Brief Report - Archives of Clinical and Experimental Surgery (2024)
An Original and Unexpensive Technique of Port-Site Fascial Closure Using Veress Needle: Technique Description
Jitao Sheri* and Sima TiagoJitao Sheri, Department of Surgery, Ahmadu Bello University, Kaduna State, Nigeria, Email: Sjitao123@yahoo.com
Received: 29-Jul-2024, Manuscript No. EJMACES-24-143728; Editor assigned: 31-Jul-2024, Pre QC No. EJMACES-24-143728 (PQ); Reviewed: 14-Aug-2024, QC No. EJMACES-24-143728; Revised: 21-Aug-2024, Manuscript No. EJMACES-24-143728 (R); Published: 29-Aug-2024
Abstract
Veress needle features a blunt inner stylet with insufflation holes and a sharp outer cannula and is widely used to induce pneumoperitoneum in laparoscopic surgery. Closure of laparoscopic port incisions is important to prevent or reduce the incidence of port-site incisional hernia and its complications. There are different instruments used to perform the closure of port incisions such as Bercy needle, Endoclose needle, Ranfac needle, Deschamps needle, etc. We describe a closing technique using a Veress needle lacking other instruments.
Keywords
Fascial closure; Veress needle; laparoscopy; Bariatric surgery
Introduction
Laparoscopic surgery is widely practiced and offers realistic benefits over conventional surgery. There is considerable variation in results between surgeons, concerning port-site complications. Laparoscopic Port-site Closure (LPC) can be performed by different techniques. There has been progressive development of new methods and refinement of existing techniques to achieve the best outcome. In some of the closure techniques, special instruments and types of needles are used to perform the LPC [1].
With the increased diffusion of laparoscopic surgery for many abdominal procedures, Port-site Incisional Hernias (PIH) have become more frequent (1% to 6%), along with their related complications (bowel or omentum incarceration and Richter’s hernia) [2]. Their operative repair is part of the daily routine of every general surgeon. It can be extremely invasive with a long and painful period of illness and even leading in some cases to a negative outcome. Surgery can be extremely complex due to the size of the defect or sac content, the extent of intraabdominal adhe- sions, and the length of the operation.
Other studies show an incidence of PIH from 1% to 22%, but the real incidence may be higher, as some patients remain asymptomatic or do not return to the primary surgeon [2-5]. PIH could develop at any port-site; however, it most frequently develops at the midline [1].
Several risk factors have been described for the development of PIH like the trocar diameter, the trocar design, pre-existing fascial defects as well as some operation- and patient-related factors. The risk of port-site hernia is greater in obese patients due to their larger preperitoneal space and elevated intra-abdominal pressure. In these patients and in cases of a larger trocar diameter, it seems to be recommendable to close port-sites by suture to avoid a later hernia development [6-9]. Other factors may influence the risk of this complication such as iterative manipulations, prolonged interventions, repeated repositioning, wound infection, diabetes mellitus and use of a trocar anchoring system [10-13].
It is recommended that all 10 mm and 12 mm trocar sites in adults and all 5-mm port sites in children be closed, incorporating the peritoneum into the fascial closure [4]. Opinions vary whether a 5 mm trocar- site defect should be closed or not in adult patients [6]. According to some authors, the risk of hernia development after 5 mm trocar placement seems to be a rare complication, thus 5 mm port-sites can be left without any suture [14].
Materials and Methods
Technique description
The Veress is a long needle with a blunt hollow spring- loaded trocar in its center. The blunt trocar springs back at and through the resistance of the abdominal wall, and springs out again to protect the viscera from the needle once the resistance disappears within the abdominal cavity. Gas flows through the hollow to create the initial pneumoperitoneum. The bore of the needle limits the initial flow during insufflation. Although many surgeons prefer to induce pneumoperitoneum with the open technique, the Veress needle is still widely used in clinical practice.
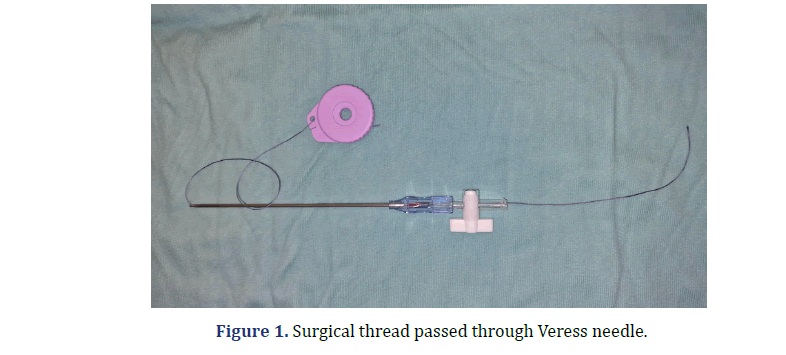
We describe a method of closing laparoscopic port- site using a classic Veress needle. We usually close them with a Ranfac needle. After a mini gastric bypass, lacking Ranfac needle, we used a thread passed through the Veress needle, as shown in Figure 1. The thread is inserted into the Veress needle lever, slid through the cannula and exited from the internal stylet, and this might be the most challenging aspect.
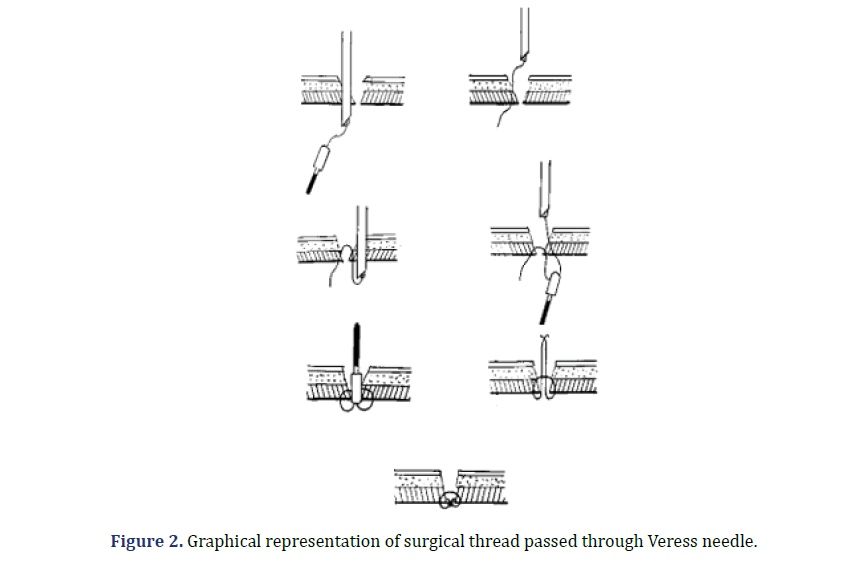
Steps for surgical thread passed through Veress needle
1. The Veress needle with the built-in thread is passed from one side of the port-site and the end of the thread is grapped by a Johannes for ceps.
2. The needle is then retracted and passed parallel to the other side of the port-site.
3. A Johannes forceps grabs the end of the thread, and the needle is retracted.
4. The same forceps, passed from the outside of the port-site, grabs both ends of the threads and withdraws them outside the abdominal cavity.
5. The knot is performed outside.
6. Final result is an introflexed knot.
Graphical representation of surgical thread passed through Veress needle was shown in Figure 2, and Some intraoperative images are reported in Figure 3.
Result and Discussion
The technique was used in 15 patients, 11 females and 4 males) with a mean age of 54.6 years (36-79) and the average BMI was 36.8 kg/m2 (27-51). Surgeries performed were sleeve gastrectomy (6), gastric bypass (1), cholecystectomy (5), left colectomy (1), right colectomy (1) and Nissen fundoplicatio (1) in the last 18 months using this 10 mm-12 mm ports access final closure, especially in obese patients (BMI>30) (BMI- Body Mass Index). The total number of 10 mm or 12 mm ports were 32. All patient details are listed in Table 1 (baseline characteristics). The 5 mm ports were not treated.
| Patient characteristics | Values |
|---|---|
| Patients number | 15 |
| Ports treated | 32 |
| Female/male | 11/4 |
| Age (years) | 54.6 (36-79) |
| BMI (kg/m2) | 36.8 (27-51) |
| Surgeries performed | |
| Sleeve gastrectomy | 6 |
| Gastric bypass (RY) | 1 |
| Cholecystectomy | 5 |
| Left colectomy | 1 |
| Right colectomy | 1 |
| Nissen fundoplicatio | 1 |
| Clavien-Dindo 0 | 14 |
| Clavien-Dindo 1 | 1 |
| Postop port bleeding | 0 |
| Port site infection | 0 |
| Incisional hernia | 0 |
| Postop. VAS Day 1 (mean)* | 2 |
| Postop. VAS Day 2 (mean) | 1, 6 |
Note: BMI-Body Mass Index; *VAS-Visual Analogic Score; Scale 1-10; related to pain in the port closure.
All patients were followed up with clinical visit at 7 postoperative day, 1 and 6 months, evaluating for postoperative port site infections, incisional hernias and of course other items and complications related to every specific operation. In selected cases abdominal ultrasound was performed. No bowel or vascular injury related to the procedure were reported. A VAS (Visual Analogic Score, 0-10 score) was used for post-operative pain record specifically related to port closure. The minimum of follow up was 6 months, maximum 18 months.
Conclusion
Time of procedure takes about 2-3 minutes for each port. The loop insertion in the Veress needle may be the most challenging aspect, a bigger loop must be prefered for greater stiffness (1 or 0 size better than 00). This report aims to describe an original use of Veress needle generally used to create pneumoperitoneum for laparoscopy, used even to close 10-12 mm port at the end of laparoscopic procedure, conceived for an unexpected lack of the usual fascial closure device. The technique may be used as a safe alternative if the usual device is not available especially in obese patients, with a very quick training and no additional costs.
References
- Hussain A, Mahmood H, Singhal T, Balakrishnan S, Nicholls J, El-Hasani S, et al. Long-term study of port-site incisional hernia after laparoscopic procedures. JSLS 2009;13(3):346-349.
[Google Scholar] [Pubmed]
- Di Lorenzo N, Coscarella G, Lirosi F, Gaspari A. Port-site closure: A new problem, an old device. JSLS 2002 ;6(2):181-183.
[Google Scholar] [Pubmed]
- Jayaraman S, Rao SD. Case series of umbilical and extra-umbilical port site herniae. Indian J Surg 2013;75(Suppl 1):488-491.
[Crossref] [Google Scholar] [Pubmed]
- Lasheen A, Safwat K, Fiad A, Elmoregy A, Hamed AW. Port-site closure using a modified aptos needle. JSLS 2013;17(2):312-315.
[Crossref] [Google Scholar] [Pubmed]
- Di Lorenzo N, Coscarella G, Lirosi F, Pietrantuono M, Susanna F, Gaspari A, et al. Trocars and hernias: A simple, cheap remedy. Chir Ital 2005;57(1):87-90.
[Google Scholar] [Pubmed]
- Tonouchi H, Ohmori Y, Kobayashi M, Kusunoki M. Trocar site hernia. Arch Surg 2004 ;139(11):1248-1256.
[Crossref] [Google Scholar] [Pubmed]
- Leibl BJ, Schmedt CG, Schwarz J, Kraft K, Bittner R. Laparoscopic surgery complications associated with trocar tip design: Review of literature and own results. J Laparoendosc Adv Surg Tech A 1999;9(2):135-140.
[Crossref] [Google Scholar] [Pubmed]
- Tarnay CM, Glass KB, Munro MG. Entry force and intra-abdominal pressure associated with six laparoscopic trocar-cannula systems: A randomized comparison. Obstet Gynecol 1999;94(1):83-88.
[Crossref] [Google Scholar] [Pubmed]
- Eid GM, Collins J. Application of a trocar wound closure system designed for laparoscopic procedures in morbidly obese patients. Obes Surg 2005;15(6):871-873.
[Crossref] [Google Scholar] [Pubmed]
- Nacef K, Chaouch MA, Chaouch A, Khalifa MB, Ghannouchi M, Boudokhane M, et al. Trocar site post incisional hernia: About 19 cases. Pan Afr Med J 2018;29:183.
[Crossref] [Google Scholar] [Pubmed]
- Ceccarelli G, Patriti A, Batoli A, Bellochi R, Spaziani A, Pisanelli MC, et al. Laparoscopic incisional hernia mesh repair with the “double-crown” technique: A case-control study. J Laparoendosc Adv Surg Tech A 2008;18(3):377-382.
[Crossref] [Google Scholar] [Pubmed]
- Campanile FC, Podda M, Pecchini F, Inama M, Molfino S, Bonino MA, et al. Laparoscopic treatment of ventral hernias: The Italian national guidelines. Updates Surg 2023;75(5):1305-1336.
[Crossref] [Google Scholar] [Pubmed]
- Silecchia G, Campanile FC, Sanchez L, Ceccarelli G, Antinori A, Ansaloni L, et al. Laparoscopic ventral/incisional hernia repair: Updated Consensus Development Conference based guidelines [corrected]. Surg Endosc 2015;29(9):2463-2484.
[Crossref] [Google Scholar] [Pubmed]
- Lambertz A, Stüben BO, Bock B, Eickhoff R, Kroh A, Klink CD, et al. Port-site incisional hernia–a case series of 54 patients. Ann Med Surg (Lond) 2017;14:8-11.
[Crossref] [Google Scholar] [Pubmed]