Case Report - Archives of Clinical and Experimental Surgery (2022)
Development of Disseminated Tuberculosis in a Non- Immune Compromised Patient after COVID-19 Infection: A Case Report
Ensiyeh Rahimi*, Sara Ghaderkhani and Yousef JamshidiEnsiyeh Rahimi, Department of Infectious Diseases, Imam Khomeini Hospital, Tehran University of Medical Science, Tehran, Iran, Email: drsaikalyanguptha@gmail.com
Received: 03-Jan-2022, Manuscript No. EJMACES-22-50919; Editor assigned: 05-Jan-2022, Pre QC No. EJMACES-22-50919 (PQ); Reviewed: 19-Jan-2022, QC No. EJMACES-22-50919; Revised: 24-Jan-2022, Manuscript No. EJMACES-22-50919 (R); Published: 31-Jan-2022
Abstract
Background: COVID-19 pandemic has had complications and has changed the pattern of disease incidence. COVID-19 affects the immune system. We present a case of disseminated Tuberculosis (TB) in non-immunocompromised person with a history of COVID-19 infection.
Case presentation: A 25 year old woman had a history of mild COVID-19 infection 3 months ago. Then the complaint of back pain began and the headache was added 1 month later. Gradually, the patient’s headache intensified. Finally, the patient was admitted with decreased level of consciousness, delirium and focal neurological symptoms. The work up confirmed disseminated TB contains of miliary pulmonary TB, TB meningitis and TB spondylodiscitis. The patient gradually improved on anti- tuberculosis treatment.
Conclusion: There may be an association between disseminated TB infections following COVID- 19 infection.
Keywords
Tubercuflosfis; Surgery Spondyflodfiscs; COVID-19
Introduction
Background
Tuberculosis is a contagious disease that is one of the top 10 causes of death worldwide and the leading cause of death from a single infectious agent. In 2019, about 10 million people developed TB and 1.4 million died.
MTB is transmitted from person to person via the airborne route. After inhalation, the droplet nucleus is carried down the bronchial tree and implants in a respiratory bronchiole or alveolus. Whether or not inhaled tubercle bacilli establish an infection depends on both host and microbial factors [1]. Miliary TB is a type of disseminate TB that results from lymphatic and hematologic spread from a TB focus and is very fatal if not treated in time [2]. In countries with low incidence, delayed diagnosis and treatment, increase mortality [3].
COVID-19 pandemic has had complications and has changed the pattern of disease incidence. COVID-19 affects the immune system. TB reactivation can be explained by T-cell depletion resulting from COVID-19 infection [4-6]. Here, we describe a patient who was diagnosed with the disseminated TB and history of COVID-19 infection.
Case Presentation
A 25-year-old Iranian female with complaints of headache and loss of consciousness was hospitalized on 2 Jun 2021. She presented with history of headache last 2 months. The patient’s headaches were mostly in the frontal lobes and parietal lobes. She had frequent outpatient visits to the physician for headaches and has taken analgesics during this time.
The patient was non-immunocompromised person. She had a history of COVID-19 infection 3 months ago. Her COVID-19 disease was mild. She had flu-like syndrome and lost her sense of smell and taste. She didn’t have COVID-19 pulmonary involvement and was not admitted to a hospital. Then the complaint of back pain began. The patient’s back pain was on the thoracic vertebrae. The patient back pain has continued until now.
The patient’s headache had worsened from 2 weeks before the admission. Finally, she came to the hospital with a severe headache. She had complaints of decreased level of consciousness, nausea, vomiting, diplopia, back pain and bladder incontinency. She had acute onset of lower limb weakness on day prior to the admission that becomes unable to even stand independently. Patient did not have any medical problem previously. She did not have any cough. There was no family history of TB. She has lost 5 kg in the last month. She had moved from village to city 22 years ago.
On admission, she was lethargic and confused. She had delirium. On physical examination she was afebrile. Signs of meningeal irritation were present. Lower limbs power decreased (4/5). She had nystagmus on eye examination.
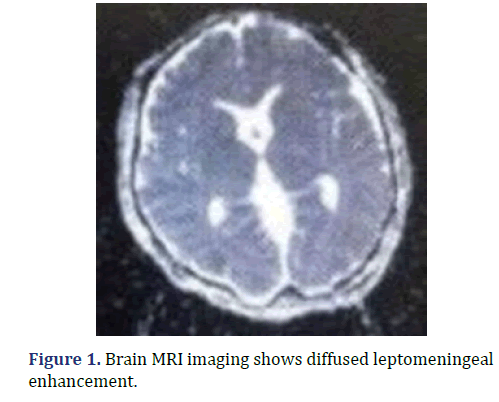
Brain Magnetic Resonance Images (MRI) showed diffused leptomeningeal enhancement. Mild hydrocephaly was seen too. There was abnormal signal area with restriction in splenium of corpus callosum without enhancement (Figure 1).
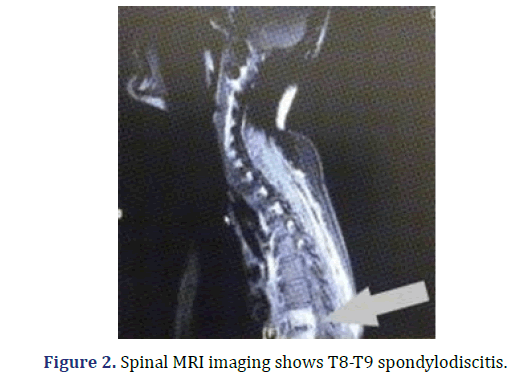
Spinal MRI showed abnormal signal intensity with enhancement in T8-T9 disc space, adjacent end plates, bodies and posterior elements and small part of body of T10 associated prevertebral soft tissue edema and enhancement (Figure 2).
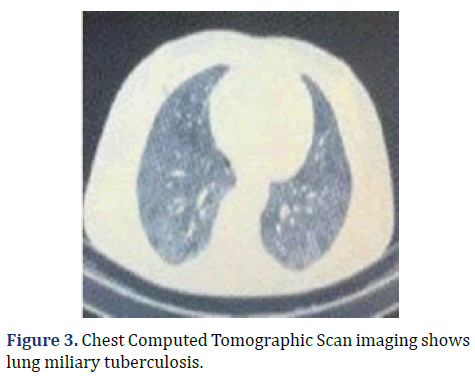
On chest computed tomographic scan, poorly spread nodularity was seen throughout the lungs suggesting miliary tuberculosis. Multiple lymphadenopathies were seen in the left axillary and mediastinum that some of them had calcifications (Figure 3).
Laboratory investigations showed elevated WBC in Cerebral Spinal Fluid (60% lymphocyte), high CSF protein and low glucose. Mycobacterium tuberculosis detected with Polymerase Chain Reaction (PCR) of Cerebral Spinal Fluid (CSF) ( Rifampin resistance not detected with the Expert MTB/RIF assay. CMV, EBV, HSV1, 2 and VZV didn’t detect with PCR of CSF. White blood cell count was 5,900 cells/mm3, (90% neutrophils, 8% lymphocytes). C-reactive protein level was 21 mg/dl. Erythrocyte Sedimentation Rate (ESR) level was 31 mm/h. HIV serology was negative. Liver function tests parameters were containing: Aspartate transaminase (AST) 57 U/L, Alanine Transaminase (ALT) 53 U/L, Alkaline Phosphatase (ALP) 264 U/L, serum bilirubin total 0.8 mg/dl and direct 0.5 mg/dl. SARS CoV2 RT-PCR from nasopharyngeal and throat swabs was negative.
Patient started on anti-tuberculosis drugs and steroid. She was started on isoniazid 300mg, rifampin 600mg, pyrazinamide 1200mg and ethambutol 825mg once daily. According to objective neurological findings, prednisolone 80 mg/day was required, which was gradually tapered and discontinued through 6 weeks. Analysis of Cerebral Spinal Fluid (CSF) on the eighth day of treatment was better. Post treatment showed significant neurological improvement. The patient’s consciousness gradually improved during the first week of treatment. Nystagmus and diplopia was improved during the second week. The patient`s headache subsided and was mostly after waking up during the third week. Delirium was completely gone in the third week. From the fourth week, force of her lower limbs improved and she was able to stand independently. Despite T8-T9 spondylodiscitis, the patient had not neurological deficits and cord compression. According to the neurosurgeon consulting, she did not need to surgery and was treated with medical treatment. The patient’s liver function tests increased at the beginning of treatment but gradually decreased after 2 weeks of treatment (Table 2).
The increase in liver function tests was less than 5 fold normal and the patient did not show signs and symptoms of acute hepatitis, so the medication continued. On day 18th of admission, the patient was discharged home in good general condition. The patient was prescribed anti tuberculous treatment for total duration of 12 months with a follow up appointment at the TB clinic. She received prednisolone for first 6 weeks’ duration and her prednisolone decreased weekly.
Discussion
An interesting point in this case is the disseminated TB in a young woman with no history of the disease and only looking for a mild COVID-19 infection. The patient had a disseminated TB with military TB pulmonary, TB meningitis and TB spondylodiscitis. Our patient was not immunocompromised. She only had a history of mild COVID-19 infection. The patient received only a few outpatient doses of dexamethasone due to the non-hospitalization. The complaint of back pain began after COVID-19 infection. No underlying cause for her disseminated TB was found. There may be an association between disseminated TB infections following COVID- 19 infection. Several studies have reported that CD4 T cells play an essential role in defense against MTB [7]. In this study, 76% COVID-19 infected patients had significant depletion in their T-cell lymphocyte counts [5]. Both CD4 and CD8 counts were severely reduced, and the surviving T cells appeared to be dysfunctional. This T cell depletion and exhaustion may promote latent TB to active TB. In acute COVID-19 infection, peripheral lymphocyte especially T lymphocyte are depleted. CD8 T lymphocytes will be recovered within 2–3 months and CD4 T lymphocytes will return to normal within a year [8].
Few studies have linked TB reactivation to viral infections. Few studies have1 demonstrated the association between active TB and COVID-19 infection or a flare up of 4 TB 5 after COVID-19 infection had reported patients with concurrent COVID-19 infection with active TB infection study coinfection TB an COVID-19 presented with median time of 4 days. They thought that the overlap of symptoms between the two diseases led to diagnosis of tuberculosis reported a patient with possible peritoneal TB who progressed to miliary pulmonary TB after COVID- 19 infection [9].
Most cases of tuberculosis have been seen after sever COVID-19 infection but in our study, tuberculosis was looking for a mild COVID-19 infection.
In endemic areas of tuberculosis, it is important to pay attention to patient’s symptoms after COVID-19 infection such as weakness, headache and weight loss. As this case have had weakness, headache, and weight loss for few months. These symptoms may be confused with post COVID-19 syndrome and lead to delays the diagnosis and treatment of tuberculosis.
Given that the COVID-19 infection is a risk factor for TB reactivation. In COVID- 19 pandemic, early identification of TB patients is important for treatment and infection control [10].
Conclusion
Due to wide patient involvement, complete and timely treatment of the patient is important. The success of drug treatment depends upon many factors. Some studies have found an increased risk of relapse among patients with signs of more extensive disease. The patient was prescribed 12 months of anti-tuberculosis treatment. Tuberculosis treatment requires multiple drugs be given for several months. It is difficult for the patient to tolerate the treatment due to the possibility of drug side effects. The patient should be aware of the importance of taking the medication correctly. It is very important that the patient be involved in making decisions concerning treatment supervision and overall care. International standards also emphasize the importance of using patient centered approaches to the treatment of tuberculosis.
References
- Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 2018;68:394-424.
[Crossref] [Google scholar] [Pubmed]
- Leporrier J, Maurel J, Chiche L, Bara S, Segol P, Launoy GA .Population-based study of the incidence, management and prognosis of hepatic metastases from colorectal cancer. Br J Surg 2006;93:465-474.
[Crossref] [Google schlor] [Pubmed]
- Riihimäki M, Hemminki A, Sundquist J, Hemminki K. Patterns of metastasis in colon and rectal cancer. Sci Rep 2016;6:29765.
[Crossref] [Google schlor] [Pubmed]
- Liu LX, Zhang WH, Jiang HC. Current treatment for liver metastases from colorectal cancer. World J Gastroenterol 2003;9:193-200.
[Crossref] [Google schlor] [Pubmed]
- Torzilli G, Adam R, Vigano L. Surgery of colorectal liver metastases: pushing the limits. Liver Cancer 2016;6:80-89.
[Crossref] [Google schlor] [Pubmed]
- Tomlinson JS, Jarnagin WR, DeMatteo RP. Actual 10-year survival after resection of colorectal liver metastases defines cure. J Clin Oncol 2007;25:4575-4780.
[Crossref] [Google schlor] [Pubmed]
- De Jong MC, Pulitano C, Ribero D. Rates and patterns of recurrence following curative intent surgery for colorectal liver metastasis: An international multi-institutional analysis of 1669 patients. Ann Surg 2009;250:440-448.
[Crossref] [Google schlor] [Pubmed]
- Abdalla EK, Vauthey JN, Ellis LM. Recurrence and outcomes following hepatic resection, radiofrequency ablation, and combined resection/ablation for colorectal liver metastases. Ann Surg 2004;239:818-825.
[Crossref] [Google schlor] [Pubmed]
- Mavros MN, de Jong M, Dogeas E, Hyder O, Pawlik TM. Impact of complications on long-term survival after resection of colorectal liver metastases. Br J Surg 2013;100:711-718.
[Crossref] [Google schlor] [Pubmed]
- Abbas S, Lam V, Hollands M. Ten-year survival after liver resection for colorectal metastases: systematic review and meta-analysis. ISRN Oncol 2011:763245.
[Crossref] [Google schlor] [Pubmed]
Copyright: © 2022 The Authors. This is an open access article under the terms of the Creative Commons Attribution NonCommercial ShareAlike 4.0 (https://creativecommons.org/licenses/by-nc-sa/4.0/). This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.