Case Series - Archives of Clinical and Experimental Surgery (2022)
Abdominal Complications of VP Shunt in Pediatric Patients
Sarvagya Jain*, Shashi Shankar Sharma, Ram Mohan Shukla, K Lavanya, Hemant Thanna and Saksham KumarSarvagya Jain, Department of Pediatric Surgery, M.Y. Hopsital, Indore, India, Email: sarvagyajain25@gmail.com
Received: 02-Feb-2022, Manuscript No. EJMACES-22-54781; Editor assigned: 04-Feb-2022, Pre QC No. EJMACES-22-54781; Reviewed: 18-Feb-2022, QC No. EJMACES-22-54781; Revised: 23-Feb-2022, Manuscript No. EJMACES-22-54781; Published: 02-Mar-2022
Abstract
Purpose: Ventriculo Peritoneal shunt (VP shunt) is the one of the most common and remains the gold standard treatment for infants and adults with congenital or acquired hydrocephalus, such as that due to a tumor. Complications include infection, obstruction of the shunt itself, and failure of a valve, or over- and under drainage of a ventricle. Intra-abdominal complications of a VP shunt are rare. Here, we report 3 abdominal complications of VP shunt, 2 obstruction and 1 perforation.
Case report 1: 7 month male: operated case of hydrocephalus with VP shunt in situ presented with complaint of not passing motion and flatus since 3 days and abdominal distension since 2 days. X-ray showed multiple air fluid levels and Patient was explored, there were multiple adhesions in the bowel loops which were causing obstruction.
Case Report 2: 1 year male operated case of VP Shunt for hydrocephalus 1 year back c/o VP shunt coming out per rectally since 1 day and pain in abdomen.
O/e: VP shunt was coming out of anus and per abdominally patient was guarding X-ray showed: VP shunt was piercing colon and coming out from anus.
Case report 3: 4 months male not passing motion associated with abdominal distension since 2 days. Patient was operated for VP shunt 2 months back.
OE: Per abdomen was distended and PR was roomy and empty.
X-ray and suggestive of Intestinal obstruction. Patient was explored and it was found multiple adhesions in between the bowel loops.
Discussion and Conclusion: Although complications of a VP shunt are common, abdominal complications, especially intestinal obstruction and perforation are rare. Regardless of the cause, management of bowel obstruction is the same.
Keywords
Pediatric; Abdominal complications of VP shunt; Intestinal obstruction; Sigmoid perforation
Introduction
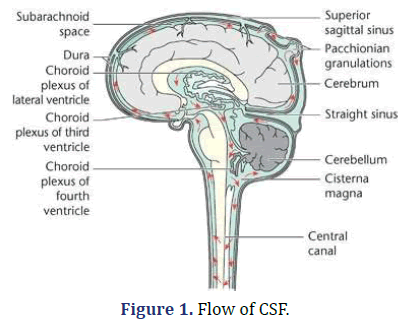
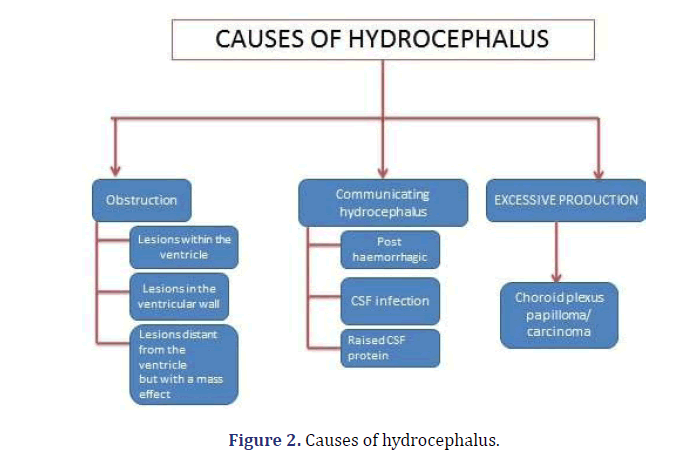
Hydrocephalus denotes an excessive accumulation of the CSF in the intracranial compartment. Normally there exists a fine balance between the CSF production by the choroid plexus and the absorption at the arachnoid villi along the superior sagittal sinuses. The CSF production=0.33 mL/kg/ hr (20 mL/hr). Almost all the fluid produced is absorbed within 8 hours. There should always be equal amount of production (by choroid plexus) and absorption of CSF (Superior saggital siunus and arachnoid villi (Figures 1 and 2).
Investigation we usually done are CT SCAN (preferred) & MRI SCAN. Treatments available for hydrocephalus are:
1. External Ventricular Drains (EVDs): temporary, bedside
2. Endoscopic third ventriculostomy: Especially useful in obstructive hydrocephalus due to aqueduct stenosis
3. Ventriculoperitoneal shunts (Gold Standard) [1].
Ventriculoperitoneal shunt (VP shunt) is the one of the most common and important tools for the treatment of hydrocephalus. It requires simple technique and demonstrates effectiveness in treating hydrocephalus [2].
Complications of VP shunt usually ranges from 24% to 47%. It Includes infection (Most common), disconnection, Over drainage of csf (headache, blood accumulation), blockage and intra-abdominal.
Complication (Intestinal obstruction and perforations are very rare complications of VP shunts (<1%).
Materials and Methodology
• Place: Department of Pediatric Surgery, M.Y. Hospital, Indore
• Duration: September 2019 to March 2021
• All 3 cases were operated case of VP shunt and later on, came with abdominal complaints.
• All 3 cases underwent exploratory laparotomy
Case report 1
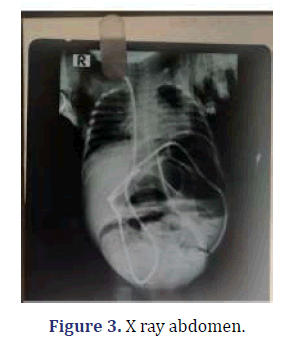
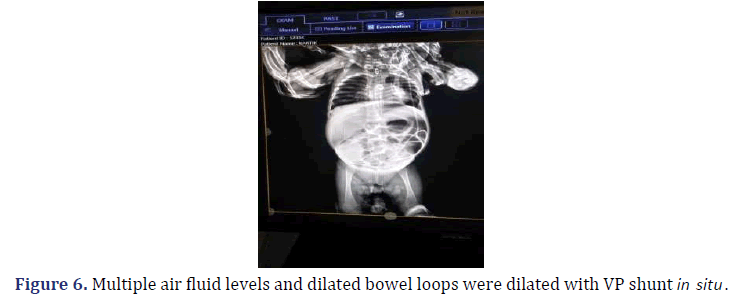
4 Month/Male, came with a complaint of not passing motion and flatus since 2 days, which was associated with abdominal distention and fever. Patient was operated case of VP shunt 3 months back. On examination, patient was vitally stable. Per abdomen was distended, and bowel loops were visible. Bowel Sound was absent on per rectal examination suggestive of roomy and empty. Routine blood investigations were within normal limits and USG was evident of dilated bowel loop, with sluggish peristaltic movement suggestive of Sub-Acute Intestinal Obstruction (SAIO)? X-ray abdomen was suggestive of multiple air fluid levels and dilated bowel loops were dilated with VP shunt in situ (Figure 3).
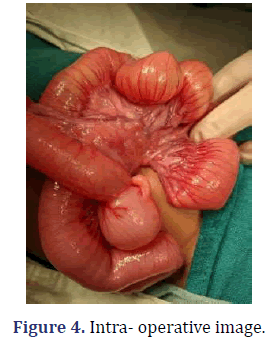
On exploration laparotomy it was found that VP shunt was passing transmesnetrically and around the tip of the bowel loops were adhered to each other causing obstruction (Figure 4).
Case report 2
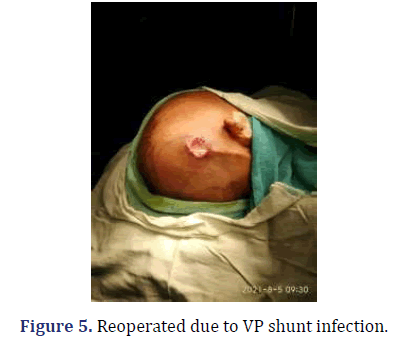
7 Month/Male, came with a complaint of not passing motion and flatus since 3 days, which was associated with abdominal distention, bilious vomiting and fever. Patient was operated for VP shunt 6 months back and 3 months back patient was reported for VP shunt due to infection and VP shunt was placed on left side. On examination, Patient was vitally stable and Per abdomen was distended, and tender. Bowel sound was hyperperistalsis. On Per rectal examination it was Roomy with fecal tinge (Figure 5).
Routine blood investigations were within normal limits and USG was suggestive of dilated bowel loop Sub-Acute Intestinal Obstruction (SAIO)? (Figure 6).
We performed Exploratory laparotomy with adhsiolysis of small bowel and relieving the obstruction and placement of VP shunt again in perihepatic space.
Case report 3
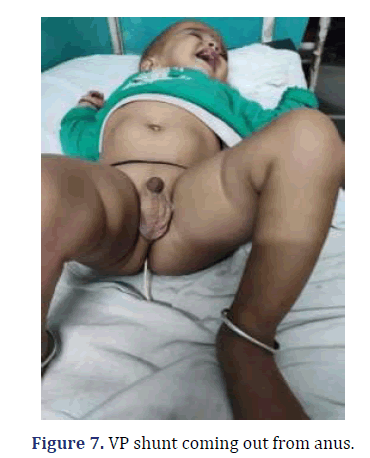
1 year male, presented with complaint of VP shunt coming out per rectally since 1 day Patient was operated for VP shunt 1 year back. On examination: Patient was vitally stable and per abdominal examination was normal. Local Examination per rectally showed VP shunt coming out per rectally (Figure 7).
Patient underwent exploratory laparotomy and it was found that VP shunt was entering the sigmoid colon and then coming out from anus. VP shunt was removed and defect was primarily repaired.
Results
All three patients were successfully discharged and are doing well (Table 1).
| Total VP shunt performed ( From September 2019 to March 2021) |
112 |
|---|---|
| Intestinal Obstruction | 2 |
| Perforation | 1 |
Discussion
Abdominal complication accounts for 10%–30%.It includes infections (5%), cyst formation (1%–2%), occlusive/mechanical and visceral perforation (<1%).
Causes of VP shunt-related intestinal obstruction [3].
1. Most common: volvulus
2. Second most common: Mechanical obstruction due to twisting of the catheter.
3. Adhesions are the rare cause of obstruction.
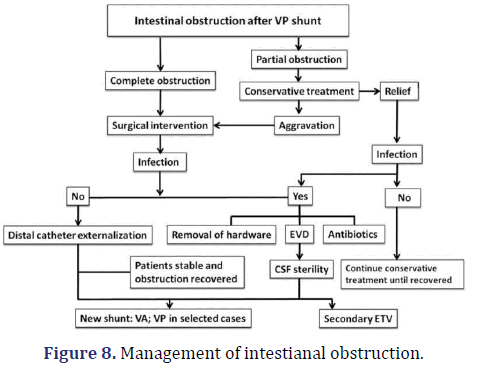
Regardless of the cause, management of bowel obstruction is the same. Conservative treatment consists of intravenous fluid and electrolyte replacement, along with placement of a nasogastric tube to decompress the stomach. Observation is warranted if a partial bowel obstruction is suspected in the absence of fever, leukocytosis, and localized abdominal pain. In the presence of complete obstruction with fever, pain, and no passage of flatus or stool, immediate surgical exploration is warranted. This is especially critical if a shunt is present as the catheter is a foreign body, and retaining a foreign body is against standard surgical principles of infection management. Furthermore, retrograde infection to the CNS is possible. Laparoscopy has been shown to be useful for the diagnosis and management of shunt-related complications such as shunt catheter entanglement [4] (Figure 8).
Akyüz [5] hypothesized that the catheter tip adheres to the visceral wall, a local inflammatory process weakens the bowel wall, and then the tip erodes into the lumen over a period [6]. A constant pressure abutting the tip of catheter with the viscera or the extruding surface usually accompanies this kind of setting. This favours tip migration through the abnormal site. The ventricular end of the VP shunt is likely to be extruded if it is insecurely anchored to the pericranium. Another factor responsible for the occurrence of this complication is extensive subcutaneous dissection at the time of primary surgery. Vuyyuru [7] reported that malnutrition and former abdominal surgery may increase the risk of migration because of adhesions that arose from infection. In children because of weak musculature of bowel, they are more susceptible to intestinal perforation [8].
Intestinal perforation usually occurs in the colon, rarely occurs in the stomach, small intestine and very rarely occurs in the duodenum. Most cases of a catheter, that entering into the intestine are diagnosed when the tube was found outside of the anus and mouth. VP shunt should ideally place properly in perihepatic space.
Conclusion
In an operated Case of VP Shunt, if patient comes with abdominal distension and pain, we should suspect obstruction and perforation due to VP shunt. Presence of local shunt tract infection, presence of meningitis, and shunt dependency are the main factors causing these complications.
Management include;
Intestinal obstruction: RT insertion, IV fluid resuscitation, antibiotics and adhesionolysis.
Perforation: By removing the catheter, then sealing the hole in the intestinal wall with open surgery or laparoscopicsurgery.
References
- Williams N, O' Connell PR. Bailey & Love's short practice of surgery. 27th edn, CRC press;2008.
- Van Dong H, Van HD, Vu HT, Chu HT. Duodenal perforation as a postoperative complication after ventriculoperitoneal shunt: A case report. Int J SurgCase Rep 2021; 83:106059.
[Crossref] [Google Scholar] [Pubmed]
- Zhao R, Shi W, Yu J, Gao X, Li H. Complete intestinal obstruction and necrosis as a complication of a ventriculoperitoneal shunt in children: a report of 2 cases and systematic literature review. Medicine 2015 ;94(34): e1375.
[Crossref] [Google Scholar] [Pubmed]
- Wu Y, Green NL, Wrensch MR, Zhao S, Gupta N. Ventriculoperitoneal shunt complications in California: 1990 to 2000. Neurosurgery 2007;61(3):557-63.
[Crossref] [Google Scholar] [Pubmed]
- Akyüz M, Uçar T, Göksu E. A thoracic complication of ventriculoperitoneal shunt: symptomatic hydrothorax from intrathoracic migration of a ventriculoperitoneal shunt catheter. Br J Neurosurg 2004;18:171–3.
[Crossref] [Google Scholar] [Pubmed]
- Bansal H, Gupta G, Gupta M, Kaushal R. Unusual ventriculoperitoneal (VP) shunt tube extrusion through anus in a child with Dandy Walker malformation: A rare case report. J Clin Diagn Res 2015;9:25–6.
[Crossref] [Google Scholar] [Pubmed]
- Vuyyuru S, Ravuri SR, Tandra VR, Panigrahi MK. Anal extrusion of a ventriculoperitoneal shunt tube: endoscopic removal. J Pediatr Neurosci 2009;4:124–6.
[Crossref] [Google Scholar] [Pubmed]
- Hai A, Rab AZ, Ghani I, Huda MF, Quadir AQ. Perforation into gut by ventriculoperitoneal shunts: a report of two cases and review of the literature. J Indian Assoc Pediatr Surg 2011;16:31–3.
[Crossref] [Google Scholar] [Pubmed]
Copyright: © 2022 The Authors. This is an open access article under the terms of the Creative Commons Attribution NonCommercial ShareAlike 4.0 (https://creativecommons.org/licenses/by-nc-sa/4.0/). This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.