. Till date, fistulotomy procedures is known as the gold standered surgical treatment, with a perfect surgical field view and allowing direct access to the source of inflammation The aim of this prospective study is to evaluate the safety and long-term efficacy of Fistulotomy with end to end primary sphincteroplasty and to assess its impact on patients’ postoperative continence status, recurrence, wound and satisfaction. Materials and methods: N=35 in both the groups (Fistulotomy with sphincteroplasty group and Fistulotomy without sphincteroplasty group) inclusion criteria the patients who of fistula-in-ano with probable etiology of cryptoglandular theory. Result and discussion: Incontinence was seen in 9 (25.7%) patients in fistulotomy group and 2 (5.7%) patients in fistulotomy with sphincterotomy group. Recurrence was seen in 12 (34.3%) patients in fistulotomy group and 4 (11.4%) patients in fistulotomy with sphincterotomy group. Wound infection was seen in 16 (45.7%) patients in fistulotomy group and 7 (20%) patients in fistulotomy with sphincterotomy group. The mean satisfaction score in fistulotomy group was 7.06 ± 0.54 and in fistulotomy with sphincterotomy group was 8.26 ± 0.61. Conclusion: The total outcomes for the patient with fistula-in-ano, which have undergone fistulotomy with sphincteroplasty, the outcomes are much better in terms of recurrence, incontinence; post op wound infection and patient satisfaction.
Keywords
Patient satisfaction; Wound infection; Incontinence; Fistulotomy with primary sphincteroplasty; High fistula-in-ano
Introduction
Fistula-in-ano (anal fistula) in simple language can be described as a connection (a granulomatous tract) between an internal opening in the anal canal and an external opening (single or multiple) in skin through which an abscess has drained. Fistula-in-ano has been regarded as chronic form of the suppurative process of ano rectal infection [1]. Surgery is the only mainstay treatment for fistula-in-ano. Fistula-in-ano is known to human for more than 2000 years, but still the surgical treatment remains challenging, due to differences in success, reoccurrence rates and incontinence risks. Till date, fistulotomy procedures are known as the gold standered surgical treatment, with a perfect surgical field view and allowing direct access to the source of inflammation [2]. Today, in the world of researches and inventions, with the help of better knowledge of anorectal anatomy, pathology and techniques, limitless surgeries are done and newer methods of treatment for fistula-in-ano are coming. Commonly done surgical procedures for fistula-in-ano are Fistulectomy, fistulotomy, over-the scope-clip (OTSC), Trans anal opening of inter-sphincteric space (TROPIS), stem cell, filac laser, Ligation of inter-sphincteric fistula tract (LIFT), Video assisted anal fistula treatment (VAAFT), fibrin glue, advancement flap, fistula plug, seton insertion(draining and cutting),sphincter repair surgeries like fistulotomy or fistulectomy with sphincteroplasty [3]. Parkash et al, in 1985, proposed a technique of fistulotomy with end to end primary sphincteroplasty (FIPS) for complex anal fistula. But this technique has always been regarded with untrust, mainly due to the lack of scientific evidence on the risk of postoperative fecal continence impairment. Now, again interest of surgeons in FIPS is gradually increasing [4]. In high fistula-in-ano, due to fear of sphincter injury, there is incomplete drainage of abscess by surgeons that lead to reoccurrence of fistula-in-ano [5]. FIPS will help surgeon to drain the abscess completely, so that there will be minimum risk of recurrence of fistula-in-ano and patient will be more satisfied. Disadvantages of fisulotomy with primary sphinceteroplasty, are long hospital stay and a large wound. But with proper care, wound can be completely healed and patient can be completely cured with fistula-in-ano. The aim of this prospective study is to evaluate the safety and long-term efficacy of Fistulotomy with end to end primary sphincteroplasty and to assess its impact on patients’ postoperative continence status, recurrence, wound and satisfaction [6].
Materials and Methods
Sources of data
All patients with high anal fistula are coming to Department of General Surgery in M.Y. Hospital, Indore (M.P).
Study design
Prospective, non-randomized and interventional study
Study population
All Patients with Fistula-in-ano cases
Study period
March 2020 to February 2021
Place of study
M.Y. Hospital, Indore (M.P)
Sample size
Total=70 patients
N=35 in both the groups (Fistulotomy with sphincteroplasty group and Fistulotomy without sphincteroplasty group) [7].
Inclusion criteria
The patients who are clinically diagnosed as high fistula- in-ano in all ages and both Sex, with probable etiology of cryptoglandular theory who are subjected to relevant investigation and undergo surgery were be included [8].
Exclusion criteria
1. Patient refusal
2. Anal fistulae may be found in association with specific
conditions such as
a. Crohn’s disease
b. Tuberculosis
c. Lymphogranuloma Venereum
d. Actinomycosis
e. Rectal Duplication
f. Foreign Body
g. Malignancy
h. Recurrence
Methodology
This prospective clinical comparative study which was carried out on 70 patients, in which 35 pateints had gone through technique as fistulotomy with sphincteroplasty and rest 35 patients undergone fistulotomy without sphincteroplasty in the patient of high anal fistula Department of General Surgery M.Y. Hospital, Indore, M.P, between March 2020 and February 2021. The study was approved by the local ethics committee. All patients were informed about the other surgical techniques, their results, and complications for the treatment of perianal fistulas. The sphincter was repaired by absorbable suture Vicryl 3-0 and fistulotomy was done as usual [9]. The possible outcomes and complications were explained to all patients. All patients who were included in study had no complained of any degree of faecal incontinence. A watchful physical examination is done for the diagnosis of anal fistulas in each patient. A day before surgery, each one of patients was given bowel preparation regimen, using Polyethylene glycol and enema on the day of surgery. Intravenous prophylaxis with antibiotics (i.v.ceftriaxone with sulbactum, 1.5 gm and i.v metronidazole 100 ml) was administered to all patients before surgery. To identify external and internal fistulous opening and tract, examination done under Spinal anaesthesia and the fistula lithotomy (extended lithotomy) position were used. The fistula tract was probed gently, cannulated and cleaned with gauze in to remove the epithelial lining. Distance of external and internal openings were measured using sterile scale. The tract was curetted and the granulation tissue was removed [10]. Length of fistula tract was measured. Sphincter was cut to completely remove the fistulous tract and repaired with vicryl 3-0 in a single layer. Anal opening was packed with a roller pack soaked in Sucralfate, povidine-iodine and metronidazole. Pack was removed on next day. His postoperative oral intake was restricted for 12 hours. Liquid diet was allowed after 12 hours gradually to regular diet. Patients received prophylactic doses of oral ciprofloxacin and metronidazole for next seven days and were instructed to apply topical ointment of Metrogyl-P to the external wound daily for seven days. Moreover, pain medication (eg. Paracetamol) was prescribed as required. Patients were instructed to do sitz bath daily four times a day for 7 days. Patients were compared on the platform of recurrence incontinence, wound infection and satisfaction (out of 10) [11].
In both the groups the incidence of wound infection was very high at 15 days follow-up, which gradually reduced in both the groups and by 180 days, only 1 patient in fistulotomy group had wound infection. At all the follow-up, the proportional comparison of wound infection was found to be statistically not significant (P>0.05), showing a comparable proportional complications between the two groups at all the follow-ups [12].
Observation and Results
Wound infection
At 15 days: The incidence of wound infection in fistulotomy group was 13 (37.1%) and in fistulotomy with sphincteroplasty group was 10 (28.6%). The incidence of wound infection was comparable between the two groups (P=0.611).
At 30 days: The incidence of wound infection in fistulotomy group was 9 (25.7%) and in fistulotomy with sphincteroplasty group was 5 (14.3%). The incidence of wound infection was comparable between the two groups (P=0.371).
At 45 days: The incidence of wound infection in fistulotomy group was 8 (22.9%) and in fistulotomy with sphincteroplasty group was 4 (11.4%). The incidence of wound infection was comparable between the two groups (P=0.342).
At 60 days: The incidence of wound infection in fistulotomy group was 7 (20%) and in fistulotomy with sphincteroplasty group was 2 (5.7%). The incidence of wound infection was comparable between the two groups (P=0.151).
At 90 days: The incidence of wound infection in fistulotomy group was 4 (11.4%) and in fistulotomy with sphincteroplasty group was 1 (2.9%). The incidence of wound infection was comparable between the two groups (P=0.356).
At 180 days: The incidence of wound infection in fistulotomy group was 1 (2.9%) and in fistulotomy with sphincteroplasty group was 0 (0.0%). The incidence of wound infection was comparable between the two groups (P=1.000).
In both the groups the incidence of wound infection was very high at 15 days follow-up, which gradually reduced in both the groups and by 180 days, only 1 patient in fistulotomy group had wound infection. At all the follow-up, the proportional comparison of wound infection was found to be statistically not significant (P>0.05), showing a comparable proportional complications between the two groups at all the follow-ups (Table 1).
| Postoperative complications | Group | Fisher’s exact p value | |
| Fistulotomy Group | Fistulotomy with sphincteroplasty group (n=35) | ||
|
Wound infection |
16 | 7 | P=0.041* |
| 45.70% | 20.00% | ||
|
Incontinence |
9 | 2 | P=0.045* |
| 25.70% | 5.70% | ||
|
Recurrence |
12 | 4 | P=0.044* |
| 34.30% | 11.40% | ||
|
Note: Fisher’s Exact Test applied. P value<0.05 was taken as statistically significant. |
|||
Wound infection
It was seen in 16 (45.7%) patients in fistulotomy group and 7 (20%) patients in fistulotomy with sphincteroplasty group. The wound infection rate was significantly higher fistulotomy group in comparison to fistulotomy with sphincteroplasty group (P=0.041).
Incontinence
It was seen in 9 (25.7%) patients in fistulotomy group and 2 (5.7%) patients in fistulotomy with sphincteroplasty group. The incontinence rate was significantly higher fistulotomy group in comparison to fistulotomy with sphincteroplasty group (P=0.045).
Recurrence
It was seen in 12 (34.3%) patients in fistulotomy group and 4 (11.4%) patients in fistulotomy with sphincteroplasty group. The recurrence rate was significantly higher fistulotomy group in comparison to fistulotomy with sphincteroplasty group (P=0.044).
All the postoperative complications were significantly more in fistulotomy group compared to fistulotomy with sphincteroplasty group.
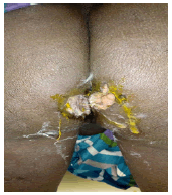
The mean satisfaction score (out of 10) in fistulotomy group was 7.06 ± 0.54 and in fistulotomy with sphincteroplasty group was 8.26 ± 0.61. The mean satisfaction score was significantly higher in fistulotomy with sphincteroplasty group in comparison to the fistulotomy group (P=0.001) (Figure 1-3).
Discussion
Fistula-in-ano is a very common disease among population, patient suffers a lot and there is a social stigma of it. Surgeons are trying from last 700 years for the effective treatment of fistula, but still the best treatment option remains the mystery [13]. In high fistula-in-ano if we go for simple fistulotomy then, we have to cut the anal sphincter which will result in post operative incontinence. If to prevent the incontinence, anal sphincters will not be damaged and improper drainage of the abscess and removal of fistula will lead to recurrence, forcing the patient to come to hospital again and again [14]. After the technique of Fistulotomy with primary sphincteroplasty by Prakesh 1985, high fistula-in-ano was reconsidered and fistulotomy was done with proper cutting of anal sphincters and again anal sphincters were repaired [15]. There were lower rates of recurrence, incontinence, post op wound infection and increased patient satisfaction. In our study on 70 patients, 35 patients were operated with fistulotomy and 35 with fistulotomy with sphincteroplasty were done [16]. The final results were:
Incontinence
It was seen in 9 (25.7%) patients in fistulotomy group and 2 (5.7%) patients in fistulotomy with sphincterotomy group. The incontinence rate was significantly higher fistulotomy group in comparison to fistulotomy with sphincterotomy group.
Recurrence
It was seen in 12 (34.3%) patients in fistulotomy group and 4 (11.4%) patients in fistulotomy with sphincterotomy group. The recurrence rate was significantly higher fistulotomy group in comparison to fistulotomy with sphincterotomy group.
Wound infection
It was seen in 16 (45.7%) patients in fistulotomy group and 7 (20%) patients in fistulotomy with sphincterotomy group. The wound infection rate was significantly higher fistulotomy group in comparison to fistulotomy with sphincterotomy group [17].
The mean satisfaction score (out of 10) in fistulotomy group was 7.06 ± 0.54 and in fistulotomy with sphincterotomy group was 8.26 ± 0.61. The mean satisfaction score was significantly higher in fistulotomy with sphincterotomy group in comparison to the fistulotomy group [18]. All the postoperative complications were significantly more in fistulotomy group compared to fistulotomy with sphincterotomy group (Table 2).
| Studies | Incontinence no (%) | Time to recurrence (mean months) |
Skin suture healing no (%) | Follow- up (months) |
Success no (%) |
|---|---|---|---|---|---|
| Parkash et al. | 3 (3.7) | 5.3 | 66 (79.5) | 6.60 | 117 (97.5) |
| Lux et al. | 21 (45.7) | NOT REPORTED | - | 16 | 46 (100) |
| Christiansen et al. | 3 (21.4) | 13.5 | 14 (100) | 12.48 | 12 (85.7) |
| Lewis | NOT REPORTED | NOT REPORTED | - | NOT REPORTED | 29 (90.6) |
| Gemsenjager | 1 (4.8) | NOT REPORTED | 20 (95.2) | 2.9 | 20 (95.2) |
| Toccaceli et al. | 0 | 0 | 33 (91.7) | 12 | 33 (91.7) |
| Roig et al. | 5 (20.0) | 2.3 | - | 24 | 28 (90.3) |
| Perez et al. | 4 (17.4) | NOT REPORTED | 8 (28.6) | 36 | 26 (92.9) |
| Jivapaisarnpong et al. | 0 | 1.5 | - | 14 | 29 (87.9) |
| Roig et al. | 11 (18.3) | 5.4 | - | 13 | 67 (89.3) |
| Kraemer et al. | 3 (4.2) | 34 (89.5) | 16 | 37 (97.4) | |
| Arroyo et al. | 8 (11.6) | 20 | 21 (30.0) | 81 | 64 (91.4) |
| Ratto et al. | 8 (11.6) | 17.4 | - | 29.4 | 69 (95.8) |
| Hirschburger et al. | 3 (6) | NOT REPORTED | - | 22 | 44 (88.0) |
| Average Our study | 13.1 | 9.3 | 73.5 | 26.3 | 92.4 |
| Fistulotomy with sphincteroplasty | 2 (5.7%) | 4 (11.4%) | - | 180 days | 91.65% |
| Fistulotomy | 9 (25.7%) | 12 (34.3%) | - | 180 days | 70% |
Conclusion
In our prospective study, we want to conclude that the total outcomes for the patient with fistula-in-ano, in which if do only fistulotomy there are high chances of recurrence, incontinence, less satisfaction to the patient and more wound infection due to incomplete drainage of abscess. While if we perform fistulotomy with sphincteroplasty, the outcomes are much better in terms of recurrence, incontinence, post op wound infection and patient satisfaction. Hence, by our study, we can recommend that for high fistula-in-ano, we should do fistulotomy with sphincteroplasty.
Acknowledgment
None
Funding
The authors received no funding for this work.
Conflict of Interest Statement
Author declares that they have no conflict of interest.
References
- Sainio P. Fistula-in-ano in a defned population. Incidence and epidemiological aspects. Ann Chir Gynaecol 2018;73:219-224.
[Goggle scholar] [Pubmed]
- Bleier JIS, Moloo H. Current management of cryptoglandular fistula-in ano. World J Gastroenterol 2011;17:3286- 3291.
[Crossref] [Goggle scholar] [Pubmed]
- Malik Al, Nelson RL. Surgical management of anal fistulae: A systematic review. Colorectal Dis. 2008;10:420-430.
[Crossref] [Goggle scholar] [Pubmed]
- Ratto C, Litta F, Donisi L, Parello A. Fistulotomy or fistulectomy and primary sphincteroplasty for anal fistula (FIPS): A systematic review. Tech Coloproctol 2015;19: 391-400.
[Crossref] [Goggle scholar] [Pubmed]
- Parkash S, Lakshmiratan V, Gajendran V. Fistula-in-ano: treatment by fistulectomy, primary closure and reconstitution. Aust N Z J Surg. 1985;55:23-27.
[Crossref] [Goggle scholar] [Pubmed]
- Lux N, Athanasiadis S. [Functional results following fistulectomy with primary muscle suture in high anal fistula. A prospective clinical and manometric study]. Chirurg. 1991;62:36-41.
[Goggle scholar] [Pubmed]
- Christiansen J, Ranholt C. Treatment of recurrent high anal fistula by total excision and primary sphincter reconstruction. Int J Colorectal Dis. 1995;10:207-209.
[Crossref] [Goggle scholar] [Pubmed]
- Gemsenj Ager E. [Results with a new therapy concept in anal fistula: Suture of the anal sphincter]. Schweiz Med Wochenschr. 1996;126:2021-2025.
- Roig, Garcia-Armengol, Jordan, Alos, Solana. Immediate reconstruction of the anal sphincter after fistulotomy in the management of complex anal fistulas. Colorectal Dis. 1999;1:137-140.
[Crossref] [Goggle scholar] [Pubmed]
- Perez F, Arroyo A, Serrano P, Candela F, Sanchez A, Calpena R. Fistulotomy with primary sphincter reconstruction in the management of complex fistula-in-ano: prospective study of clinical and manometric results. J Am Coll Surg. 2005;200:897-903.
[Crossref] [Goggle scholar] [Pubmed]
- Perez F, Arroyo A, Serrano P, Sanchez A, Candela F. Randomized clinical and manometric study of advancement flap versus fistulotomy with sphincter reconstruction in the management of complex fistula-in-ano. Am J Surg. 2006;192:34-40.
[Crossref] [Goggle scholar] [Pubmed]
- Jivapaisarnpong P. Core out fistulectomy, anal sphincter reconstruction and primary repair of internal opening in the treatment of complex anal fistula. J Med Assoc Thai. 2009;92:638-642. [Crossref]
[Goggle scholar] [Pubmed]
- Goggle scholar
- Kraemer M, Picke D. Fistulotomy with primary sphincter repair for the treatment of anal fistula. Coloproctology. 2011;33:104-108.
- Arroyo A, Parez-Legaz J, Moya P, Armatanzas L, Lacueva J, Parez-Vicente F. Fistulotomy and sphincter reconstruction in the treatment of complex fistula-in-ano: long-term clinical and manometric results. Ann Surg 2012; 255: 935-939 .
[Crossref] [Goggle scholar] [Pubmed]
- Ratto C, Litta F, Parello A, Parello A, Zaccone G, Donisi L. Fistulotomy with end-to-end primary sphincteroplasty for anal fistula: Results from a prospective study. Dis Colon Rectum 2013;56: 226-233.
[Crossref] [Goggle scholar] [Pubmed]
- Hirschburger M, Schwandner T, Hecker A, Kierer W, Weinel R. Fistulectomy with primary sphincter reconstruction in the treatment of high transsphincteric anal fistulas. Int J Colorectal Dis 2014;29:247-52.
[Crossref] [Goggle scholar] [Pubmed]
- Litta F, Parello A, De Simone V, Grossi U, Orefice R. Fistulotomy and primary sphincteroplasty for anal fistula: Long-term data on continence and patient satisfaction. Tech Coloproctol 2019; 23:993-1001.
[Crossref] [Goggle scholar] [Pubmed]
Copyright: © 2022 The Authors. This is an open access article under the terms of the Creative Commons Attribution NonCommercial ShareAlike 4.0 (https://creativecommons.org/licenses/by-nc-sa/4.0/). This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.