Research Article - Archives of Clinical and Experimental Surgery (2024)
Endoscopic Cystogastrostomy Versus Open Cystogastrostomy Drainage for Pancreatic Pseudocyst: A Comparative Study
Priyanka RK, Sharanabasavaraj Javali*, Prashant Kanni Y, Shruti Sahu and Mohan LNSharanabasavaraj Javali, Department of General Surgery, Vydehi Institute of Medical Sciences and Research Centre, Bangalore, India, Tel: +919902354299, Email: dr.s.c.javali@gmail.com
Received: 03-Jan-2024, Manuscript No. EJMACES-24-124395; Editor assigned: 08-Jan-2024, Pre QC No. EJMACES-24-124395 (PQ); Reviewed: 22-Jan-2024, QC No. EJMACES-24-124395; Revised: 29-Jan-2024, Manuscript No. EJMACES-24-124395 (R); Published: 05-Feb-2024
Abstract
Introduction: Pancreatic pseudocyst is a localized peripancreatic fluid collection that results from pancreatic inflammation due to pancreatitis, trauma or ductal obstruction due to stricture or stone. Pancreatic pseudocyst drainage through the stomach or small intestine can be performed by open drainage, considered as standard treatment, and the endoscopic approach is less invasive than open surgery. This study aimed to compare the efficacy of open and endoscopic cystogastrostomy for the drainage of pancreatic pseudocysts.
Materials and methods: Thirty patients diagnosed (based on CECT (Contrast-Enhanced Computed Tomography)) with pancreatic pseudocysts (size being>6 cm) requiring intervention were considered. Patients were divided into 2 groups; Group 1 consisted of patients planned for open cystogastrostomy drainage and Group 2 consisted of patients planned for endoscopic ultrasound-guided Drainage. Patients were followed up for 6 months after discharge to record any complications.
Results: There was no statistically significant difference found between the two groups with respect to age, gender, presence of co-morbidities, presenting symptoms and signs, location of pseudocyst, presence or absence of complication during the procedure and hospital stay (p>0.05). The complications were observed in 26.7% and 46.15% of patients in groups 1 and 2 respectively. In follow-up, 6 patients in group 1 and one in group 2 exhibited complications. However, this was not statistically significant (p=0.08). No recurrence was seen in either group during the 6-month follow-up period. Duration of hospital stay was significantly lower in group 2 compared to group 1 (p<0.05).
Conclusion: Both endoscopic and surgical drainage procedures, are equal in terms of efficacy and success rates; the use of ultrasound guidance for the endoscopic procedures is probably attributable to the good success rate. However, endoscopic drainage should be considered the first line of management for pancreatic pseudocysts when available owing to the lower treatment cost, lesser duration of hospitalisation and lesser morbidity associated with the procedure in the long run.
Keywords
Pancreas; Comparative efficacy; Endoscopic ultrasound guided cystogastrostomy; Open cystogastrostomy; Pancreatic pseudocyst
Introduction
Pancreatic pseudocyst is a small accumulation of peripancreatic fluid resulting from trauma and ductal obstruction by stricture or stone, pancreatic inflammation brought on by pancreatitis. Because it lacks an epithelial coating, it is not a real cyst. A fibrous or granulation tissue wall encloses it [1]. Symptoms of pancreatic pseudocysts can include pain, satiety, upper gastrointestinal haemorrhage, nausea, and vomiting. They can also be asymptomatic. Approximately 2 to 6 weeks are needed for pancreatic pseudocysts to mature, and during this time, 33% of cysts are anticipated to clear on their own. However, due to potential problems such infection, bleeding, and cyst rupture, a significant number of persistent cysts need to be treated. Pancreatic pseudocysts should only be drained in cases when the patient exhibits symptoms, the pseudocyst is large (>6 cm), growing quickly, or it is connected with problems. Pancreatic pseudocyst drainage can be accomplished through stomach or small intestine. Open, endoscopic, or laparoscopic procedures can all be used for drainage. Although surgical drainage is still the preferred method for treating pseudocyst drainage, endoscopic drainage should be given priority due to its reasonable success rate [2]. The advantage of using an endoscopic method over open surgery is that it is less invasive. Several publications have contrasted endoscopic versus surgical methods for Pancreatic Pseudo Cyst (PPC). The endoscopic group has been compared with surgical cystogastrostomy or cystojejunostomy, but many of these studies show a significant amount of heterogeneity. There are various surgical techniques, and none of them have a gold standard [3]. This study compares the efficacy of open and endoscopic cystogastrostomy for drainage of Pancreatic Pseudocysts in our institution.
Materials and Methods
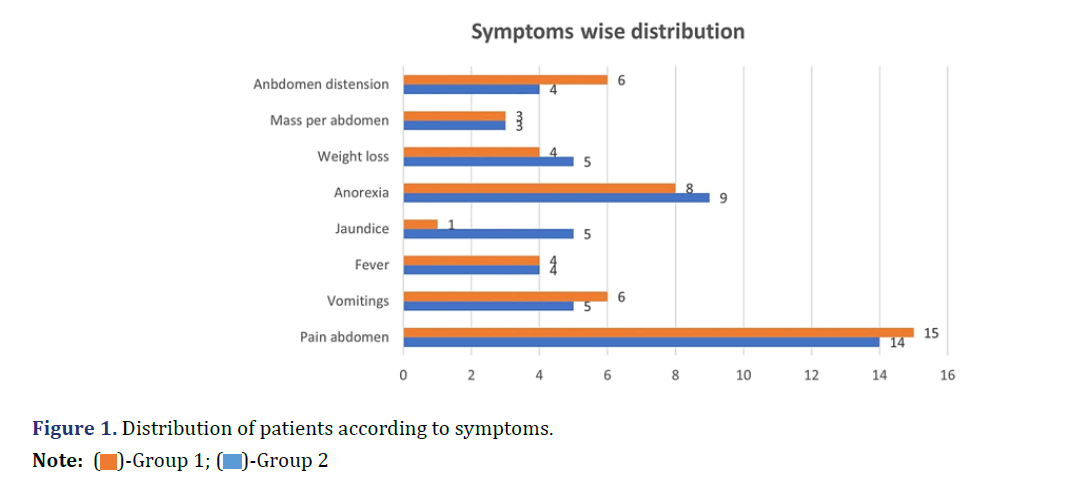
This prospective comparative study consists of Thirty diagnosed cases with pancreatic pseudocyst and requiring intervention at Vydehi Institute of Medical Sciences and Research Centre, Bangalore, during the period of 2019 to 2021. Patients aged between 18 to 80 years, with acute and chronic pancreatitis with pseudocyst, persistence of Pseudocyst for more than 6 weeks, and pseudocyst of size greater than 6 cm in diameter were included. Patients with pregnancy, multiple pseudocysts, comorbidities with American Society of Anesthesiology (ASA) grade IV, associated with pancreatic necrosis, cysts in the pancreatic tail and not willing to participate were excluded. Written informed consent was obtained from all the study participants after obtaining approval and clearance from the Institutional Ethics Committee (VIEC/2019/ APP/176 dated 14th November 2019) Patients diagnosed with pancreatic pseudocyst (Contrast- Enhanced Computed Tomography (CECT) abdomen) and requiring intervention were divided into two groups. Patients visiting the general Surgery department were allocated for Open cystogastrostomy drainage and were considered in Group 1(n=15) and Patients visiting the Medical Gastroenterology department were planned for Ultrasound-guided Endoscopic Cystogastrostomy and were considered in Group 2 (n=15). Patients’ signs, symptoms and size of the pseudocyst on CECT abdomen were recorded (Figure 1).
The predetermined cost for each procedure was considered. Intra and immediate (within 24 hours) postprocedure complications were recorded. Cyst wall in both the management options was sent for histopathological examination to rule out carcinoma. Patients were monitored post-procedure in the hospital and complications, if any were recorded. Number of days of hospitalisation was recorded until the patient was stable and discharged. Patients were followed up for 6 months after discharge to record any complications. The collected data was analysed using SPSS version 22.0. Categorical data was represented in the form of Frequencies and proportions. The chi-square test or Fischer’s exact test (for 2 × 2 tables only) was used as a test of significance for qualitative data. Continuous data was represented as mean and standard deviation. An Independent t-test was used as a test of significance to identify the mean difference between two quantitative variables results The mean difference of age was not statistically significant between the two groups. Male participants were common in both study groups. In Group 1, 8 patients had co-morbidities and in Group 2, 4 patients had comorbidities. There was no significant statistical difference (p=0.136) observed between the 2 groups with respect to the presence of co-morbidities. Diabetes mellitus was found to be a predominant comorbidity in the study. 5 patients in Group 1 and 2 patients in Group 2 had DM (Diabetes Mellitus). Out of the 5 patients in Group 1 with DM, 1 patient was found to have SSI as a complication during the post-operative period. There was no statistically significant difference found between groups with respect to any of the aetiology (p>0.05) (Tables 1 and 2).
| Group 1 | Group 2 | ||||
|---|---|---|---|---|---|
| Variables | Frequency | Percentage | Frequency | Percentage | p-value |
| Age | 40.80 ± 11.79 | 35.53 ± 15.29 | 0.301 | ||
| Gender | |||||
| Male | 10 | 66.7% | 12 | 80% | 0.682 |
| Female | 5 | 33.3% | 3 | 20% | |
| Status of comorbidities | |||||
| Present | 8 | 53.3% | 4 | 26.7% | 0.136 |
| Absent | 7 | 46.7% | 11 | 73.3% | |
| Etiological distribution | |||||
| Trauma | 2 | 13.3% | 2 | 13.3% | 1 |
| Alcohol | 7 | 46.7% | 8 | 53.3% | 1 |
| Biliary pancreatitis | 5 | 33.3% | 3 | 20% | 0.682 |
| Group 1 | Group 2 | ||||
|---|---|---|---|---|---|
| Variables | Frequency | Percentage | Frequency | Percentage | p-value |
| Clinical signs | |||||
| Tenderness | 14 | 93.3% | 12 | 80% | 0.598 |
| Abdomen mass | 6 | 40% | 8 | 53.3% | 0.715 |
| Ascites | 4 | 26.7% | 3 | 20% | 1 |
| Location of pseudocyst in pancreas | |||||
| Body | 7 | 46.7% | 7 | 46.7% | 0.64 |
| Head | 5 | 33.3% | 1 | 6.7% | |
| Head and Body | 1 | 6.7% | 4 | 26.7% | |
| Head and neck | 1 | 6.7% | 2 | 13.3% | |
| Head, Neck, Uncinate Process | 1 | 6.7% | - | - | |
| Neck and body | - | - | 1 | 6.7% | |
| Complication during hospital stay | |||||
| Absent | 11 | 73.3% | 7 | 53.85% | 0.283 |
| Present | 4 | 26.7% | 6 | 46.15% | |
| Complication during follow-up | |||||
| Absent | 9 | 64.3% | 12 | 92.3% | 0.08 |
| Present | 5 | 35.7% | 1 | 7.7% | |
| Duration of hospital stay | 12.33 ± 2.52 | - | 6.40 ± 2.694 | - | 0.001 |
Results and Discussion
Pancreatic pseudocysts are commonly encountered after acute and chronic pancreatic inflammation and also lead to commonly occurring cystic lesions of pancreas. Pancreatic Pseudocysts may be asymptomatic or may present with a variety of symptoms such as pain, satiety, upper gastrointestinal bleeding, nausea and vomiting. This study aimed to evaluate open versus endoscopic cystogastrostomy drainage for pancreatic pseudocyst. Patient age, gender, presenting complaints, presence or absence of comorbidities were matched in both groups and there was no statistically significant difference noted between the two groups in our study. It was noted that there was no statistically significant difference observed with respect to aetiology in either group which is comparable to other studies done before. In a study by Saluja et al. comparing surgical and endoscopic cystogastrostomy drainage procedures, it was found that the surgical group had significantly higher rates of technical success (20/20 vs. 27/35) and fewer complications (2/20 vs. 10/35) as well as a shorter hospital stay (5 days vs. 6.5 days), 17% of patients converted to surgical drainage [2]. According to a study by Varadarajulu et al. that compared endoscopic and surgical cystogastrostomy for pancreatic pseudocyst drainage, at the end of a 24-month follow-up period, no subjects had pseudocyst recurrence, however, one instance had been surgically treated [4]. The two 4 of 6 groups. Endoscopic drainage of pancreatic pseudocysts had a great success rate, general side effects, and a recurrence rate comparable to that seen with surgical treatment, according to a systematic review and meta- analysis. However, due to its lower expenses and shorter hospital stay, this procedure is favoured for the draining of pancreatic pseudocysts [5]. Teoh et al. stated that endoscopic ultrasound-guided drainage is effective in pancreatic pseudocyst drainage situated adjacent to the stomach and duodenum [6]. In the present study, although the cost for both procedures was similar it was found that the overall treatment cost in the case of endoscopic group was lower than in the surgical group. This was mainly attributed to the longer duration of hospital stay and medications in the surgical group. Around six patients in our Surgical group came with complications during the follow-up period: 1 patient with Pancreaticopleural fistula was managed with decortication, 1 patient with persistent pain abdomen was managed with celiac plexus block, 1 patient with subacute intestinal obstruction was managed conservatively, 1 patient with Ascites was worked up and it was found that cirrhosis was the cause and was managed by the medical team, 1 patient had persistent cyst and 1 patient presented with Incisional Hernia and was managed with Open Mesh Hernioplasty.
Out of these six patients, five were attributable to the procedure and the majority required intervention. The patient with Ascites was not considered a complication of the procedure. While only one patient in the endoscopic group had complaints in the follow- up period and was managed without intervention. There was no recurrence seen in the study population during the 6-month follow-up period. Hence, it was noted in our study that the morbidity in the surgical group was found to be more during the follow-up period. Although this was not statistically significant, the morbidity associated with the surgical procedure is to be considered. Whereas, there were hardly any complications in endoscopic group. A comparative analysis of pseudocyst drainage by Sandulescu et al. revealed an endoscopic method success rate of 77%. According to their investigation, the remaining patients’ failures were caused by the contents, thick pseudocyst walls, and bleeding at the puncture site [7]. In the present study, the success rate in both groups was comparable. It was seen that one patient in endoscopic drainage group had a persistent and haemorrhagic cyst and one patient in open surgical drainage group had a persistent cyst (4-week follow-up showed persistent pseudocyst on CT with mild symptoms) in the follow up period [8-10]. This persistent cyst does not mean technical failure since there was significant reduction in the cyst size as compared to that prior to intervention. Both the patients were followed up without any intervention and resolution of symptoms was seen on following up further. Further, the success rate in the endoscopic group could be attributed to the use of ultrasound guidance for all the procedures. Also, those patients with pseudocysts located in the pancreatic tail were excluded from the study, making the drainage procedures more effective in both groups. There was no mortality during this study period. All the Histo Pathological Examination (HPE) reports of the cyst wall in the study were benign and no malignancy was reported.
Conclusion
In conclusion, although both surgical and endoscopic drainage methods are equally efficient with similar success rate in managing pancreatic pseudocysts, endoscopic drainage should be considered as the first line of management, when available, owing to the lesser overall procedural cost, lesser duration of hospital stay and lesser morbidity in the long run. Additional Information Disclosures Human subjects: Consent was obtained or waived by all participants in this study. Vydehi Institutional had comparable levels of therapeutic success, problems, or reinterventions.
Limitations
The study had a short follow-up period and hence complications developed thereafter are not reported. Also, the prevailing pandemic must have prevented a greater number of patients from following up after the procedure.
References
- Redwan AA, Hamad MA, Omar MA. Pancreatic pseudocyst dilemma: Cumulative multicenter experience in management using endoscopy, laparoscopy, and open surgery. J Laparoendosc Adv Surg Tech A 2017;27(10):1022-1030.
[Crossref] [Google Scholar] [Pubmed]
- Saluja SS, Srivastava S, Govind SH, Dahale A, Sharma BC, Mishra PK, et al. Endoscopic cystogastrostomy versus surgical cystogastrostomy in the management of acute pancreatic pseudocysts. J Minim Access Surg 2020;16(2):126-131.
[Crossref] [Google Scholar] [Pubmed]
- Saul A, Luna MA, Chan C, Uscanga L, Andraca FV, Calleros JH, et al. EUS-guided drainage of pancreatic pseudocysts offers similar success and complications compared to surgical treatment but with a lower cost. Surg Endosc 2016;30:1459-1465.
[Crossref] [Google Scholar] [Pubmed]
- Varadarajulu S, Bang JY, Sutton BS, Trevino JM, Christein JD, Wilcox CM, et al. Equal efficacy of endoscopic and surgical cystogastrostomy for pancreatic pseudocyst drainage in a randomized trial. Gastroenterology 2013;145(3):583-590.
[Crossref] [Google Scholar] [Pubmed]
- Farias GF, Bernardo WM, de Moura DT, Guedes HG, Brunaldi VO, Visconti TA, et al. Endoscopic versus surgical treatment for pancreatic pseudocysts: Systematic review and meta-analysis. Medicine 2019;98(8): e14255.
[Crossref] [Google Scholar] [Pubmed]
- Teoh AY, Dhir V, Jin ZD, Kida M, Seo DW, Ho KY, et al. Systematic review comparing endoscopic, percutaneous and surgical pancreatic pseudocyst drainage. World J Gastrointest Endosc 2016;8(6):310-318.
[Crossref] [Google Scholar] [Pubmed]
- Sandulescu S, Surlin V, Margaritescu D, Georgescu E, Georgescu I. Surgical Drainage versus Endoscopic Drainage in Pancreatic Pseudocyst. Curr Health Sci J 2013;39(3): 164-168.
- Zhao X, Feng T, Ji W. Endoscopic versus surgical treatment for pancreatic pseudocyst. Dig Endosc 2016;28(1):83-91.
[Crossref] [Google Scholar] [Pubmed]
- Melman L, Azar R, Beddow K, Brunt LM, Halpin VJ, Eagon JC, et al. Primary and overall success rates for clinical outcomes after laparoscopic, endoscopic, and open pancreatic cystgastrostomy for pancreatic pseudocysts. Surg Endosc 2009;23:267-271.
[Crossref] [Google Scholar] [Pubmed]
- Varadarajulu S, Lopes TL, Wilcox CM, Drelichman ER, Kilgore ML, Christein JD, et al. EUS versus surgical cyst-gastrostomy for management of pancreatic pseudocysts. Gastrointest Endosc 2008;68(4):649-655.
[Crossref] [Google Scholar] [Pubmed]