Case Report - Archives of Clinical and Experimental Surgery (2022)
Immediate Dental Implants, Clinical, Radiographic, Aesthetic Outcomes, Advantages and Disadvantages
Shaimaa Hussein Rafat Kotb*Shaimaa Hussein Rafat Kotb, Department of Oral Medicine and Periodontology, Alazher University, Assuit, Egypt, Tel: +201062051669, Email: shaymarafat.dental@gmail.com
Received: 26-Aug-2022, Manuscript No. EJMACES-22-72971; Editor assigned: 29-Aug-2022, Pre QC No. EJMACES-22-72971 (PQ); Reviewed: 15-Sep-2022, QC No. EJMACES-22-72971; Revised: 21-Sep-2022, Manuscript No. EJMACES-22-72971 (R); Published: 30-Sep-2022
Abstract
Background: Immediate implantation in fresh extraction sockets is regarded as a treatment modality that appears to give various advantages over the delayed traditional type. Thus, the aim of this case series was to assess the clinical, radiographic, and esthetic outcomes of the immediately placed implants and describe some of the essential clinical factors to consider when selecting patients for implants such as, the thickness of socket walls, thickness of gingival drapes, and optimal position of the implant, and patient factors such as medical conditions, hygiene and smoking cessation, as well as the benefits and drawbacks of this treatment modality.
Objective: To restore the normal function, aesthetics, speech, and health of patients. The ability to achieve these characteristics with the use of immediate dental implants in the rehabilitation of partially and fully edentulous jaws has become a well-established and accepted modern therapeutic modality techniqies.
Methods: Immediate dental implant placement was placed at the freash extraction socket. Radiographic evaluation was performed to assess the amount of marginal bone loss, and patient assessed outcomes were also evaluated at the 6 month follow-up. All implants were successful functionally without any pain or inflammation, with optimal soft tissue health and esthetics, and with minimal radiographic marginal bone loss at the last follow-up visit (3 months after).
Results: There were an excellent clinical, radiographical and aesthetics outcomes in immediately placed implants.
Conclusion: Immediate implants showed excellent results regarding implant success, survival and esthetic outcomes with high patient satisfaction in this study. Evidence available indicates that it is a successful procedure that may benefit patients. However, careful planning and case selection are needed to ensure implant success and final esthetic outcomes.
https://marmarisdentalcenter.com
https://dentalclinicmarmaris.com
https://smilemakeovermarmaris.com
https://marmarisdentals.com
https://marisdentist.com
https://turkeysmilemakeover.com
https://dentalcenterinistanbul.com
https://turkeydentalcenter.co.uk
Keywords
Dental implants; Immediate implants; Delayed implants; Osseointegration; Fresh extraction sockets; Tooth extraction
INTRODUCTION
Dental implants are the most sophisticated method of tooth replacement following tooth extractions; this is the principal indication for dental implants. Immediate implant placement defined as the positioning of a dental implant immediately into a fresh extraction socket after tooth extraction, has been considered a predictable and acceptable procedure for restoring missing teeth. Immediate placement at the moment of extraction has become increasingly prevalent in recent years and may provide practitioners and patients with distinct benefits. It provides for a reduction in treatment time, which may boost patient satisfaction, decrease morbidity, and allow for the prosthetics right placement of implants. It also aids in preserving the alveolar bone’s height and preventing the marginal bone loss that usually occures during socket healing following extraction. Immediate implant placement in extraction sockets is a relatively new and extremely successful method of therapy. Its advantages include less bone resorption and a shorter treatment period compared to implantation in healed sockets [1,2].
Ideal implant parameters would include the appropriate bone quality (D2 or D3 bone), screw-shaped implants, a rough implant surface, a minimum implant length of 10 mm, suffient primary stability, and the avoidance of lateral stresses. Immediate dental implants appear to be mostly dependent on the primary stability of the immediately implanted prosthesis [3].
Conventional implant placement was considered a delayed dental implant that included tooth extraction, 2–4 months following the extraction socket to heal, insertion of the implant, and 3–6 months for the implant to integrate with the surrounding bone; a second operation was necessary to expose the implant and put the prosthetic abutment. The patient had to wait between eight and twelve months, inclusive of the prosthetic therapy, for the replacement of a missing tooth [4].
Immediate dental implantation necessitates the use of atraumatic extraction procedures, which are necessary for maintaining the maximum amount of bone surrounding the implant. Additionally, it preserves the integrity of the buccal bone plate, without which it would be contraindicated to insert implants rapidly. Therefore immediate implants remain a technique-sensitive surgery [5].
Periotome-assisted extraction with little mucoperiosteal flap elevation by surrounding the removed tooth with a periotome, the periodontal ligaments are ruptured and torn. Using the proper forceps and a gentle twisting motion, care should be taken to preserve the face and palatal walls of the socket. To eliminate any vestiges of connective tissue tags or periodontal ligaments, the socket is vigorously degranulated and irrigated with a saline solution using a tiny curette. Preoperative X- rays, including periapical X-rays, Cone-Beam Computed Tomography (CBCT), and panoramic radiographs, are required to detect implant size and bone irregularities. Using a rachet, the implant is manually tightened to 45 N of tension. The implant was positioned at the crestal bone level. With a cover screw, the implant was covered. In between the implant and the socket wall, an autoplastic bone graft is placed. The graft particles were densely packed in space. Instead of covering the bone transplant with a membrane, the implant was closed with natural soft tissue. The implant sites were clinically and radiographically assessed one week and six months following surgery [6].
Radiographic evaluation of the crestal bone height using the long-cone parallelling method, radiographs (Kodak Ultra Speed; Eastman Kodak Co., Rochester, NY, USA) were acquired at the time of prosthesis implantation and six months later perpendicular to the implant axis. The radiographs were digitized, and the level of the crestal bone was analysed to determine the level of the marginal bone. OPG images were used to examine the implant’s surrounding radiolucency [7].
Immediate implant placement seeks to achieve osseointegration by encouraging the formation of new bone at the extraction site. The majority of early dental implants achieved osseointegration. Immediate implant techniques reduce the number of clinical procedures and enhance the patient environment. The ability to previsualize dental implants immediately or shortly after surgery enables the patient to recover normal masticatory function as quickly as feasible. The osteointegration (biological stability) of an implant is subsequent to bone regeneration and remodelling. The insertion of bone substitutes between the titanium implant surface and the inside walls of the sockets would enhance the initial stability of immediately inserted implants, followed by biological fixing and the osseointegration process [8].
To minimize osteonecrosis and the subsequent growth of fibrous tissue surrounding the implants, immediate dental implants are designed to lessen surgical trauma during a one-step surgical procedure. According to Misch, et al., the reduction of surgical trauma in immediate implant procedures can be achieved by minimizing heat production during surgical stages and strain at the bone/implant contact. Therefore, the rationale for immediate dental implants is not only to decrease the risk of fibrous tissue formation but also to reduce the growth of immature bone and to speed the maturation of immature bone into lamellar bone [9,10].
Implant primary stability is an important determinant of the efficacy of immediate implants. Several variables, including implant geometry and length, surface morphology, splinting of implants, management of occlusal stress, bone quality, and absence of unfavorable patient behaviors, have been shown to influence implant stability. Implant stability consists of two stages: primary stability, which is mostly derived from mechanical contact with cortical bone, and secondary stability, which offers biological stability via bone regeneration and re-modelling (osseointegration) [11].
Following several months of healing, osseointegrated dental implants with bone deposition are now close to the implant surface. Implants with immediate placement have excellent osseointegration success rates. Bone deposition occurs in phases, beginning with the creation of woven bone, particularly in the spaces between implant threads. This eventually evolves into lamellar bone. The surface features, surface material, and loading factors can affect the adaptation of developing bone to the implant surface [12].
The functional surface area is more critical to the design of an implant than its size. Cylindrical implants with a wider diameter and no threads have a lower surface area than screws with a smaller diameter. Therefore, implants with threads should be ideal for quick loading processes. Implants for quick loading operations must be threaded, have surface treatment (rough surface), and be at least 10 mm in length, according to Uribe, et al. [13].
Instantaneous implant procedures require primary implant stabilization between 35 and 60 N/cm during surgery. According to Uribe, et al., osseointegration may be expected when primary stability and torque equal to or greater than 35 N/cm are achieved. Major stability is affected by surgical procedures, implant design, bone density, and quantity. After early stabilization, the bone starts its mending through bone plasticity, reabsorption, and apposition in response to a local stimulus. Lamellar and immature bones are more prevalent near dental implants. The lamellar bone has the highest resistivity and modulus of elasticity, making it the most effective bone for supporting stresses. In contrast, juvenile bone is disorganized, brittle, and pliable, leaving it incapable of supporting weight. In delayed loading operations, the majority of immature bone tissues are replaced by lamellar bone three to six months following surgical implant insertion. Therefore, one of the indications for rapid loading implants would not only be to lower the danger of creating fibrous tissues but also to limit the formation of immature bone and encourage a quicker maturation of juvenile bone into lamellar bone [14].
The primary cause of acute dental implant failure is dysfunctional behaviors. Despite the fact that parafunctional loads increase the risk of fracture or loosening of abutments and interim restorations, occlusal adjustment seems to favor the results of rapid loading implants. Inappropriate quality or quantity of peri-implant hard and soft tissue, the patient’s medical state, unfavorable behaviors, inadequate surgical and prosthetic therapy, implant design, implant localization and location, and inadequate plaque management may all contribute to implant loss or failure [14,15].
The significance of the long-term prognosis and the efficacy of the implants is the preservation of peri-implant bone levels since medically-induced stress may result in marginal bone loss. In addition, the prognosis and success are affected by the appropriate creation of the biological width and frequent removal and reattachment of prosthetic components [16].
Albrektsson states that crestal bone loss of 0.1 to 0.2 mm per year following insertion is common and effective. There are still obstacles for the oral surgeon in evaluating the appropriate implant position at the bone level, which increases the risk of implant exposure. Subcrestal implant placement reduces this danger and permits bone stabilization or development over the shoulder of the implant. As the apical section of the alveolar ridge is often broader than the coronal portion, subcrestal implant placement can reduce the requirement for augmentation therapy [17].
Immediate implants have several advantages, including fewer surgical interventions, a reduction in overall treatment time, a decrease in soft and hard tissue loss, patient satisfaction, and less invasive surgery. Consequently, immediate implant placement in the extracted socket is a widely a cognledged and practiced technique that delivers outstanding success rates and the most patient happiness, which is our major objective. In many instances, immediate implants are considered a feasible alternative to standard delayed implants [18].
Disadvantages of immediate implant placement include lack of control over the final implant position; difficulty achieving primary stability; inadequate soft tissue coverage; inability to inspect all aspects of the extraction site for defects or infection; difficulty in preparing the osteotomy due to bur movement along the extraction site walls; and the additional cost of bone grafting. Immediate dental treatment necessitates additional chairside time at the time of implant placement compared to conventional implant therapy [19].
The decision to extract teeth and replace them with immediate implants is determined by many factors. Advanced periodontal attachment loss, teeth restored with crowns, loosened endodontic posts, and advanced caries, unfavorable crown-to-root ratios. The goal of this article is to review some of the important clinical considerations when selecting patients for immediate implant placement, and to discuss the advantages and disadvantages of this mode of therapy.
Methodology
Patient evaluation
The first step in determining whether immediate implant placement is a reasonable clinical choice is the evaluation of the potential implant site. Residual extraction socket morphology may complicate ideal implant positioning in fresh extraction sockets. The slope of the axial walls, the root curvature of the extracted tooth, and the final position of the apex of the extracted tooth in the alveolar housing pose challenges to the precise, atraumatic placement of an implant in the most desirable restorative position.
The inclusion criteria: The ideal extraction site for immediate implant placement was one with little or no periodontal bone loss on the tooth that was to be extracted, such as a tooth being extracted due to endodontic involvement, root fracture, root resorption, periapical pathology, root perforation, or unfavorable crown-to-root ratio. Most researchers recommend at least 3 to 5 mm of bone beyond the apex and a bony length of 10 mm or greater for stability when placing immediate implants. Therefore, immediate implant placement should be limited to those defects that have three or four walled sockets, sufficient bone to stabilize the implant, and minimal circumferential defects. Initial implant stability is the most critical factor in implant osseointegration. Thus, an ideal site is one that has significant alveolar bone around the socket enabling the implant to fill the socket space.
The exclusion criteria: compromised general health, which may have an effect on the healing and osseointegration of dental implants, parafunctions (bruxism, clenching, heavy smokers (>10 cigarettes per day); malignant disease; chemotherapy, bisphosphonate therapy, irradiation therapy; immunocompromising diseases, e.g. HIV and poor oral hygiene (PSI ≥ 3).
The requirements for immediate implant placement were according to the third ITI Consensus Conference are:
(1) Minimal-invasive tooth extraction, with retention of the vestibular bone lamella.
(2) Removal of all granulation tissue.
(3) Sufficient primary stability (30–40 Ncm).
(4) Three-dimensionally correct position considering the later restoration by means of the provisional tool based on the previous tooth position.
(5) No local contraindications such as parafunctions.
Case study
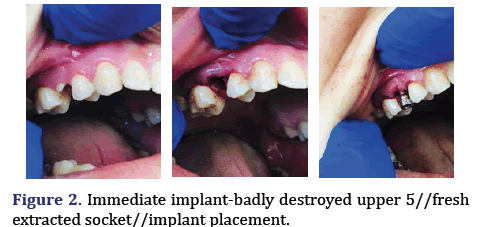
A 31-year-old-female medically fit patient presented in September 2019 with a deep subgingival caries and failed endodontic treatment of the maxillary left second premolar. The patient requested a definitive restoration of this tooth. After discussing with the patient different treatment options such as endodontic retreatment and orthodontic forced eruption or crown lengthening to allow the tooth to be crowned with sufficient ferrule, or single tooth implant crown, the patient selected the immediate implant option since the cross sectional CBCT showed sufficient native bone to achieve good primary stability for immediate implant placement.
Clinical procedure
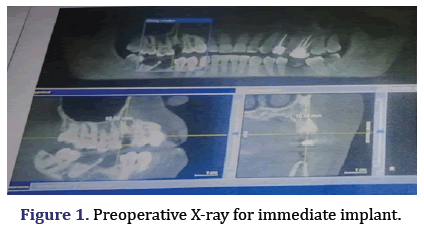
Tooth extraction the first step in immediate implant placement after case selection was atraumatic extraction. Every attempt should be made to minimize trauma to the alveolus during the the palatal aspect of the alveolus to prevent perforation of the buccal plate. Once the osteotomy was prepared to the desired depth with at least 3 to 5 mm of intimate implant-to-bone contact, an implant was placed. The implant must be stable within the osteotomy with no mobility. Kohal, et al. have shown that the pressure of the implant on the bony walls of the alveolus can result in microfractures and early crestal bone loss. The ideal situation would be for the implant to be in contact with the socket without putting undue pressure on the socket walls unless the alveolus was very thick, leaving no gap between the head or neck of the implant and surrounding socketwalls. In other words, the radiographic appearance of an ideal immediate implant placement would look the same as a standard implant placement. The implant-to-socket wall space: promotes greater osseointegration. When a gap exists between the socket wall and the implant fixture, a bone graft and/or membrane can be used to prevent epithelial migration into the space and aid in healing. Preoperative X-ray for Immediate Implant is shown in Figure 1.
Soft tissue management
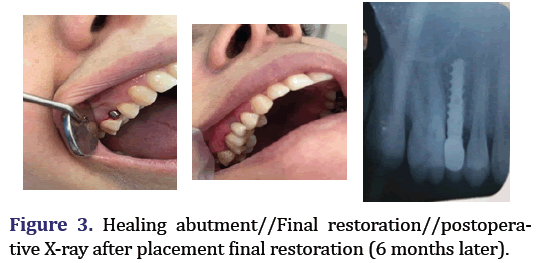
One of the most critical factors in implant restorative esthetics is the gingival form. The gingival tissues can be shaped and managed by the provisional prosthesis and by the provisional crown placed on the implant prior to placement of the definitive crown. The use of anatomic gingival formers or single stage implants and the placement of implants without elevating a flap have significantly improved the clinician’s ability to achieve an excellent peri-implant gingival form (Figures 2 and 3).
Results
Clinical evaluation
All the patients showed no signs or symptoms of pain, tenderness, redness or inflammation of soft tissue around the inserted implant site throughout the study. Normal healing process of the soft tissue and bone around the implant are observed throughout the study. All patients continued the follow up period without any signs of infection, gingivitis or peri-implantitis.
Discussion
The aim of this study was to investigate the clinical, radiographic outcome and patient satisfaction of immediately placed implants. No significant differences were found in marginal bone level loss with respect to implant placement time. Cavallaro, et al. [19] concluded that when the treatment is planned for extraction and potential immediate implant therapy the, teeth should be extracted in the most a traumatic manner possible. There are still challenges for the oral surgeon to determine the appropriate bone substitute around the inserted immediate implant to achieve a successful osseointegration and increase the success rate of dental implants.
Advantages and Disadvantages
Advantages of placing immediate implants are the reduction in time of therapy, reduction in surgical episodes, and preservation of the bone and gingival tissues. Agreater rate of bone resorption occurs during the first 6 months following tooth extraction, unless an implant is placed or a socket augmentation procedure was performed. The biological advantages of immediate implant placement are also psychological advantages. Although many patients readily accept delayed implant placement, some find it difficult to face the prospect of waiting up to 6 months for an extraction site to heal followed by an additional 3 to 6 months for the implant to osseointegrate. Disadvantages of immediate implant placement include,: (i) lack of control of the final implant position; (ii) difficulty obtaining primary stability; (iii) inadequate soft tissue coverage; (iv) inability to inspect all aspects of the extraction site for defects or infection; (v) difficulty in preparing the osteotomy due to bur movement (chatter) on the walls of the extraction site; and (vi) the added cost of bone grafting.
Summary
Challenge era to the clinician for ideal implant positions, such as unfavorable extraction socket morphology, inadequate soft tissue for implant coverage, and bone defects. Dental implants that are placed immediately into the selected extraction sockets have high survival rates comparable to delayed implants that are placed in the healed sites. Immediate implants provide significant advantages, including fewer surgical procedures, shorter treatment times, and improved aesthetics. The key to implant success is to achieve primary stability.
Conclusion
Immediate dental implants show excellent outcomes with regards to clinical, radiographic and aesthetics outcomes of implant survival and minimal changes in peri-implant soft and hard tissue dimensions. Case selection is critical, before any surgical approach, and detailed systemic medical conditions and habit history should be obtained. Patient compliance and expectations should be determined. Evidence available indicates that it is an effective procedure that might help patients. To guarantee implant success and desired aesthetic results, however, meticulous planning and case selection are required.
Conflict of Interest
No conflict of interest.
Funding
Self-funding.
References
- Quirynen M, van Assche N, Botticelli D, Berglundh T. How does the timing of implant placement to extraction affect outcome? Int J Oral Maxillofac Implants 2007; 22:203-23.
[Google Scholar] [Pubmed]
- Botticelli D, Renzi A, Lindhe J, Berglundh T. Implants in fresh extraction sockets: a prospective 5‐year follow‐up clinical study. Clin Oral Implants 2008;19(12):1226-32.
- Vidyadharan A, Hanawa Y, Godfrey S, Resmi PG. Immediate implants and immediate loading in full arch maxilla and mandible of a bruxer–A case report. IOSR J Dent Med Sci. 2014;13:62-7.
- Schropp L, Isidor F. Timing of implant placement relative to tooth extraction. J Oral Rehabil 2008;35:33-43.
- Wagenberg B, Froum SJ. A Retrospective Study of 1,925 Consecutively Placed Immediate Implants From 1988 to 2004. Int J Oral Maxillofac Implants 2006;21(1):71-80.
[Google Scholar] [Pubmed]
- Becker W, Goldstein M. Immediate implant placement: Treatment planning and surgical steps for successful outcome. Periodontology 2008;47(1):79-89.
[Crossref] [Google Scholar] [Pubmed]
- Misch CE, Wang HL, Misch CM, Sharawy M, Lemons J, Judy KW, et al. Rationale for the application of immediate load in implant dentistry: part II. Implant Dent 2004;13(4):310-21.
- Terro W, Terro M. The effect of smoking and nonsmoking on bone healing (Osseo integrated phase) around locking-taper dental implants. J Dent Impl 2015;5(1):12-5.
- Misch CE, Wang HL, Misch CM, Sharawy M, Lemons J, Judy KW. Rationale for the application of immediate load in implant dentistry: Part I. Implant dent 2004;13(3):207-17.
- Duyck J, Naert I, Rønold HJ, Ellingsen JE, van Oosterwyck H, Vander Sloten J, et al. The influence of static and dynamic loading on marginal bone reactions around osseointegrated implants: An animal experimental study. Clin Oral Implants Res 2001;12(3):207-18.
[Crossref] [Google Scholar] [Pubmed]
- Atsumi M, Park SH, Wang HL. Methods used to assess implant stability: current status. Int J Oral Maxillofac Implants 2007;22(5): 743–54.
[Google Scholar] [Pubmed]
- Nkenke E, Fenner M, Vairaktaris EG, Neukam FW, Radespiel-Tröger M. Immediate versus delayed loading of dental implants in the maxillae of minipigs. Part II: Histomorphometric analysis. Int J Oral Maxillofac Implants 2005;20(4): 540-6.
[Google Scholar] [Pubmed]
- Uribe R, Penarrocha M, Balaguer J, Fulgueiras N. Immediate loading in oral implants. Present situation. Med Oral Patol Oral Cir Bucal 2005;10:143-53.
[Google Scholar] [Pubmed]
- Ganeles J, Wismeijer D. Early and immediately restored and loaded dental implants for single-tooth and partial-arch applications. Int J Oral Maxillofac Implants 2004;19(7): 92–102.
[Google Scholar] [Pubmed]
- Schnitman PA, Wöhrle PS, Rubenstein JE, DaSilva JD, Wang NH. Ten-year results for Brånemark implants immediately loaded with fixed prostheses at implant placement. Int J Oral Maxillofac Implants 1997;12(4): 495-503.
[Google Scholar] [Pubmed]
- Kourtis SG, Sotiriadou S, Voliotis S, Challas A. Private practice results of dental implants. Part I: Survival and evaluation of risk factors—Part II: Surgical and prosthetic complications. Implant Dent 2004;13(4):373-85.
[Crossref] [Google Scholar] [Pubmed]
- Tolstunov L. Dental implant success-failure analysis: A concept of implant vulnerability. Implant Dent 2006 ;15(4):341-6.
[Crossref] [Google Scholar] [Pubmed]
- Grunder U. Immediate functional loading of immediate implants in edentulous arches: two-year results. Int J Periodontics Restorative Dent 2001;21: 545-51.
[Google Scholar] [Pubmed]
- Cavallaro JS, Greenstein G, Tarnow DP. Clinical pearls for surgical implant dentistry: Part 3. Dent Today 2010;29(10):134-6.
[Google Scholar] [Pubmed]
Copyright: © 2022 The Authors. This is an open access article under the terms of the Creative Commons Attribution NonCommercial ShareAlike 4.0 (https://creativecommons.org/licenses/by-nc-sa/4.0/). This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.