Research Article - Archives of Clinical and Experimental Surgery (2023)
Impact of Covid-19 Pandemic on Breast Cancer Patients in a Tertiary Care Center
Jujar Kapadia*, Shashi Shankar Sharma, Sanjay Kumar Mahajan, Rahul Tayal, Swati Simran, Sonia Moses, Sachin Verma, Sahaj Dhakad, Gaurav Garg and Gautam BirlaJujar Kapadia, Department of General Surgery, Madhya Pradesh Medical Science University, Madhya Pradesh, India, Tel: +919039377752, Email: jujar.kapadia123@gmail.com
Received: 01-May-2023, Manuscript No. EJMACES-23-97494; Editor assigned: 03-May-2023, Pre QC No. EJMACES-23-97494 (PQ); Reviewed: 18-May-2023, QC No. EJMACES-23-97494; Revised: 25-May-2023, Manuscript No. EJMACES-23-97494 (R); Published: 01-Jun-2023
Abstract
Background: The COVID-19 pandemic has significantly impacted the health-care system worldwide, and surgeons faced challenges in clinical practice, especially in managing cancer patients. This study aimed to assess the impact of COVID-19 on delay of breast cancer patient’s management.
Methods: A cross-sectional study was conducted to study the impact of global COVID-19 pandemic and subsequent governmental directives on surgery department of M.G.M. Medical College, M.Y. Hospital, Indore (M.P.) on all breast cancer patients referred to our unit from march 2021 to July 2021. Type of treatments and surgery, TNM, tumor diameter, and predictive and prognostic factors were analysed.
Conclusions: The study’s findings show that the active COVID-19 pandemic led to a more stressful situation among physicians, which has affected management of breast cancer patients. COVID-19 is reshaping the delivery of not only breast cancer care but also general oncology practice. Currently, due to the availability of effective vaccination and more understanding of COVID-19, we believe that breast cancer operations should be performed on their scheduled date.
Keywords
Breast cancer; COVID-19; Surgery
Introduction
At the end of December 2019, an outbreak of an interstitial lung disease caused by a novel type of coronavirus (SARS-CoV-2) was first reported in the city of Wuhan, China [1]. The World Health Organization (WHO) subsequently designated it as the Coronavirus Disease 2019 (COVID-19) [2,3]. One month later, the COVID-19 outbreak was declared a pandemic [4]. The rapid global spread of the viral infections and disease led to the introduction of far-reaching containment and reduction strategies in the affected countries around the world. To provide hospital capacity, protective equipment and ventilators for an expected increasing number of COVID-19 patients, surgical disciplines in India were instructed to postpone all elective surgeries and to reallocate staff to the intensive care units and COVID-19 wards as needed [5]. Various national surgical societies and associations published statements on the guidance for triage and urgent surgical interventions that were still considered feasible or mandatory [6,7,8]. Many surgical units were massively affected by restructuring measures [9,10]. 45% of patients with early breast cancer; depending on age and tumor biology) may be recommended to receive neoadjuvant chemotherapy or adjuvant chemotherapy and the benefits are related to maintaining dose and schedule [11-16]. Neoadjuvant chemotherapy is generally recommended for the treatment of high-risk early breast cancer [17], and this approach continues to be appropriate during the pandemic [18]. Delay or interruption of neoadjuvant chemotherapy or adjuvant chemotherapy by COVID-19 infection could result in adverse outcomes including development of drug resistance and cancer progression. This Perspective addresses the impact of the pandemic on neoadjuvant chemotherapy and routine care [19-21].
The present cross-sectional study aims to evaluate the impact of the global COVID-19 pandemic and subsequent governmental directives on surgical departments. In the survey conducted, data were collected on experiences regarding the effect of the governmental restrictions, on restructuring and financial burdens for the surgical departments, as well as on the assessment of future developments. The results may be helpful for other countries in adapting containment strategies or resuming elective surgeries in order to regain high quality surgical care under the given circumstances, especially since further waves of the pandemic are expected.
Methods
Study design
A cross sectional study was conducted to study the impact of global COVID-19 pandemic and subsequent governmental directives on surgery department of M.G.M. Medical College, M.Y. Hospital, Indore (M.P.) on all breast cancer patients referred to our unit from March 2021 to July 2021 were enrolled. Type of treatments and surgery, TNM, tumor diameter, and predictive and prognostic factors were analyzed.
Duration of study- 5 months
Sample size: All the patient whose surgeries were delayed due to COVID 19 pandemic and who underwent chemo therapy for breast carcinoma was selected.
Inclusion criteria
1. All cases of breast cancer whose diagnosis was confirmed by histopathological examination.
2. All the patients who gave written consent.
Methodology
Women older than 18 years and diagnosed with breast cancer during study period were selected for inclusion. After breast cancer diagnosis, the following data are gathered: patient characteristics (e.g., age at diagnosis, gender, socio-economic status), detection method (e.g., screening), tumor characteristics (e.g., TNM stage, morphology, grade, and hormone receptor status), and primary treatment (e.g., surgery, neoadjuvant therapy, and systemic therapy).
Results
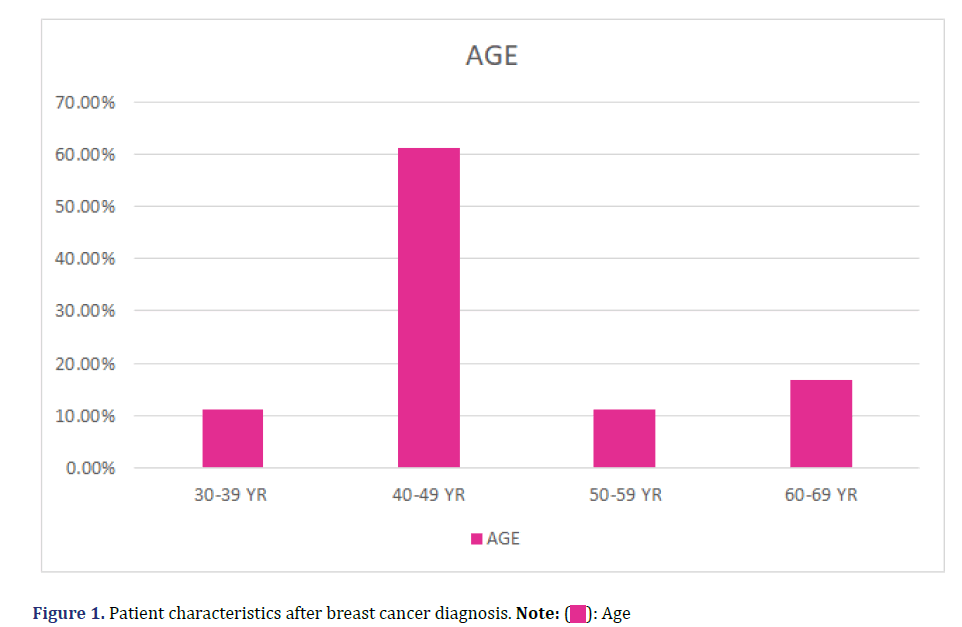
Twenty patients were diagnosed with carcinoma of breast from March 2021 to July 2021. All patients were female, ranging from 30 to 63 years of age (mean 47.3 ± 5.45) (Figure 1). On histo-pathological examination 17 (85%) patients had invasive carcinoma, while remaining had medullary carcinoma of breast (1), neuroendocrine tumor (1) and ductal carcinoma in situ (1) (Figure 2). Those who presented with a benign lump were excluded from the study. No participant withdrew from the study at any time after giving consent. Majority of them i.e., 9 (45%) had grade 3 tumor, 5 had grade 2 tumor (Figure 3). All of them underwent chemotherapy.
Discussion
The COVID-19 pandemic which started in December 2019, is not over yet and at present it cannot be predicted when this is going to end as it depends on multiple factors like infectivity of a person, the isolation measures and lockdown status of affected countries, and emerging immunity. The vaccination campaign is having an impact, albeit slowly, it will take ages for the country to achieve herd immunity.
With the reallocation of the maximum resources by the hospital to the COVID-19 patient care in critical units, resource demanding diseases like breast cancer services have faced serious setbacks. We have tried to quantify what setbacks breast cancer care has taken in our hospital due to this pandemic. We have seen in our study that these patients present extremely late to the hospital due to a myriad of known and unknown reason. On top of that sometimes they are just lost to follow up for indefinite periods even after the treatment has started. Although we tried to continue with the same treatment protocol for COVID negative and positive patients the patients with positive PCR had to be quarantined as per hospital policy in vogue, which may have contributed to upstaging of disease in some of these patients.
We determined in our study that most of the patients 60 (87%) presented with advanced (stage 2b and above) of breast cancer. This is comparable to another research in where 69.9% females reported in stage III and IV of Breast Cancer [11]. This presentation in advanced stage can be due to longer patient delays from noticing of first symptom to presenting to a health care facility as explained in a meta-analysis by Richard et al. in which a positive relation was seen between patient delay and advanced stage of breast cancer at presentation [11,12]. Though our study does not focus on determining the incidence of COVID-19 among Breast Cancer patients, only a small number of breast cancer patients (17.4%) tested positive which indicates that the suggestion, that breast cancer patients are not at higher risk of COVID-19 than the general population by Vuagnat et al., may have notable footing [22]. Moreover, we found out that the COVID status itself doesn’t have the significant impact on delay in presentation, definitive treatment or surgery. Though, for those testing positive, we followed the quarantine protocol of 14 days isolation with one PCR negative report after completing quarantine.
The limitations of this work include a small number of patients from a single center. So, our results may not be generalizable. For this a multi-centric study with a large sample size is needed, to study the overall outcome of COVID-19 on breast cancer patients and disease progression among them. We also did not include histopathological correlation and response of different types of breast cancer to chemotherapy with disease upstaging and covid status. More research work is needed to find relation of disease upstaging with COVID status.
Conclusion
We found that COVID-19 pandemic had no significant impact on delay in presentation, breast cancer management/ treatment and disease upstaging as compared to figures available for our population before the pandemic. However, our study showed significant correlation between disease upstaging and COVID positive status of patients. These findings made us think to reconsider our protocols of breast cancer care management among COVID positive patients in this pandemic. Our results might help researchers in formulating new breast cancer management guidelines for patients in current or any anticipated future pandemic.
Conflict of Interest
Authors have no conflict of interest.
Funding Agency
None to declare.
References
- Cancer referrals fell from 40,000 to 10,000 per week in April. In NHS Providers 2020.
- Kutikov A, Weinberg DS, Edelman MJ, Horwitz EM, Uzzo RG, Fisher RI, et al. A war on two fronts: Cancer care in the time of COVID-19. Ann Intern Med 2020;172(11):756-758.
[Crossref] [Google Scholar] [Pubmed]
- Updated Intercollegiate General Surgery Guidance on COVID-19. Royal College of Surgeons England, 2020.
- Endoscopy activity and COVID-19: British Society of Gastroenterology and Joint Advisory Group guidance, 2020.
- National Cancer Registration and Analysis Service (NCRAS). Public Health England, 2018.
- Cancer Treatment Information by Cancer Type. National Cancer Institute, 2020.
- ICNARC report on COVID-19 in critical care (24/4/20). Intensive Care National Audit and Research Centre, 2020.
- Docherty AB, Harrison EM, Green CA, Hardwick HE, Pius R, Norman L, et al. Features of 20 133 UK patients in hospital with covid-19 using the ISARIC WHO Clinical Characterisation Protocol: Prospective observational cohort study. BMJ 2020;369:m1985.
[Crossref] [Google Scholar] [Pubmed]
- The Epidemiological Characteristics of an Outbreak of 2019 Novel Coronavirus Diseases (COVID-19), China CCDC, 2020.
- Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19), World Health Organisation, 2020.
- Lee YH, Kung PT, Wang YH, Kuo WY, Kao SL, Tsai WC, et al . Effect of length of time from diagnosis to treatment on colorectal cancer survival: a population-based study. PloS one 2019;14(1):e0210465.
[Crossref] [Google Scholar] [Pubmed]
- Richards MA, Westcombe AM, Love SB, Littlejohns P, Ramirez AJ. Influence of delay on survival in patients with breast cancer: A systematic review. The Lancet 1999;353(9159):1119-1126.
[Crossref] [Google Scholar] [Pubmed]
- Mano R, Vertosick EA, Hakimi AA, Sternberg IA, Sjoberg DD, Bernstein M, et al. The effect of delaying nephrectomy on oncologic outcomes in patients with renal tumors greater than 4 cm. Urol Oncol 2016;34(5):239.e1-8.
[Crossref] [Google Scholar] [Pubmed]
- Smith EC, Ziogas A, Anton-Culver H. Delay in surgical treatment and survival after breast cancer diagnosis in young women by race/ethnicity. JAMA surg 2013;148(6):516-523.
[Crossref] [Google Scholar] [Pubmed]
- Chu AT, Holt SK, Wright JL, Ramos JD, Grivas P, Yu EY, et al. Delays in radical cystectomy for muscle-invasive bladder cancer. Cancer 2019;125(12):2011-2017.
[Crossref] [Google Scholar] [Pubmed]
- Sanchez-Ortiz RF, Huang WC, Mick R, Van Arsdalen KN, Wein AJ, Malkowicz SB, et al. An interval longer than 12 weeks between the diagnosis of muscle invasion and cystectomy is associated with worse outcome in bladder carcinoma. Journal Urol. 2003;169(1):110-115.
[Crossref] [Google Scholar] [Pubmed]
- May M, Nitzke T, Helke C, Vogler H, Hoschke B. Significance of the time period between diagnosis of muscle invasion and radical cystectomy with regard to the prognosis of transitional cell carcinoma of the urothelium in the bladder. Scand J Urol Nephrol 2004;38(3):231-235.
[Crossref] [Google Scholar] [Pubmed]
- Bleicher RJ, Ruth K, Sigurdson ER, Beck JR, Ross E, Wong YN, et al. Time to surgery and breast cancer survival in the United States. JAMA Oncol 2016;2(3):330-339.
[Crossref] [Google Scholar] [Pubmed]
- Samson P, Patel A, Garrett T, Crabtree T, Kreisel D, Krupnick AS, et al. Effects of delayed surgical resection on short-term and long-term outcomes in clinical stage I non-small cell lung cancer. Ann Thorac Surg 2015;99(6):19006-19013.
[Crossref] [Google Scholar] [Pubmed]
- Yang CF, Wang H, Kumar A, Wang X, Hartwig MG, D'Amico TA, et al. Impact of timing of lobectomy on survival for clinical stage IA lung squamous cell carcinoma. Chest 2017;152(6):1239-1250.
[Crossref] [Google Scholar] [Pubmed]
- Richards MA, Smith P, Ramirez AJ, Fentiman IS, Rubens RD. The influence on survival of delay in the presentation and treatment of symptomatic breast cancer. Br J Cancer 1999;79(5):858-864.
[Crossref] [Google Scholar] [Pubmed]
- Elliss-Brookes L, McPhail S, Ives A, Greenslade M, Shelton J, Hiom S, et al. Routes to diagnosis for cancer–determining the patient journey using multiple routine data sets. Br J Cancer 2012;107(8):1220-1206.
[Crossref] [Google Scholar] [Pubmed]
Copyright: © 2023 The Authors. This is an open access article under the terms of the Creative Commons Attribution Non Commercial Share Alike 4.0 (https://creativecommons.org/licenses/by-nc-sa/4.0/). This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.








 ): Age
): Age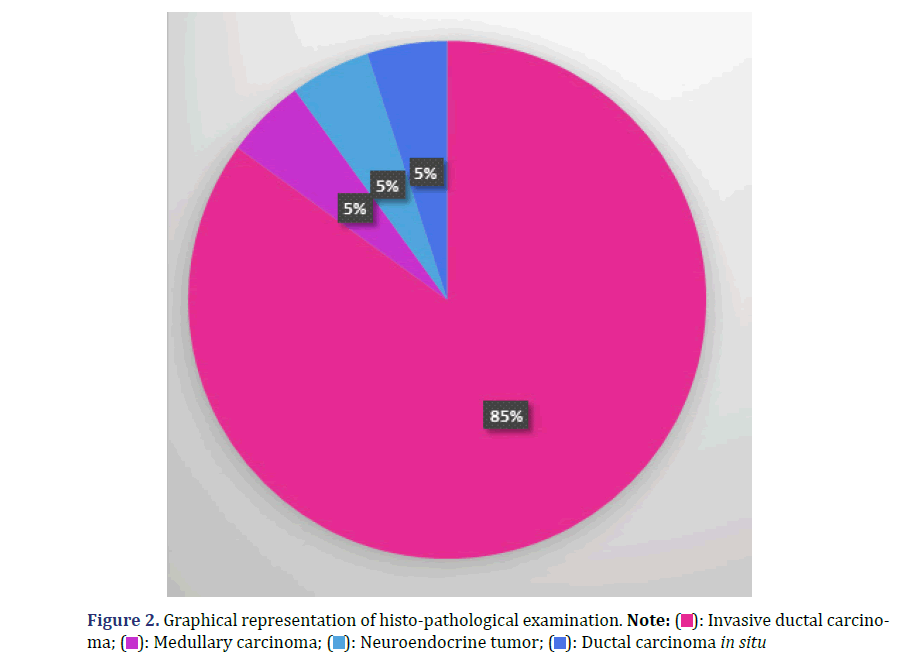
 ): Invasive ductal carcinoma;
(
): Invasive ductal carcinoma;
( ): Medullary carcinoma; (
): Medullary carcinoma; ( ): Neuroendocrine tumor; (
): Neuroendocrine tumor; ( ): Ductal carcinoma in situ
): Ductal carcinoma in situ
 ): Grade 1; (
): Grade 1; ( ): Grade 2; (
): Grade 2; ( ): Grade 3;
(
): Grade 3;
( ): Grade 4.
): Grade 4.