Research Article - Archives of Clinical and Experimental Surgery (2022)
A Prospective Study of Outcome of Gips Procedure as Minimal Invasive Surgical Approach for Pilonidal Sinus
Hina Gupta*, Avinash Gautam, Sumit Shukla and Ankur MaheshwariHina Gupta, Department of General Surgery, M.G.M. Medical College and M.Y. Hospital, Madhya Pradesh, India, Email: guptahina1996@gmail.com
Received: 06-Dec-2022, Manuscript No. EJMACES-22-82477; Editor assigned: 09-Dec-2022, Pre QC No. EJMACES-22-82477 (PQ); Reviewed: 26-Dec-2022, QC No. EJMACES-22-82477; Revised: 02-Jan-2023, Manuscript No. EJMACES-22-82477 (R); Published: 09-Jan-2023
Abstract
Background: Pilonidal disease is a very common anorectal problem that most often arises in the hair follicles of the natal cleft of the sacrococcygeal area. Incidence of male being affected are more than female due to their hirsute nature. Pilonidal sinuses are also associated with obesity (37%), sedentary lifestyle (44%), local irritation or trauma. Pilonidal sinus can appear as acute abscess along with sinus tract formation. The management of pilonidal sinus is mostly surgical. The most commonly used procedures are simple incision, excision, plastic surgery techniques, minimally invasive sinusectomy, marsupialization, fistulotomy.
Materials and methods: A total of 30 patients, suffering from pilonidal sinus were enrolled in the study over a period of 18 months. A detailed history relating to the disease process and about socioeconomic, cultural and economic backgrounds of the patient was taken. Patients were operated with the minimally invasive GIPS procedure which combines the principles of a minimally invasive method proposed by Lord and Millar and the individual excision of midline openings proposed by Bascom, hence, named after them.
Results: In our study we observed that 83.3% patients were males with majority (50%) of them belonging to 21-40 years age group. Majority of the patients were driver by occupation (30%) and had co-morbidities of diabetes mellitus (14%) and hypertension (16.6%). Majority of them presented with chronic discharging sinus swelling (40%). Patients operated with GIPS procedure for the pilonidal sinus had healing rate of 70% after 2 weeks with minimal complications.
Conclusions: Patients operated with GIPS procedure had better outcome with quick recovery and healing. These patients had less post- operative pain and discomfort, early resumption of daily activities with least recurrence and complication rates. Hence, GIPS procedure, being a day care procedure represents a good option for the patients of pilonidal sinus.
Keywords
Pilonidal sinus; Marsupialization; GIPS procedure; Anorectal abscess; Surgery of pilonidal sinus
Introduction
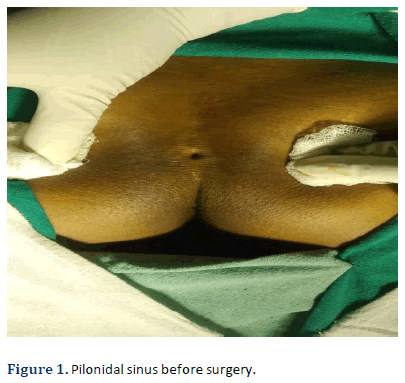
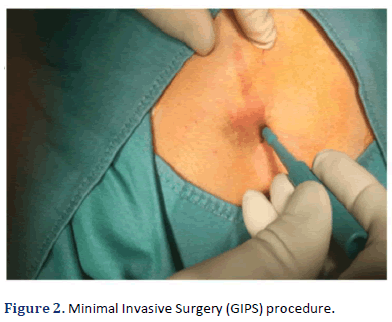
Pilonidal sinus is a common benign anorectal disease condition affecting skin and subcutaneous tissues. It was in 1833, a sinus containing hair follicles in sacrococcygeal region in a woman was described by a British Physiologist, Anatomist and Surgeon, Herbert Mayo after which he named the disease as “pilonidal sinus” [1]. A sinus tract, also known as a tiny channel, known as the pilonidal sinus may branch off from the site of the infection and open to the skin’s surface. Material from the cyst drains through the pilonidal sinus. A pilonidal cyst is usually painful, but with draining the patient might not feel pain. Incidence of male being affected is more than female due to their hirsute nature. Pilonidal sinuses are also associated with obesity (37%), sedentary lifestyle (44%), local irritation or trauma. Pilonidal sinus can appear as acute abscess along with sinus tract formation [2]. In the present era, incidence rate of pilonidal sinus is approximately 0.7% [3]. The disease is found to be a young patient disease with incidence noted in the age group of 19-25 years, male being more affected with the ratio of 4:1 [4,5]. Majority of patients were found to be a hirsute with strong wiry dark hair. Pilonidal sinus disease is basically a foreign body reaction of host tissue to the hair [6]. The tip of hair enters into the cavity, gets entrapped as barbs preventing it from being expelled [7,8]. The trapped hair elicits a foreign body reaction leading to pain, infection, abscess and eventually sinus formation. The treatment of this condition is mostly surgical. In Figure 1 there are various surgeries that are done for pilonidal sinus like Marsupialization, Excision with primary closure, Karydaki’s flap, Bascom procedure, Modified Bascom procedure, Transposition flaps (z-plasty), Rhomboid flap of Limberg, Minimal Invasive Surgery (GIPS) (Figure 2).
Materials and Methods
This is a prospective study conducted at our institute during 2020 to 2022. A total of 30 patients of more than 14 years from various socioeconomic, cultural and economic backgrounds were included in this study who were suffering from pilonidal disease. Patient undergoing Pilonidal sinus surgery by other surgical techniques were excluded from the study. Informed consent (Assent) was taken from all patients or parents of the patient included in the study.
All patients in study underwent a detailed history taking along with general examination and investigations. Their personal history, past medical history, family history, dietary history, socio economic history, clinical history pertaining to pain, hematuria and fever was recorded and documented. Various blood investigations (Complete blood Count, Renal Function Test, Serum Electrolytes, Serum Calcium); radiological investigations (X-Ray chest, Ultrasound of perianal region) were done in all the patients.
Patients were admitted for day care procedure. After anesthesia, patient was placed in prone position with buttocks gently taped apart exposing the diseased region. Each fistulous opening is probed to ac- cess the depth and direction of tracts. Skin debris, hair, epithelial linings are excised from the tracts with the help of trephines. The trephined openings are cleaned off of any residuals and left open to heal by secondary intention and dressed. Patient is kept in observation for any post-operative complications in supine position for 1-2 hours before discharge. Patient was followed up for 6 months.
Results and Discussion
This was a prospective study consisting of 30 cases suffering from pilonidal disease (Tables 1-7).
| Age Group (years) | Number of Patients | Percentage (%) |
|---|---|---|
| 18-20 | 2 | 6.6 |
| 21-40 | 15 | 50 |
| 41-60 | 9 | 30 |
| 61-80 | 4 | 13.3 |
| Gender | Number of Patients | Percentage (%) |
|---|---|---|
| Male | 25 | 83.3 |
| Female | 5 | 16.6 |
| Total | 30 | 100 |
| Occupation | Number of Patients | Percentage (%) |
|---|---|---|
| Driver | 9 | 30 |
| Tailor | 5 | 16.6 |
| Shop keeper | 8 | 26.8 |
| Student | 5 | 16.6 |
| Factory workers | 3 | 10 |
| Co-morbidities | No. of Patients | Percentage |
|---|---|---|
| Diabetes Mellitus | 3 | 14 |
| Hypertension | 5 | 16.6 |
| Obesity | 2 | 6.6 |
| Other | 0 | 0 |
| Mode of Presentation | No. of Patients | Percentage |
|---|---|---|
| Sinus with Acute Abscess | 8 | 26.6 |
| Chronic Discharging Sinus | 12 | 40 |
| Follow up week | Healing rate |
|---|---|
| First week | 30 |
| Second week | 70 |
| Sixth week | 100 |
| Three months | 100 |
| Six months | 100 |
| Complication | No. of patients | Percentage |
|---|---|---|
| Wound infection | 4 | 13.3 |
| Recurrence | 2 | 6.6 |
Age distribution
In our study, it was observed that maximum number of patients was in 21-40 years age group (50%). Also, lifestyle, occupation and demographic factors have a cumulative effect with advancing age, leading to formation of pilonidal sinuses. Similar results were found in the other study like study of Angelo Di Castro, et al [9].
Sex distribution
In our study we found that majority of the patients were male (83.3%) compared to females (16.6%). Usually overweight males with thick profuse hair growth over the sacral area presented with the disease. Similar results were also seen in studies done in Minnesota college in the past where 364 out of 31597 males (1.1%) and 22 out of 21467 females (0.11%) had pilonidal disease.
Distribution based on occupation
In our study we observed that majority of the patients belonged to lower income society with long hours of sitting work. As even in past, it was observed to be associated more commonly among jeep drivers, hence, the disease is also called, “Jeep Bottom disease”. Therefore, people associated with long hours of sitting more commonly suffers from pilonidal sinus disease. Patients with occupation involving driving, tailoring, shop keepers are more affected by the disease.
Distribution based on associated co-morbidities
In our study, we observed that patients with co-morbidities like diabetes mellitus (3 patients, 10%), hypertension (5 patients 16.6%), obesity (2 patients 6.6%) and poor hygienic conditions were observed to have delayed healing and more wound infections presenting usually with chronic discharging sinuses.
Distribution based on disease presentation
In our study, we observed Patients of pilonidal sinus presented to the OPD at various stages of their presentations. Stages of presentation are defined by the duration of the illness. It can be acute abscess presented within 7-8 days of their first presentation or chronic sinus with discharge presented months after their first presentation of illness. In our study, 8 patients presented with acute abscess (26.6%) whereas 12 patients with chron- ic sinus with discharge (40%).
Distribution based on healing rate
In our study, we operated our patients with the minimal invasive day care GIPS procedure using trephine to remove the pilonidal cyst. Patients were observed and followed up to access the healing rate of the wound after GIPS procedure. Patients were followed up after 1 week, 2 weeks, 6 weeks, 3 months and 6 months. It was observed that healing rate of most of the patients was 30% in 1st week, 70% after 2 weeks and completely healed wound was found when followed up after 6 weeks.
Distribution based on complications
In our study it was observed that when we treat patients with GIPS procedure of pilonidal surgery, patients have early ambulation, fast recovery, less pain and complications. 4 patients out of 30 (13.3%), suffered from wound infections which lead to delayed healing of the wound, whereas recurrence was observed in 2 patients (6.6 %) in our study. Similar results were found in a study conducted by Dieguez et al., in 2014 [10].
Conclusions
• From our study we can conclude that pilonidal sinus
disease has a relation with multiple factors.
• Gender of the patient, socio economic status of the
family, their occupation, hygiene, associated comorbidities and lifestyle have a direct relation with the
presence of the disease.
• Occupation plays a major role for the occurrence of
the disease.
• Our study concluded that the males have higher predilection
for the development of pilonidal sinus.
• In our study we found that the patients with dis- ease majorly were overweight, had thick hairy profuse
growth over the affected region. Excessive sweating,
unhygienic conditions, local infections are other factors
associated with the disease.
• From our study we can conclude that majority of the patients present with chronic discharging sinuses.
The outcome of GIPS procedure seen in our study in pilonidal sinus surgery are much better as it is associated with quick recovery and healing with less post-operative pain and discomfort, early resumption of daily activities with least recurrence and complication rates. Hence, GIPS procedure, being a day care procedure represent a good option for the patients of pilonidal sinus.
References
- Hodges RM. Pilonidal sinus. Boston Med Surg J 1880; 103:485-586.
- Clothier PR, Haywood IR. The natural history of the post anal (pilonidal) sinus. Ann R Coll Surg Engl. 1984; 66 (3):201-3.
[Google Scholar] [Pubmed]
- Corman ML, Nicholls RJ, Fazio VW, Bergamaschi R. Corman's Colon and Rectal Surgery. 6th edn, 2012; 195-203.
- Guerra F, Giuliani G, Amore Bonapasta S, Coletta D, La Torre F. Cleft lift versus standard excision with primary midline closure for the treatment of pilonidal disease. A snapshot of worldwide current practice. Eur Surg 2016;48(5):269-72.
- McCallum IJ, King PM, Bruce J. Healing by primary closure versus open healing after surgery for pilonidal sinus: Systematic review and meta-analysis. Bmj 2008;336(7649):868-71.
[Crossref] [Google Scholar] [Pubmed]
- Thompson MR, Senapati A, Kitchen P. Simple day-case surgery for pilonidal sinus disease. Br J Surg 2011;98(2):198-209.
[Crossref] [Google Scholar] [Pubmed]
- Senapati A, Cripps NP, Flashman K, Thompson MR. Cleft closure for the treatment of pilonidal sinus disease. Colorectal Dis 2011;13(3):333-6.
[Crossref] [Google Scholar] [Pubmed]
- Enriquez-Navascues JM, Emparanza JI, Alkorta M, Placer C. Meta-analysis of randomized controlled trials comparing different techniques with primary closure for chronic pilonidal sinus. Tech Coloproctol 2014;18(10):863-72.
[Crossref] [Google Scholar] [Pubmed]
- Di Castro A, Guerra F, Sandri GB, Ettorre GM. Minimally invasive surgery for the treatment of pilonidal disease. The Gips procedure on 2347 patients. Int J Surg 2016;36:201-5.
[Crossref] [Google Scholar] [Pubmed]
- Diéguez I, Costa A, Miró I, March Villalba JA, Del Peral M, Marco Macián A, et al. En bloc resection vs. Gips procedure in pilonidal sinus surgery. Cir Pediatr 2022;35(2):75-9.
[Crossref] [Google Scholar] [Pubmed]
Copyright: © 2023 The Authors. This is an open access article under the terms of the Creative Commons Attribution NonCommercial ShareAlike 4.0 (https://creativecommons.org/licenses/by-nc-sa/4.0/). This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.