Research Article - Archives of Clinical and Experimental Surgery (2024)
Comparison of Toric Intraocular Lens Calculations Between the IOLMaster 700 and Pentacam AXL
Mohamed R. Gemae1 and Davin Johnson2*2Department of Ophthalmology, Kingston Health Sciences Center, Kingston, Canada
Davin Johnson, Department of Ophthalmology, Kingston Health Sciences Center, Kingston, Canada, Email: davin.johnson@queensu.ca
Received: 10-Jul-2024, Manuscript No. EJMACES-24-141252; Editor assigned: 12-Jul-2024, Pre QC No. EJMACES-24-141252 (PQ); Reviewed: 26-Jul-2024, QC No. EJMACES-24-141252; Revised: 02-Aug-2024, Manuscript No. EJMACES-24-141252 (R); Published: 12-Aug-2024
Abstract
Purpose: To compare toric IOL (Intra Ocular Lenses) suggestions for power, toric, and IOL alignment between the IOLMaster 700 and Pentacam AXL (Axial Length).
Methods: This single-center retrospective chart review analyzed the charts of 62 patients (n=93 eyes) who underwent cataract surgery with a toric IOL between January and April 2022. For all patients, preoperative biometry was measured using both the IOLMaster 700 and Pentacam AXL, followed by IOL calculations performed on the Barrett Toric Online Calculator. The suggested IOL power and toric were defined as spherical equivalent power and toric power closest to plano and minimal residual astigmatism, respectively. Surgeons used lens suggestions as per IOLMaster 700 measurements, with Pentacam AXL being used as a confirmatory test. Patients with a history of laser refractive surgery, corneal disease, or in whom cataract density precluded measurements with either device were excluded. The outcome measures compared between devices were power, toric, and alignment suggestions.
Results: Power suggestions were within ± 0.5D in 94% of the eyes, and were identical in 54%. Toric suggestions differed by ± 1 toric step in 100% of eyes, and were identical in 67%. IOL alignment suggestions, however, were slightly more variable and differed by ± 5º in 38-55% of eyes. At one-month post-op, the mean absolute error in spherical equivalent was nearly identical between devices.
Conclusion: Our results show that IOLMaster 700 and Pentacam AXL show generally similar TORIC calculations with respect to spherical equivalent and suggested toric power. Small differences in alignment axis are frequent between the two devices and warrant further study.
Keywords
Biometry; Cataract surgery; Corneal astigmatism; Toric IOL
Introduction
Up to one third of patients undergoing cataract surgery have clinically significant astigmatism [1,2]. Despite the increasing use and improvements of toric Intra Ocular Lens (IOL), methods of astigmatism corrections still lag behind standard lenses with only 50% of patients achieving <0.5D (Diopters) of astigmatism using the Barrett toric calculator [3]. A number of factors account for this include variability in pre-operative measurements, effect of the posterior cornea, astigmatic effect of surgical wounds, intraoperative alignment, and postoperative alignment [4,5].
In standard biometry measurements, only the anterior surface of the cornea is measured, and it is assumed that the cornea’s curvature is uniform [6-11]. Biometry in individuals with astigmatism is inherently more imprecise due to the imperfect curvature of the cornea [4,5]. Thus, it is important to measure both the anterior and posterior surfaces of the cornea accurately. In fact, 76% of cataract surgery patients using toric IOLs experienced lens misalignment purely due to measurement error [12]. The effect of minimizing biometry measurement error is important for correcting astigmatism. The current gold-standard biometry device for cataract surgery is the IOLMaster 700 [6,13]. A new and increasingly popular biometry device available is the Pentacam AXL which evaluates corneal shape using Scheimpflug imaging [14]. Many practices have recently begun to use both IOLMaster 700 and Pentacam AXL as it is thought that repeated measurements using different devices may translate to a more successful outcome [4-6].
Previously, studies have compared standard IOL power measurements between Pentacam AXL and IOLMaster 700, finding small but clinically important differences [9-11,15]. However, to date no research has compared toric IOL suggestions by the two devices (ie., power, toric, and alignment). These lens calculations are critical given the prevalence of concurrent cataract and astigmatism, and the increasing use of toric IOLs for individuals with astigmatism. This study aims to investigate the agreement between the values of toric lens parameters as analyzed by these two devices.
Materials and Methods
This study was approved by the Queen’s University Health Sciences and Science Research Ethics Board (TRAQ #6037380) and conformed with the latest revision of the Declaration of Helsinki.
We conducted a retrospective chart review which enrolled 93 eyes from 62 patients who underwent cataract surgery and received a toric IOL between January and March 2022. All cataract surgeries were performed at an out-of-hospital Independent Health Facility comprising 5 surgeons. Surgically Induced Astigmatism (SIA) and incision axis were recorded for each surgeon. SIA was 0.25 for four of the five surgeons, and 0.3 for the fifth surgeon. Incision axis was 190º OD (Oculus Dexter) and 10º OS (Oculus Sinister) for four of the five surgeons, and 130 OU (Oculus Uterque) for the fifth surgeon. The lens models used by the surgeons were Alcon (Fort Worth, Texas, USA) Vivity (DFTx15), Alcon PanOptix Multifocal (TFNTx), and Alcon TORIC (SN6ATx).
Our study included patients 18 years or older undergoing cataract surgery with toric IOL with complete records and no previous ocular history, including laser eye surgery or corneal disease. All patients had preoperative biometry using both Pentacam AXL and IOLMaster 700, with a scan quality exceeding the manufacturer recommendation. Written informed consent was obtained from all included participants.
All patients had biometry measurements acquired using both IOLMaster 700 (Carl Zeiss Meditec, Jena, Germany) and Pentacam AXL (Oculus Optikgeräte GmbH, Wetzlar, Germany). The keratometry data from both devices was inputted into the ASCRS Online Barrett Toric Calculator and the suggested lens power (closest to plano), toricity (least amount of astigmatism even if axis flipped), and alignment were recorded. Additionally, the predicted refractive results based on the actual IOL used were collected. Finally, a followup visit was conducted 4-6 weeks post-operatively to assess the patients’ refractive results.
Our study contained three arms-IOLMaster 700 (using standard as opposed to total keratometry), Pentacam AXL with predicted posterior corneal astigmatism, Pentacam (P), and Pentacam AXL with measured posterior corneal astigmatism, Pentacam (p). For each study arm, we compared three primary outcome measures of IOL suggestions: Lens Power, Toric, and Alignment.
Pentacam (P), and Pentacam AXL with measured posterior corneal astigmatism, Pentacam (p). For each study arm, we compared three primary outcome measures of IOL suggestions: Lens Power, Toric, and Alignment.
Data analysis
Data analysis was performed using SPSS (Statistical Package for the Social Sciences) for Mac (Version 28). A Kolmogorov-Smirnov test was performed to examine the data for distribution normality. The outliers were excluded to ensure statistical validity. For biometry measurements, means and Standard Deviations (SD) were calculated, and a paired t-test was performed to evaluate statistically significant differences in keratometry and refractive data (continuous variables) between IOLMaster 700 and Pentacam AXL. Pearson correlations were performed between our primary outcome measures (ordinal variables) to assess their agreement. Figures were generated using Prism 8 (GraphPad, CA, USA).
Results
Participant characteristics are included in Table 1. A total of 93 eyes from 62 patients were included in the study. The sample consisted of 27 males (39 eyes) and 35 females (54 eyes). The mean age was 59 ± 10 years. Baseline keratometry data is also available in Table 1. Overall, IOLMaster 700 and Pentacam AXL showed excellent correlation for all keratometry measurements (Pearson>0.7 for all parameters). The mean power, toric, and alignment suggestions are presented in Table 2.
| Parameter | Value | ||
|---|---|---|---|
| Eyes (n) | 93 | ||
| Right (n) | 42 | ||
| Male/Female (%) | 42/58 | ||
| Age (years) | 59 ± 10 | ||
| Lens used | - | ||
| DFT | 29 | ||
| TFNT | 53 | ||
| SA6AT | 11 | ||
| Pre-op Sphere (D) | -2.36 ± 4.56 | ||
| Pre-op Cylinder (D) | 1.16 ± 0.87 | ||
| Pre-op SE (D) | -1.78 ± 4.46 | ||
| Biometry Parameter | IOL Master 700 | Pentacam AXL | Pearson |
| AL (mm) | 24.07 ± 1.71 | 24.06 ± 1.70 | 1 |
| ACD (mm) | 3.29 ± 0.37 | 3.31 ± 0.36 | 0.99 |
| LT (mm) | 4.36 ± 0.37 | N/A | N/A |
| WTW (mm) | 12.09 ± 0.39 | 11.74 ± 0.39 | 0.95 |
| Average K (mm) | 44.19 ± 1.63 | 44.12 ± 1.62 | 0.99 |
| PCA (D) | N/A | 0.29 ± 0.16 | N/A |
Note: Values presented as Mean ± Standard Deviation. AL: Axial Length; ACD: Anterior Chamber Depth; LT: Lens Thickness; K: Keratometry; PCA: Posterior Corneal Astigmatism; D: Diopters; SE: Spherical Equivalent.
Overall, IOLMaster 700 suggested lower IOL power than Pentacam AXL (18.9 ± 5.4 vs. 19.1 ± 5.5 D, p<0.001). As demonstrated in Figure 1A, the suggested IOL power was identical between both devices in 54% of eyes. The power suggestions differed by ± 0.5D in 40% of eyes. Thus, IOLMaster 700 and Pentacam AXL only differed by over 0.5D in 6% of eyes in their IOL power suggestions. The power suggestions were identical in 100% of cases between both arms of Pentacam AXL.
Toric suggestions also showed excellent correlation between the three study arms (Pearson>0.81 between arms). The toric suggestions between IOLMaster 700, Pentacam AXL (P) and (M) were not statistically significant (2.9 ± 1.0 step, 2.8 ± 1.1, and 2.8 ± 1.0, respectively). As demonstrated in Figure 1B, toric suggestions were identical between IOLMaster 700 and Pentacam AXL in 67% and differed by ± 1 step in 33% of eyes when posterior corneal astigmatism was predicted. However, when posterior corneal astigmatism was measured, toric suggestions were only identical in 57% of eyes and differed by ± 1 step in 43%. Toric suggestions were identical between both Pentacam AXL study arms in only 73% of eyes. These results are presented in Figure 1. The differences in toric suggestions showed no correlation with pre- operative astigmatism (Pearson=-0.13).
| Study arm | Power (D) | Toric | Alignment (º) |
|---|---|---|---|
| IOLMaster 700 | 18.9 ± 5.4 | 2.9 ± 1.0 | 97 ± 54 |
| Pentacam (P) | 19.1 ± 5.5 | 2.8 ± 1.1 | 98 ± 53 |
| Pentacam (M) | 19.1 ± 5.5 | 2.8 ± 1.0 | 99 ± 53 |
Note: P: Pentacam; PCA: Pentacam Predicted; M: Pentacam: PCA: Pentacam Measured.
IOL alignment suggestions also showed excellent statistical correlation between the three study arms (Pearson >0.98 between arms). Alignment suggestions were identical between IOLMaster 700 and Pentacam (P) in 9% of eyes compared to only 3% of eyes for a comparison with Pentacam (P). Alignment suggestions differed by ± 3º in 42% of eyes when comparing IOLMaster 700 and with Pentacam (P), compared to 28% of eyes when compared with Pentacam (P). This is outlined in Table 3.
| Alignment differences | IOLMaster 700 vs. Pentacam AXL (P) | IOLMaster 700 vs. Pentacam AXL (M) | Pentacam (P) vs. Pentacam AXL (M) |
|---|---|---|---|
| Exactly 0º | 9 | 3 | 13 |
| ± 1º | 19 | 17 | 35 |
| ± 2º | 28 | 27 | 53 |
| ± 3º | 42 | 28 | 69 |
| ± 4º | 51 | 33 | 84 |
| ± 5º | 55 | 38 | 90 |
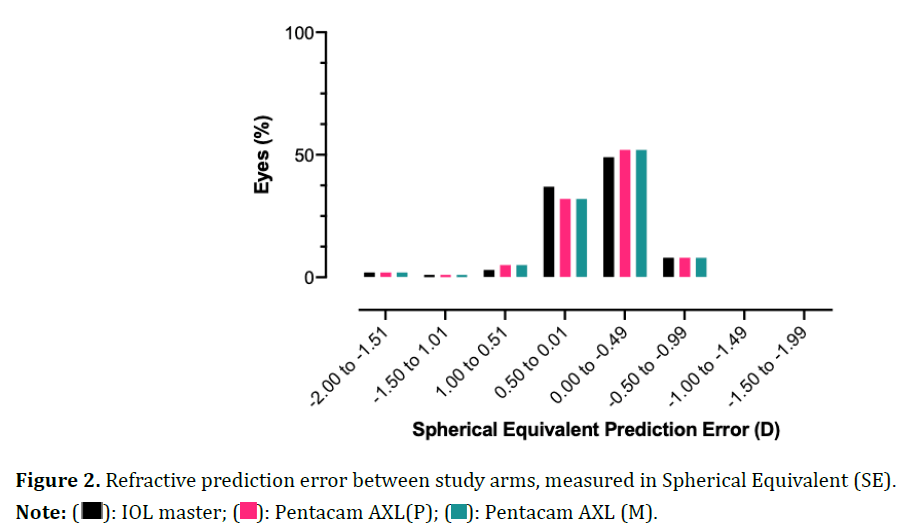
The postoperative refractive outcomes are illustrated in Figure 2. The mean absolute error between predicted and actual refraction was very similar between IOLMaster 700 and Pentacam AXL, with an error of ± 0.5D in 82-84% of eyes.
Discussion
This study aimed to compare two commonly used biometry devices used for preoperative measurements of cataract surgery, namely the IOLMaster 700 and the Pentacam AXL. Given these devices are often used in combination, we sought to address whether there were any differences between their toric IOL suggestions for power, toric, and alignment, which could potentially impact surgical outcomes.
The study found that keratometry data was well correlated between the two devices, and the predicted refraction error was within 0.5D for both devices in almost 90% of cases. These results are in line with other studies that have compared these devices [9,11].
The clinically meaningful IOL suggestions for toric lenses are power, toric, and alignment. For IOL power, we found an overall 0.2D difference in the suggested IOL power between IOLMaster 700 and Pentacam AXL. While small, this can translate into a clinically meaningful difference particularly with presbyopia-correcting IOLs. Secondly, the results from this study showed excellent complementarity in the toric suggestions between both devices. In fact, toric suggestions were identical in 2/3 cases and were within 1 step in almost all cases when comparing IOLMaster 700 with Pentacam AXL with predicted posterior corneal astigmatism. The agreement between devices was slightly decreased when the posterior cornea was measured with the Pentacam AXL, but still yielded excellent complementarity. Finally, the study found that the alignment suggestions were well statistically correlated (r=0.98). Clinically, however, there were meaningful differences between the suggestions from both devices. The suggestions were only identical between both devices in 3%-9% of cases, and within a difference of 5º in 38%-55% of cases. Interestingly, the alignment suggestions were better correlated when posterior corneal astigmatism was measured using Pentacam AXL. This is an important finding as previous studies have shown that measuring the posterior corneal astigmatism with Pentacam can lead to lower residual astigmatism prediction errors [16-18].
The variability in suggestions for IOL alignment may be attributed to differences in how the two devices measure the eye, with the Pentacam AXL using Scheimpflug cameras while the IOLMaster 700 emits infrared lights to calculate the same biometry parameters. Additionally, alignment is also a more variable outcome, measured on a scale of 0-180, whereas toric is measured in steps, and the range in this study was 0-7. With that being said, the discrepancy in alignment suggestions is clinically important as each degree of misalignment results in a 3% reduction in astigmatism correction [4,5].
Due to the retrospective nature of this study, there are some limitations. This study could not directly compare the accuracy of each device, limiting its applicability. In fact, the surgeons all used the IOLMaster 700’s suggestions when planning their surgery (mainly using the Pentacam AXL as a confirmatory test), preventing us from performing vector analysis and limited the comparison of outcomes between devices. Additionally, the postoperative refractive data did not include lens alignment, which is a surrogate measure for surgical success.
Conclusion
This study compared toric IOL calculations between the IOLMaster 700 and the Pentacam AXL and found that both devices showed statistically excellent correlation for power, toricity, and alignment suggestions. However, there were potentially clinically meaningful differences in alignment suggestions. These outcomes improve our knowledge on the complementarity of both devices for toric IOLs. Future prospective studies are needed to determine which device was more accurate in achieving astigmatism correction.
Acknowledgments
The authors report no conflicts of interest in this work.
Funding
William Samuel Thomas Connell Memorial Fund was a research studentship received by MRG. The sponsor had no role in the design or conduct of this research.
Author Contributions
All authors contributed to the study conception and design. Data collection and analysis was performed by Mohamed R. Gemae. The first draft of the manuscript was written by Mohamed R. Gemae and Davin Johnson. All authors read and approved the final manuscript.
References
- Ferrer-Blasco T, Montés-Micó R, Peixoto-de-Matos SC, González-Méijome JM, Cerviño A. Prevalence of corneal astigmatism before cataract surgery. J Cataract Refract Surg 2009;35(1):70-75.
[Crossref] [Google Scholar] [Pubmed]
- Hoffmann PC, Hütz WW. Analysis of biometry and prevalence data for corneal astigmatism in 23 239 eyes. J Cataract Refract Surg 2010;36(9):1479-1485.
[Crossref] [Google Scholar] [Pubmed]
- Holland E, Lane S, Horn JD, Ernest P, Arleo R, Miller KM. The AcrySof Toric intraocular lens in subjects with cataracts and corneal astigmatism: A randomized, subject-masked, parallel-group, 1-year study. Ophthalmology 2010;117(11):2104-2111.
[Crossref] [Google Scholar] [Pubmed]
- Ahmed II, Rocha G, Slomovic AR, Climenhaga H, Gohill J, Grégoire A, et al. Visual function and patient experience after bilateral implantation of toric intraocular lenses. J Cataract Refract Surg 2010;36(4):609-616.
[Crossref] [Google Scholar] [Pubmed]
- Kaur M, Shaikh F, Falera R, Titiyal JS. Optimizing outcomes with toric intraocular lenses. Indian J Ophthalmol 2017;65(12):1301-1313.
[Crossref] [Google Scholar] [Pubmed]
- Sahin A, Hamrah P. Clinically relevant biometry. Curr Opin Ophthalmol 2012;23(1):47-53.
[Crossref] [Google Scholar] [Pubmed]
- Lee AC, Qazi MA, Pepose JS. Biometry and intraocular lens power calculation. Current opinion in ophthalmology. 2008;19(1):13-17.
[Crossref] [Google Scholar] [Pubmed]
- Sayed KM, Alsamman AH. Interchangeability between Pentacam and IOLMaster in phakic intraocular lens calculation. Eur J Ophthalmol 2015;25(3):202-207.
[Crossref] [Google Scholar] [Pubmed]
- Helmy T, Ali H, Sameh M, EL-zankalony YA. Comparative study between Pentacam and IOL master in measuring anterior segment parameters in eyes of egyptian individuals. Med J Cairo Univ 2019;87:4087-4092.
- Muzyka-Woźniak M, Oleszko A. Comparison of anterior segment parameters and axial length measurements performed on a Scheimpflug device with biometry function and a reference optical biometer. Int Ophthalmol 2019;39:1115-1122.
[Crossref] [Google Scholar] [Pubmed]
- Wang ZY, Yang WL, Li DJ, Chen W, Zhao Q, Li YF, et al. Comparison of biometry with the Pentacam AXL, IOLMaster 700 and IOLMaster 500 in cataract patients. (Zhonghua yan ke za zhi) Chinese J Ophthalmol 2019;55(7):515-521.
[Crossref] [Google Scholar] [Pubmed]
- Potvin R, Kramer BA, Hardten DR, Berdahl JP. Toric intraocular lens orientation and residual refractive astigmatism: An analysis. Clin Ophthalmol 2016:1829-1836.
[Crossref] [Google Scholar] [Pubmed]
- Rajan MS, Keilhorn I, Bell JA. Partial coherence laser interferometry vs conventional ultrasound biometry in intraocular lens power calculations. Eye (Lond) 2002;16(5):552-556.
[Crossref] [Google Scholar] [Pubmed]
- Motlagh MN, Moshirfar M, Murri MS, Skanchy DF, Momeni-Moghaddam H, Ronquillo YC, et al. Pentacam® corneal tomography for screening of refractive surgery candidates: A review of the literature, part I. Med Hypothesis Discov Innov Ophthalmol 2019;8(3):177-203.
[Google Scholar] [Pubmed]
- Lee BW, Galor A, Feuer WJ, Pouyeh B, Pelletier JS, Vaddavalli PK, et al. Agreement between Pentacam and IOLMaster in patients undergoing toric IOL implantation. J Refract Surg 2013;29(2):114-120.
[Crossref] [Google Scholar] [Pubmed]
- Park DY, Lim DH, Hwang S, Hyun J, Chung TY. Comparison of astigmatism prediction error taken with the Pentacam measurements, Baylor nomogram, and Barrett formula for toric intraocular lens implantation. BMC Ophthalmol 2017;17:1-9.
[Crossref] [Google Scholar] [Pubmed]
- Reitblat O, Levy A, Kleinmann G, Abulafia A, Assia EI. Effect of posterior corneal astigmatism on power calculation and alignment of toric intraocular lenses: Comparison of methodologies. J Cataract Refract Surg 2016;42(2):217-225.
[Crossref] [Google Scholar] [Pubmed]
- Davison JA, Potvin R. Refractive cylinder outcomes after calculating toric intraocular lens cylinder power using total corneal refractive power. Clin Ophthalmol 2015:1511-1517.