Case Report - Archives of Clinical and Experimental Surgery (2023)
Atraumatic Spontaneous Splenic Rupture: First Presentation of Metastatic Relapse in a Patient of Ovarian Carcinoma
Saikalyan Guptha A*, Ravi kumar H, Karthik H S, Manikanta Lgandula and Rambhupal ChoudarySaikalyan Guptha A, Department of General Surgery, Vydehi Institute of Medical Sciences and Research Centre, Bangalore, India, Tel: +919663313222, Email: drsaikalyanguptha@gmail.com
Received: 05-Jan-2023, Manuscript No. EJMACES-23-85384; Editor assigned: 09-Jan-2023, Pre QC No. EJMACES-23-85384 (PQ); Reviewed: 23-Jan-2023, QC No. EJMACES-23-85384; Revised: 30-Jan-2023, Manuscript No. EJMACES-23-85384 (R); Published: 06-Feb-2023
Abstract
Splenic rupture is a potentially life-threatening condition and the majority of cases are secondary to trauma. Atraumatic Splenic Rupture or Spontaneous Splenic rupture is rare and is usually secondary to underlying pathological condition. Splenic rupture secondary to metastasis is very rare. We present a case report of a 53-year-old elderly female who presented to casualty with acute abdominal pain. Abdominal imaging showed splenic rupture with active hemorrhage and hemoperitoneum. She underwent emergency exploratory laparotomy and splenectomy. She made a full recovery. Postoperative period was complicated due moderate COVID-19 infection and was treated with a full course of remdesivir and Karnataka state COVID-19 protocol. Following discharge, she was referred medical oncologist and completed 6 cycles of Paclitaxel and Carboplatin.
Keywords
Spontaneous splenic rupture; Ovarian adenocarcinoma; Splenic metastasis; Emergency splenectomy
Introduction
Splenic rupture is potentially life-threatening condition. It is typically caused by a blow to the left upper abdomen or the left lower chest, such as might happen during sporting accidents, fistfights and car crashes. Injury to spleen is seen in an estimated 30% of blunt abdominal trauma [1]. The extent of the injury determines whether it is managed conservatively or surgically. Individuals present to the emergency department with an acute abdomen and shock. There is a dramatic shift toward successful nonoperative management of hemodynamically stable patients [1]. Ruptures occurring without trauma are often called spontaneous or atraumatic splenic rupture in literature [2,3].
Spontaneous or atraumatic splenic rupture is rare. Earliest description of Spontaneous splenic rupture was made by Rokitansky in 1861 and Atkinson in 1874, accounts for 1% of all splenic ruptures [4]. The spleen can rupture in the following circumstances: trauma to a diseased spleen; trauma to a normal spleen; spontaneous rupture of diseased spleen (pathologic rupture) and spontaneous rupture of a normal spleen [5].
A variety of underlying conditions predispose to splenic rupture. Bacterial, viral and protozoan infections including infectious mononucleosis and malaria, have been documented as the most common causes of atraumatic rupture [1,5,6]. Neoplasms including leukaemias, lymphoma, angiosarcoma, choriocarcinoma are also documented [3].
We present a case of spontaneous rupture of spleen found to be a metastatic relapse of ovarian carcinoma.
Case Presentation
A 53-year-old female presented to the emergency department with complaints of abdominal pain in the left upper abdomen. Pain was throbbing in nature, sudden spontaneous onset, gradually progressed to severe intensity. Pain associated with discomfort in the left shoulder. No specific aggravating factors. Pain was not relieved with analgesics. Not associated with vomiting. Not associated with constipation or loose stools. Not associated with burning micturition. Not associated with blood in urine or stools
She was diagnosed with Serous carcinoma (grade 2/high grade) involving both ovaries and omentum, TNM stage (y) pN0, FIGO stage IIIB in 2016 and had undergone Radical Hysterectomy with bilateral Salpi ngo-Oopherectomy and Omentectomy followed by chemotherapy-radiotherapy.
She was not taking any anticoagulants at the time of presentation. She had no family history of ovarian cancer or breast cancer.
On examination, she was moderately built and well-nourished. She was conscious oriented to time, place and person. Pulse of 106 beats per minute was rapid. Blood pressure of 106/68 mm hg was with in normal limit. Mild pallor noted. Distended abdomen with midline scar noticed, healthy, healed by primary intension. Guarding in the left hypochondrium noted. Abdomen soft to palpate with no palpable hepatosplenomegaly. Shifting dullness not present on examination. Bowel sounds heard.
Investigation
A standard 12 lead electrocardiogram showed sinus tachycardia. Chest radiograph showed normal broncho- vascular marking and lung fields. Complete blood count showed leukocytosis, FAST scan showed splenomegaly with hematoma and hemoperitoneum in the left hypochondrium.
• Random blood sugars were normal.
• Renal function tests were normal.
• Serum electrolytes were normal.
• Serology for HIV, HBsAg, and HCV were negative.
• Patient was screened for COVID-19 with GeneXpert and was found to be negative pre-operatively.
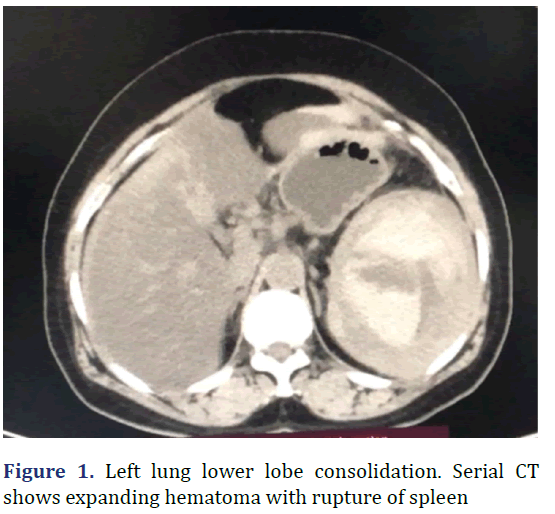
CECT abdomen showed gross hepatomegaly, splenomegaly with a large predominantly hyperdense collection occupying entire spleen, suggestive of hematoma with active extravasation of contrast along inferior pole, mild hemoperitoneum (Figure 1).
Diagnosis
A diagnosis of Atraumatic spontaneous splenic rupture with expanding splenic hematoma and hemoperitoneum was made.
Treatment
Patient was triaged and resuscitated with intravenous fluids.
As FAST and CT abdomen suggested hemoperitoneum along with splenic rupture, she underwent emergency Explor erative atory Laparotomy and splenectomy. Intraopfindings include hemoperitoneum of 500 ml with clots and splenomegaly with 10 cm laceration over the an teromedial surface of the spleen.
Outcome
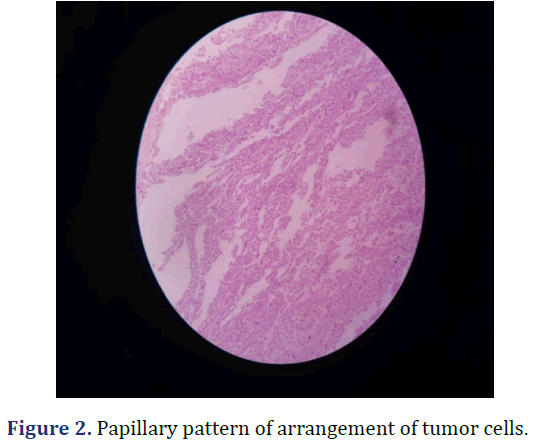
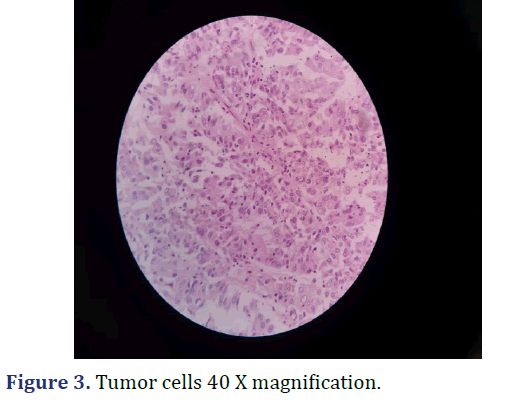
Histopathological Examination of the specimen showed metastatic adenocarcinoma compatible with known case of carcinoma ovary (Figures 2 and 3).
On fifth post operative day she developed fever and breathlessness. RTPCR test for COVID-19 was positive and she was isolated. Chest radiograph and digital plet-hysmography suggested moderate and needed intensive care. She was treated with full course of Rem-desevir, Dexamethasone and Enoxaparin as per Karna taka State COVID-19 protocol. She developed high blood sugars on sixth post operative day and was treated with insulin atrapid with TID GRBS monitoring. She developed Klebsiella Pneumonia Lower respiratory tract co-infection on post operative day 8.7- day course Amikacin and 12-day course of Piperacillin was added to treat the co infection. She needed 9 days of supplemental oxygen via facemask since the start of COVID -19 infection. Following 14 days of intensive care she was symptomatically better and was discharged with advice of home isolation.She was referred to medical oncologist and underwent 6 cycles of palliative chemotherapy with Paclitaxel and Carboplatin.
Results & Discussion
Spontaneous rupture of spleen is a rare life threatening entitiy. Majority of the spontaneous splenic rupture patients present with peritoneal symptoms including pain, tenderness, guarding and features of hemorrhagic shock. Spontaneous Splenic rupture accounts for 1% of all splenic ruptures [4]. In a recent systematic review of 613 cases of splenic rupture 48 cases were attributed to non-hematologic neoplastic causes [7].
Spontaneous splenic rupture has been attributed to many causes (Table 1) but almost always occurs as a of an enlarged or diseased spleen [1]. Splenic metastasis of ovarian cancer appears to be more common in serous cystadenocarcinomas [8]. Splenic metastasis usually occurs postoperatively and simultaneously with dissemination to the greater omentum and pelvic cavity [8]. Primary tumors with splenic metastases, systematically reported in Western countries, are mainly melanomas and lymphomas, followed by breast, lung and ovarian cancers [9].
| Cause | Variations |
|---|---|
| Infections | Bacterial (Staphylococci, Streptococci, Clostridium, Actinomyces, Pseudomonas, Salmonella, Enterobacter, Campylobacter, Haemophilus, tularemia, brucellosis, legionella, tuberculosis) Viral (infectious mononucleosis, mumps, hepatitis A, cytomegalovirus, dengue, Vermicelli zoster, human immunodeficiency virus, virus associated hemophagocytic syndrome) Protozoal (malaria, kala-azar). Other (syphilis, hydatid disease, typhus, leptospirosis, Q fever, candidiasis). |
| Hematologic conditions | Hemophilia, congenital factor XIII deficiency, protein S deficiency, ITP, TTP, hemolytic anemia, polycythemia vera, leukemia, lymphoma, myelofibrosis, multiple myeloma, congenital afibrinogenemia. |
| Metabolic disorders | Amyloidosis, Wilson disease, Gaucher disease, Niemann-Pick disease. |
| Local splenic disorders | Splenic cyst, angiomatosis of the spleen, splenic vein thrombosis, portal hypertension. |
| Splenic malignancy | Primary (angiosarcoma). Secondary (metastatic carcinoma, teratoma, melanoma, or choriocarcinoma). |
| Drug Therapy | Heparin, Coumadin, streptokinase, G-CSF, ticlopidine, dicumarol. |
| Iatrogenic | ESWL or operative injury. |
The Orloff and Peskin criteria are used to establish the diagnosis of atraumatic idiopathic splenic rupture [5]. Crate and Payne have added a fifth criterion stating that full virological studies of acute phase and convalescent serum should show no significant rise in antibody titres suggesting recent viral infection [10].
Orloff and peskin’s criteria for spontaneous rup - ture of normal spleen
• On thorough questioning, either prior to operation or in retrospect after operation, there should be no history of trauma or unsual effort which conceivably could injure the spleen.
• There should be no evidence of disease on the organs other than the spleen that is known to affect the spleen adversely and, thereby, could cause it to rupture.
• There should be no perisplenic adhesions or scarring of the spleen which suggests that it had been traumatized or had ruptured previously.
• Other than the findings of hemorrhage and rupture, the spleen should be normal on both gross and histological examination.
Individuals may present to emergency department with an acute abdomen and hypovolaemic shock. Abdominal examination may reveal signs of peritonitis, Kehr’s sign (left diaphragmatic irritation resulting in referred left shoulder pain) and Balance sign (palpable tender mass in the left upper quadrant). Other clinical findings include nausea, vomiting or syncopal episodes. FAST is now considered the best initial imaging method for unstable patients.
Management is determined by hemodynamic stability and underlying pathology. There has been a shift toward non-operative management in clinically stable patients. Ongoing hemorrhage, hemodynamically unstable patients and suspicion of neoplasm surgical management is recommended. Based on the extent of injury and suspicion of malignancy surgical options are splenorraphy and splenectomy. Transcatheter embolization is another option in stable patients.
Conclusion
The case we reported is one of the rare presentations. She had spontaneous rupture of spleen. The specimen showed metastatic relapse of the ovarian carcinoma and post-operative period was complicated with moderate COVID-19 infection and Klebsiella Pneumonia co infection. Despite that patient recovered and underwent 6 cylces of chemotherapy with Paclitaxel and Carboplatin and was discharged in a stable condition.
References
- Tataria M, Dicker RA, Melcher M, Spain DA, Brundage SI. Spontaneous splenic rupture: The masquerade of minor trauma. J Trauma 2005;59(5):1228-30.
[Crossref] [Google Scholar] [Pubmed]
- Kocael PC, Simsek O, Bilgin IA, Tutar O, Saribeyoglu K, Pekmezci S, et al. Characteristics of patients with spontaneous splenic rupture. Int Surg 2014;99(6):714-8.
[Crossref] [Google Scholar] [Pubmed]
- Renzulli P, Hostettler A, Schoepfer AM, Gloor B, Candinas D. Systematic review of atraumatic splenic rupture. Br J Surg 2009;96(10):1114-21.
[Crossref] [Google Scholar] [Pubmed]
- Dunphy L, Abbas SH, Patel A, Tebala G. Spontaneous splenic rupture: A rare first presentation of diffuse large B cell lymphoma. BMJ Case Reports CP 2019;12(8):e231101.
- Debnath D, Valerio D. A traumatic rupture of the spleen in adults. J R Coll Surg Edinb 2002;47(1):437-45.
[Google Scholar] [Pubmed]
- Kinderknecht JJ. Infectious mononucleosis and the spleen. Current sports medicine reports. 2002;1(2):116-20.
[Crossref] [Google Scholar] [Pubmed]
- Aubrey-Bassler FK, Sowers N. 613 cases of splenic rupture without risk factors or previously diagnosed disease: A systematic review. BMC Emerg Med 2012;14:12.
[Crossref] [Google Scholar] [Pubmed]
- Lv M, Li Y, Luo C, Liu P, Yang J. Splenic metastasis of ovarian clear cell adenocarcinoma: A case report and review of the literature. Exp Ther Med 2014;7(4):982-6.
[Crossref] [Google Scholar] [Pubmed]
- Siler J, Hunter TB, Weiss J, Haber K. Increased echogenicity of the spleen in benign and malignant disease. Am J Roentgenol 1980;134(5):1011-4.
- Crate ID, Payne MJ. Is the diagnosis of spontaneous rupture of a normal spleen valid? J R Army Med Corps 1991;137(1):50-1.
[Crossref] [Google Scholar] [Pubmed]
Copyright: © 2023 The Authors. This is an open access article under the terms of the Creative Commons Attribution NonCommercial ShareAlike 4.0 (https://creativecommons.org/licenses/by-nc-sa/4.0/). This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.