Research Article - Archives of Clinical and Experimental Surgery (2023)
Inverted Internal Limiting Membrane Flap vs. ILM Peeling for <400 µm Macular Hole: A Meta-Analysis and Systematic Review
Pingping Li1*, Lu Li1 and Jianhua Wu22Department of Wuhan Aier Eye Hospital, Wuhan University, Wuhan, China
Pingping Li, Department of Eye Center, Renmin Hospital of Wuhan University, Wuhan, China, Tel: +8615294216239, Email: li_pingping2022@163.com
Received: 15-Feb-2023, Manuscript No. EJMACES-23-89444; Editor assigned: 17-Feb-2023, Pre QC No. EJMACES-23-89444 (PQ); Reviewed: 06-Mar-2023, QC No. EJMACES-23-89444; Revised: 13-Mar-2023, Manuscript No. EJMACES-23-89444 (R); Published: 21-Mar-2023
Abstract
Inverted Internal Limiting Membrane (ILM) flap technique was developed to achieve Macular Hole (MH) closure in large MH. But the efficacy of small holes has been controversial. The aim of this study was to compare the anatomical and visual outcomes of vitrectomy (PPV) combined with the inverted ILM flap and ILM peeling in small and medium size MHs. Search relevant literature within PubMed, Web of Science, Embase, Cochrane library, and CNKI from inception through October 2022 in English or Chinese. Only case-control studies were included. Heterogeneity, publication bias, and sensitivity analysis were conducted to ensure the statistical power. This meta-analysis included six studies involving 299 eyes, 3 randomized control trials, and 3 retrospective studies. Summarizing data displayed that the MH closure rate was not different between the inverted ILM flap group and peeling group (Odds Ratio (OR) =0.29?95% Confidence Interval (CI): 0.04 ~ 1.96, P=0.33). Whereas there was no significant difference in visual acuity improvement, the integrity of the External Limiting Membrane (ELM) and the Ellipsoid Zone (EZ) in 3 months or 12 months after surgery between the two groups. Therefore inverted ILM flap and ILM peeling are both effective treatments for <400 μm MHs, and are associated with comparable outcomes as well as don’t damage the integrity of the retina.
Keywords
Macular hole; Eye; Retina; Surgery
Introduction
Macular Hole (MH) refers to the tissue defect from the inner limiting membrane of the retina to the photoreceptor layer in the macula area. Meanwhile, many patients feel severe visual decline, visual deformation, central scotoma, and other visual impairment. In 1988, Gass [1] suggested that the hole was the tensile force of a tangent line to the surface of the retina. To accelerate the holes close, the traction in the macular area needs to be relieved. Since Kelly, et al. [2] first reported the treatment of MH with ILM peeling in 1991, the rate of MH closure has been greatly improved. Therefore, PPV combined with ILM peeling, gas-liquid exchange during the surgery, and filled vitrectomy became the standard operation for MH [3-6].
The International Vitreomacular Traction Study Group categorized MH according to the size of the minimal diameter of the MH as follows: Small (≤ 250 μm), medium (251–400 μm), and large (>400 μm) [7]. Michalewska, et al. [8] introduced the ILM flap technique to treat large Full-Thickness Macular Holes (FTMH), which refined the standard ILM peeling, and the rate of hole closure arrived at 76%, only 52% in traditional ILM peeling. Mahalingam, et al. [9] also reported that patients of large MH gain better visual acuity in the end by the ILM flap technique. This technique was beneficial for anatomic and functional outcomes for large, traumatic, myopic, and chronic FTMH, since then, more and more surgeons are willing to choose this way. However, it has long been debated whether the ILM flap is effective for small and medium size macular holes. Some studies thought traditional ILM peeling had achieved a very high closing rate, and inverted ILM flap made it harder to operate. But some new research showed that the inverted ILM flap achieved the same visual outcomes as ILM peeling, it resulted in faster visual acuity improvement and anatomical recovery in the early period [10-12].
In this meta-analysis, we comprehensively and quantitatively compared PPV with inverted ILM flap and ILM peeling in small and medium size MHs, to explore the optimal surgical approach for the treatment of <400μm MHs.
Methods
Search strategy
We cautiously searched for studies that used the inverted ILM flap technique or ILM peeling to treat small and medium size MHs. The PubMed, Web of Science, Embase, Cochrane library, and CNKI databases were systematically searched for all articles including relevant prospective and retrospective clinical trials published before October 2022. The search terms “macular hole OR MH OR macular break” AND “inverted internal limiting membrane flap technique” OR “inverted ILM flap technique” AND” internal limiting membrane peeling” OR “ILM peeling” OR “internal limiting membrane removal” OR “removing the ILM” OR “ILM peel” were searched. To avoid literature omission, we also searched manually.
Inclusion and exclusion criteria
According to the participants, intervention measures, comparison, results, and study design (PICOS) protocol, we used the following criteria: (I) Participants: diagnosed with MH and a minimum diameter of the hole <400 μm; (II) Intervention measures: the experimental group: participants chose PPV combined with inverted ILM flap, the control group: participants chose PPV combined with ILM peeling; (III) Outcome measures: including the effective rate of MH closure, preoperative and postoperative Best Corrected Visual Acuity (BCVA), postoperative ELM and EZ assessment results; (IV) Study design: Prospective randomized controlled trials, retrospective case trials.
The exclusion criteria were as follows: (I) Combination with severe cataract, glaucoma, myopia, retinal detachment, and other eye diseases. (II) Didn’t provide the data required for this meta-analysis; (III) Follow-up time of fewer than 3 months; (IV) Poor quality of literature, missing data, duplicate reports; (V) Reviews or case reports.
Data extraction
Data extraction was independently performed by two investigators, and any discrepancy between the extraction was resolved by discussion or consultation with a third researcher. Data extraction content included: first author, publication year, country, BCVA, follow- up time, and so on.
Quality of assessment
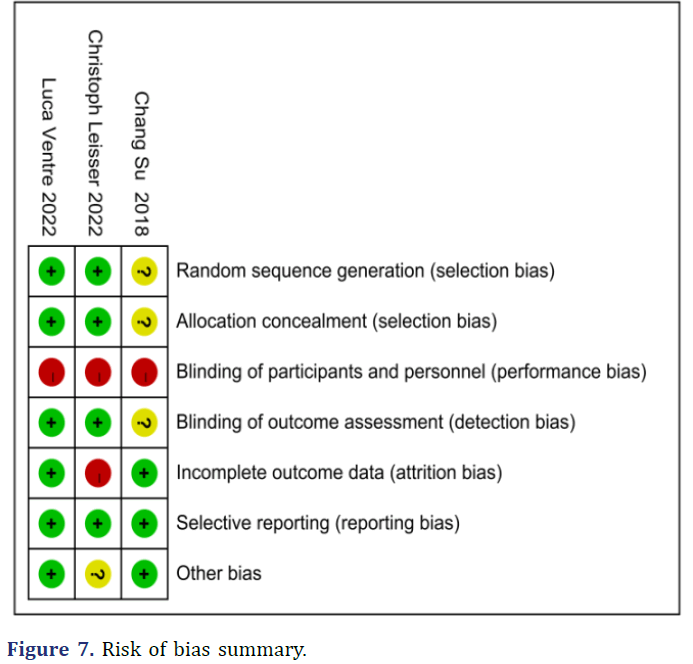
The Randomized Control Trials (RCTs) were evaluated for quality by the “Risk of bias” tool recommended by the Cochrane Handbook 5.1.0. Studies were assessed on seven accepts: “random sequence generation,” “allocation concealment,” “blinding of participants and personnel,” “blinding of outcome assessment,” “incomplete outcome data,” “selective reporting,” and” other bias.” The methodological quality of retrospective case series was assessed based on the Newcastle-Ottawa Scale (NOS). Studies were rated in three areas: selection, comparability, and exposure. Scores ≥ 6 indicated that the quality of research was relatively high.
Statistical analysis
analysis was performed using Review Manager 5.3 software. Cochrane test and I2 statistics were used to assess the heterogeneity of included studies. Values ≥ 50% indicated high heterogeneity, values between 25% and 50% indicated moderate heterogeneity, values between 0% and 25% indicated mild heterogeneity, and I2=0% indicates no heterogeneity [13]. When I2 >50%, a random-effects model was used for data synthesis in the presence of significant heterogeneity, while a fixed-effects model was used when there was no significant heterogeneity. Dichotomous variable data results were stated as Odds Ratio (OR) with a 95% Confidence Interval (CI), while numerical variable data outcomes were recorded as Standardized Mean Difference (SMD) and a 95% CI. Differences were considered statistically significant at P<0.05. Sensitivity analysis was used to verify whether the conclusion of the meta- analysis was robust and credible. Forest diagrams were applied to analyze the results of meta-analysis and funnel plots were applied to evaluate if the results had potential publication bias [14].
Results
Search results
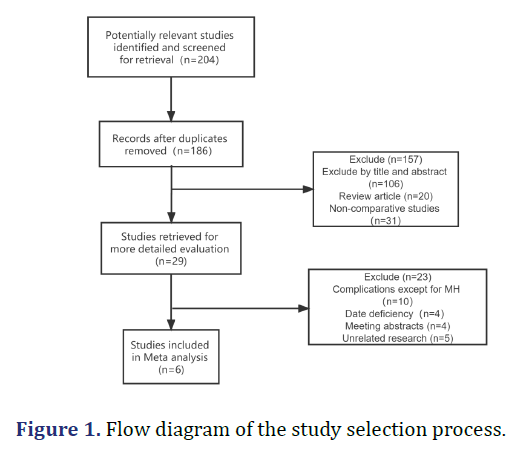
The included literature processed in this meta-analysis is shown in Figure 1. Initially, a total of 204 studies were retrieved. After excluding 175 records by screening the titles and abstracts, a total of 29 articles were considered for more detailed evaluation. We ultimately included 6 studies [15-19] (299 eyes) in our meta-analysis, including 161 eyes in the ILM peeling group and 138 eyes in the inverted ILM flap group. Of these studies, 3 studies [19-21] were retrospective observational studies and 3 studies [16-18] were RCTs. The main characteristics of the included studies were listed in Table 1.
| Study | Year | Country | Group | Trial type | No. of eye | Age | Mean diameter of MH(μm) | Pre-BCVA, logMAR | Post-BCVA, logMAR | Follow up (months) |
|---|---|---|---|---|---|---|---|---|---|---|
| Luca Ventre [16] | 2022 | Italy | ILM flap | A randomized control trial | 25 | 62 | 269 | 0.76 | 0.22 | 1、3、6、12 |
| ILM peeling | 25 | 64 | 254 | 0.72 | 0.19 | 1、3、6、12 | ||||
| Christoph Leisser [17] | 2022 | Austria | ILM flap | A randomized control trial | 7 | 71 | 275 | NA | NA | 3 |
| ILM peeling | 9 | 67 | 244 | NA | NA | 3 | ||||
| Chang Su [18] | 2018 | China | ILM flap | A randomized control trial | 15 | 48.7 | <400 | 1.2 | 0.41 | 1、3、6 |
| ILM peeling | 15 | 48.7 | <400 | 1.34 | 0.45 | 1、3、6 | ||||
| Hung-Da Chou [19] | 2021 | China | ILM flap | A retrospective case trial | 55 | NA | 261.6 | 1.05 | 0.48 | 1、3、6、12 |
| ILM peeling | 62 | NA | 251.9 | 1.05 | 0.51 | 1、3、6、12 | ||||
| Carmen Baumann [20] | 2021 | Germany | ILM flap | A retrospective case trial | 24 | 63.1 | 282 | 0.77 | 0.18 | 3、6、12 |
| ILM peeling | 36 | 70.5 | 238 | 0.74 | 0.26 | 3、6、12 | ||||
| Kanako Yamada [21] | 2022 | Japan | ILM flap | A retrospective case trial | 21 | 66.2 | 278.6 | 0.71 | 0.28 | 1、3、6、12 |
| ILM peeling | 21 | 66.6 | 276 | 0.73 | 0.24 | 1、3、6、12 |
Meta-analysis results
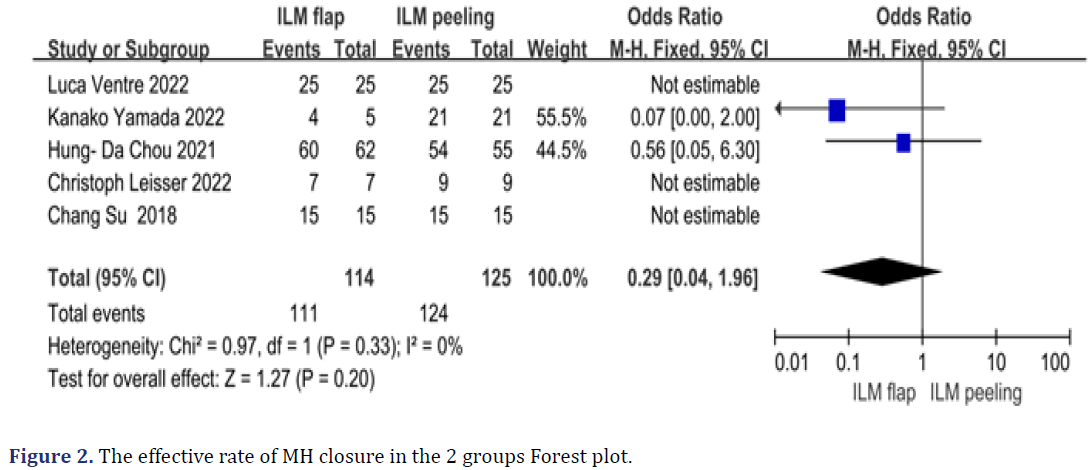
The rate of macular hole closure: Five studies [16- 19, 21] reported the MH closure rate after being treated with ILM peeling or inverted ILM flap. It was 97.3% (111/114 eyes) in the inverted ILM flap group and 99.2% (124/125 eyes) in the ILM peeling group. Due to I2=0%, we chose the fixed-effects model, the analysis showed that the MH closure rate wasn’t significantly different between the two groups (OR=0.29, 95%CI: 0.04~1.96, P=0.33, Figure 2)
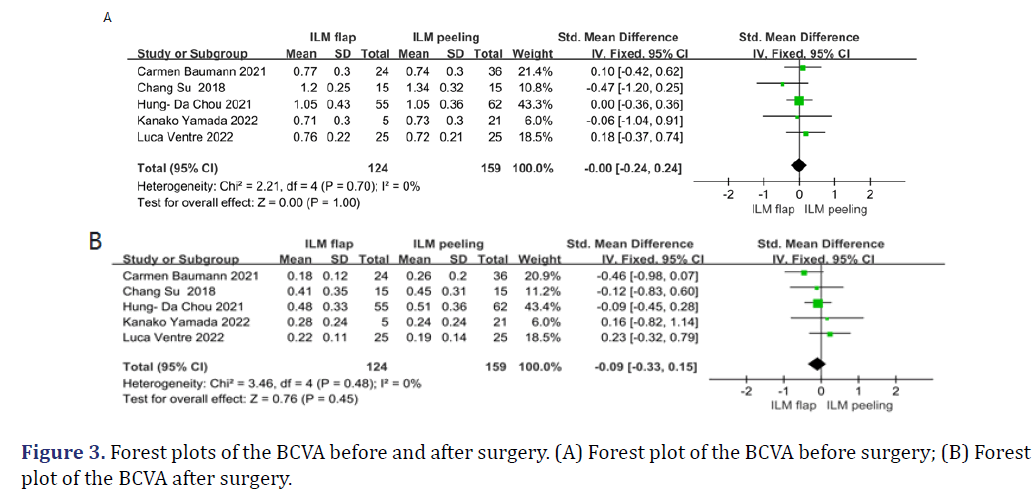
Preoperative and postoperative visual acuity: One of the six trials [17] didn’t report preoperative and postoperative BCVA (converted to log MAR visual acuity for recording), which recorded Distance Corrected Visual Acuity (DCVA), thus the remaining five trials [16, 18-21] were analysed. Merging the data, no heterogeneity was revealed in preoperative BCVA (I2=0%, P=0.70) and postoperative BCVA (I2=0%, P=0.48) in each study, therefore, the fixed-effects model was used. These results suggested that the preoperative BCVA (WMD=-0.00, 95% CI: -0.24~0.24, P=0.70, Figure 3(A) and postoperative BCVA(WMD=-0.09, 95%CI: -0.33~0.15, P=0.48,Figure 3(B)) wasn’t significantly different between two groups (Figure 3).
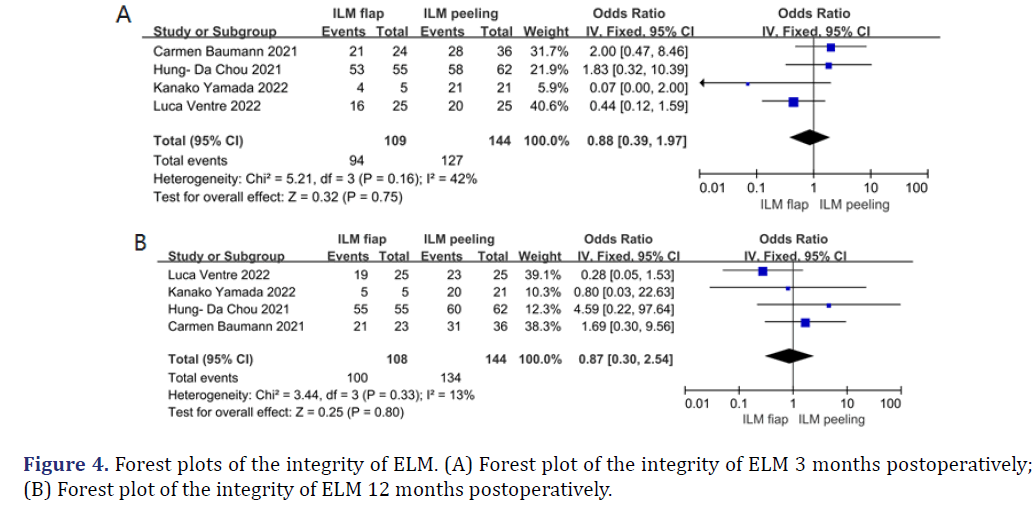
Postoperative ELM recovery: In four of six studies [16, 19-21] that observed the anatomical structure of the retina by Spectral-Domain Optical Coherence Tomography (SD-OCT), we compared the integrity of ELM after surgery in 3 months and 12 months between two groups. The heterogeneity was less than 50%, in which 3 months of I2 was 46% and 12 months of I2 was 13%, we chose the fixed-effects model. The ELM was completely intact in 100/109 (91.7%) eyes of the inverted ILM flap group and 134/144 (93.0%) of the ILM peeling group after 12 months. There was no significant difference in the integrity of the ELM between patients who did or didn’t receive an inverted ILM flap at either 3 months (OR=0.88, 95%CI: 0.39~1.97, P=0.16, Figure 4 (A)) or 12 months (OR=0.87, 95%CI: 0.30~2.54, P=0.33 Figure 4(B)) (Figure 4).
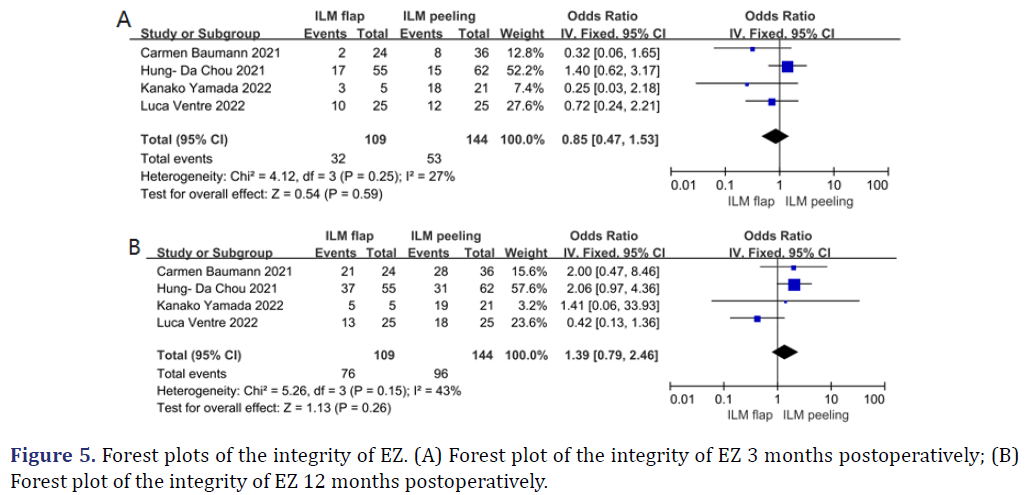
Postoperative E recovery: Four studies [16,19-21] recorded the structure of EZ, we collected 3 months and 12 months postoperatively as well. To merge data, I2 was 27% after 3 months and was 43% after 12 months, these were less than 50%, so the fixed-effects model was analyzed. The EZ was completely intact in 76/109 (69.7%) eyes of the inverted ILM flap group and 96/144 (66.7%) of the ILM peeling group after 12 months. The results showed that absence of significant differences was observed in postoperative EZ recovery between the control group, 3 months (OR=0.85, 95% CI: 0.47~1.53, P=0.25 Figure 5 (A)) and 12 months (OR=1.397, 95% CI: 0.79~2.46, P=0.15 Figure 5 (B), Figure 5).
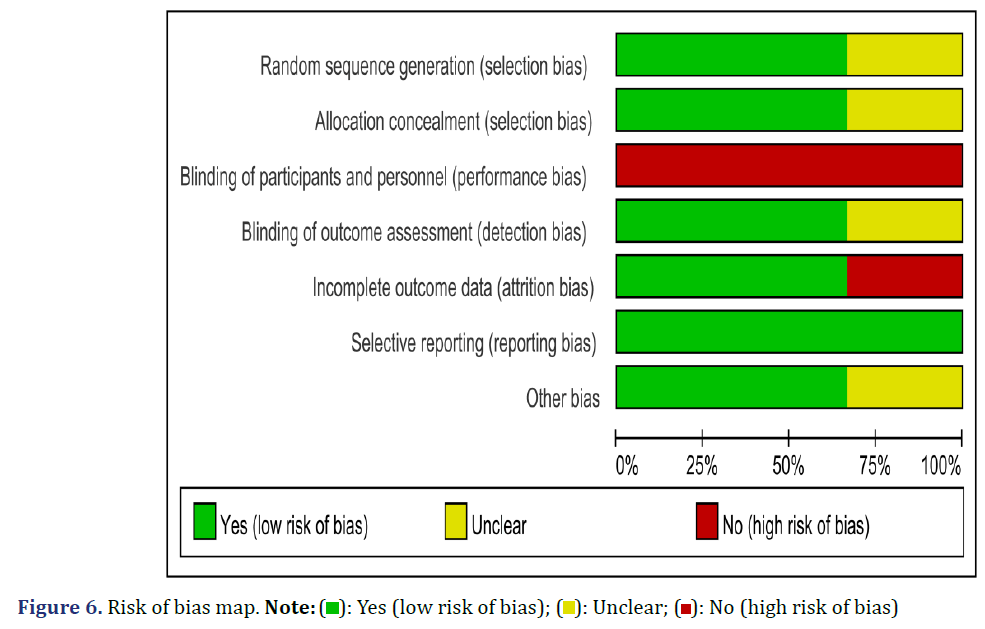
Quality assessment: We assessed the quality of the 3 RCTs [16-18] using Risk of Bias (RoB), which was a Cochrane collaboration tool. The clinical intervention of all included research in our meta-analysis was the surgical operation, so the operators and patients didn’t use blind, but the results may be little affected by performance bias and selective bias. Except this study reported by Leisser Christoph, et al. [17] that had a low risk of bias in all assessing criteria and were assessed as high-quality trials, which had only 1 item with “unclear risk of bias” in Figure 6 and Figure 7. One research [17] was rated a low-quality trial because it missed some follow-up data. For 3 non-randomized controlled trials [19-21], we applied NOS to access the studies’ quality. All research were pointed to 6 stars or above that were high-quality research (Table 2).
| Study (year) | Selection | Comparability | Exposure | Total |
|---|---|---|---|---|
| Hung-Da Chou (2021) | 4 | 1 | 2 | 7 |
| Carmen Baumann (2021) | 4 | 2 | 2 | 8 |
| Kanko Yamada (2022) | 4 | 2 | 2 | 8 |
Sensitivity analysis: As it can be seen from the results of the above analysis, there was heterogeneity between all studies, and we conducted a sensitivity analysis by excluding studies with the largest and least weights to verify the stability of the results. The rate of MH closure, the visual acuity before and after surgery have no heterogeneity, we didn’t conduct sensitivity analysis. When each study was excluded in the meta-analysis of postoperative 3 and 6 months of ELZ and EZ, there was no major change in the consequences. According to sensitivity analysis, all research of our meta-analysis was reliable.
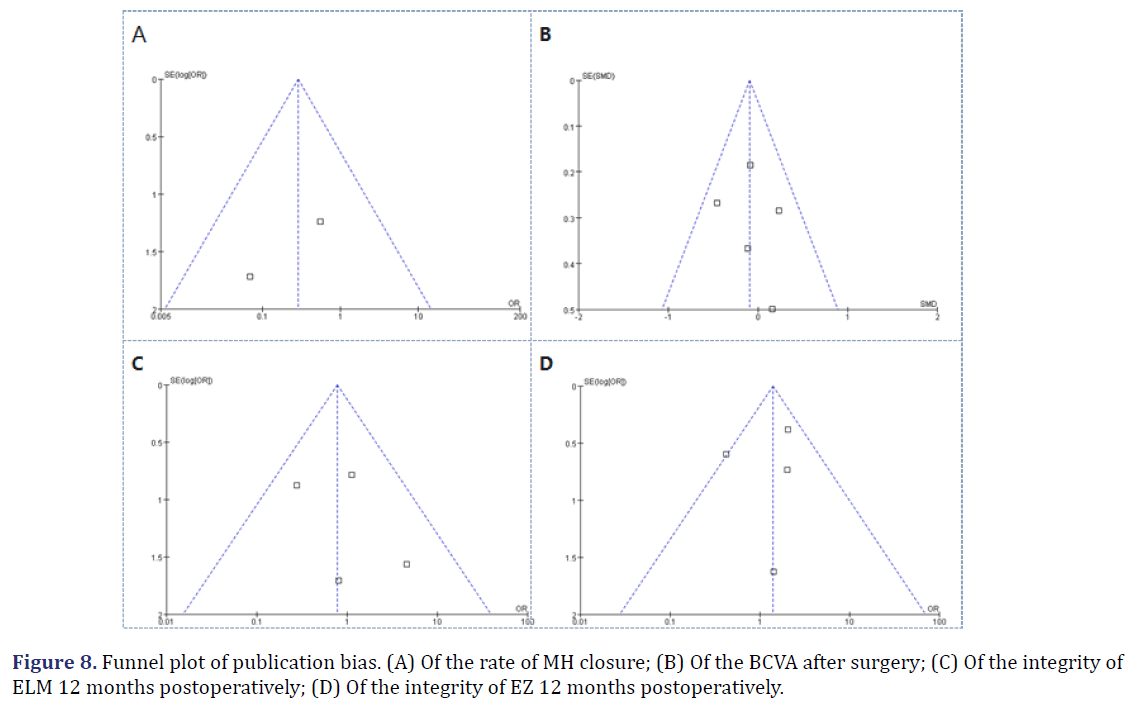
Publication bias analysis: We assessed publication bias of the studies by funnel plots (Figure 8). No statistically significant evidence of publication bias was detected.
Discussion
With the gradual deepening of knowledge about MH and the continuous innovation of various treatment options, there have been gradual improvement in hole closure after MH surgery. Inverted ILM flap technology is considered to be effective in clinical research, especially large MHs, complex MHs, and myopic MHs [9, 22- 24]. Many meta-analysis and systematic reviews have recorded the advantages of the inverted ILM flap. However, there is a lack of such meta-analysis and systematic review: The efficacy of inverted ILM flap and traditional ILM peeling treatment in small and medium size MHs. Thus, we made the first meta-analysis to compare the effective rate of hole closure and visual acuity improvement after surgery between the two groups to more reasonably guide the treatment of small and medium size MHs.
We conducted this systematic review and double-arm meta-analysis of the literature to summarize current evidence, compare the anatomical and visual outcomes of PPV with inverted ILM flap technique or ILM peeling. After pooling the results of the rate of MH closure in these studies, the rate wasn’t different between the flap and peeling groups. Visual acuity was improved obviously in five studies [16, 18-21], but there was no evidence of a difference between the two groups as well. Furthermore, 4 studies [16, 19-21] recorded the healing of the ELM and EZ. The results exhibited an absence of significant variation in the integrity of the ELM or EZ at 3 months and 12 months between patients who received ILM flap or accepted conventional peeling. Our study suggests that inverted ILM flap and ILM peeling are equally effective in treating small and medium size MHs.
The inverted flap technique was first introduced by Michalewska, et al. [25] in 2010 to treat large MH, and they discovered the peeled-off ILM contains Müller cell fragments, which ILM peeling can induce gliosis to enhance closure. Moreover, the inverted ILM flap provided a scaffold for tissue proliferation, in which cells always need a basement membrane to proliferate. The same hypothesis was proved by Kurt Spiteri, et al. [26]. On the one hand, type IV collagen, protein fiber connections, and laminin in the ILM can promote Müller cells proliferation and migration, inducing the retina move towards the center. On the other hand, the ILM flap separated the outer retina from the vitreous, reducing the hydration affection, maintaining the central fovea to reshape, and bringing a good vision outcome [27]. However, there are always controversial about inverted ILM flap. Iwasaki, et al. [28] thought that the ILM flap technique restricted the refractory MH. They observed the poorer anatomical and visual results associated with inverted ILM flap compared with ILM peeling by studying 24 patients of MH. The reason may be different surgical options, they filled some ILM in the hole to cause anatomical damage and scar tissue, thereby leading to a different ending. Our meta-analysis excluded this influence, all surgeons used a single flap to cover the hole in six studies.
We observed ELM and EZ recovery after surgery at 3 months and 12 months in two groups, 3 months replacing short-term effect and 12 months replacing relatively long-term effect. The integrity of the ELM and EZ appeared to have critical roles in the restoration of the photoreceptor microstructures [29]. EZ is the only marker band to determine whether the photoreceptor cells are alive [30]. Some studies have also reported that postoperative ELM and EZ integrity represent a key prognostic factor for photoreceptor layer recovery, which had a positive visual outcome after MH surgery [29, 31-33]. Although the two groups have no obvious difference in our meta-analysis, a continuous ELM could be observed postoperatively of most patients in a short time. A fully regenerated ELM was identified to be essential for EZ regeneration [34, 35]. Our study also validated this finding. Chou, et al. [19] found an earlier restoration of ELM in the inverted flap group compared with conventional ILM peeling: The rate of ELM restoration was higher in the inverted flap group at 1 and 3 months, while this was comparable between the two groups at 12 months. Other research evidenced the same view [36, 37]. Masayuki Horiguchi, et al. [38] compared operated eyes with inverted ILM flap and with normal fellow eyes by multifocal electroretinograms that found the upper retina without the ILM flap and the lower retina covering the ILM flap have no significant difference. These related studies indicated that the inverted ILM flap technology didn’t cause worse functional and morphological outcomes.
Limitations of the Study
Our study has several limitations. Only two RCTs were rated as high-quality, and these studies had small sample sizes and insufficient follow-up time, which may have resulted in certain selection and information biases. Third, due to baseline information inadequacy, such as gender, symptom continuance time, and so on, the effects of various factors weren’t analysed. Further prospective studies with large sample sizes are necessary to validate our study.
Conclusion
In conclusion, there was evidence favouring inverted ILM flap about BCVA at 12 months, final macular hole closure, and retina anatomical structure with no deterioration, it was considered to be equal treatment effective with ILM peeling. Accordingly, this therapeutic approach may be advisable for the treatment of patients with <400 μm MHs.
Acknowledgements
We thank the department of Renmin Hospital of Wuhan University for technical assistance.
Contributions
P.P.L. took part in designing the research, collected the data, analyzed the results and wrote the manuscript. L.L. designed the research, revised the manuscript and supervised all the work. J.H.W. screened titles, abstracts, and full-text articles, abstracted and cleaned data, conducted quality assessment, and solved the disagreements between P.P.L. and L.L., All authors read and provided suggestions during manuscript preparation.
Competing Interests
The authors declare no competing interests.
Additional Information
The datasets generated during and analyzed during the current study are available from the corresponding author on reasonable request.
References
- Gass JD. Idiopathic senile macular hole: Its early stages and pathogenesis. Arch Ophthalmol 1988;106(5):629-639.
[Crossref] [Google Scholar] [PubMed]
- Kelly NE, Wendel RT. Vitreous surgery for idiopathic macular holes: Results of a pilot study. Arch Ophthalmol 1991;109(5):654-659.
[Crossref] [Google Scholar] [PubMed]
- Freeman WR, Azen SP, Kim JW, El-Haig W, Mishell DR, Bailey I. Vitrectomy for the treatment of full-thickness stage 3 or 4 macular holes: Results of a multicentered randomized clinical trial. Arch Ophthalmol 1997;115(1):11-21.
[Crossref] [Google Scholar] [PubMed]
- Korobelnik JF, Hannouche D, Belayachi N, Branger M, Guez JE, Hoang-Xuan T, et al. Autologous platelet concentrate as an adjunct in macular hole healing: A pilot study. Ophthalmology 1996;103(4):590-594.
[Crossref] [Google Scholar] [PubMed]
- Leonard II RE, Smiddy WE, Flynn Jr HW, Feuer W. Long-term visual outcomes in patients with successful macular hole surgery. Ophthalmology 1997;104(10):1648-1652.
[Crossref] [Google Scholar] [PubMed]
- Funata M, Wendel Rt, De La Cruz Ze, Green Wr. Clinicopathologic study of bilateral macular holes treated with pars plana vitrectomy and gas tamponade. Retina 1992;12(4):289-298.
[Crossref] [Google Scholar] [PubMed]
- Duker JS, Kaiser PK, Binder S, de Smet MD, Gaudric A, Reichel E, et al. The International Vitreomacular Traction Study Group classification of vitreomacular adhesion, traction, and macular hole. Ophthalmology 2013;120(12):2611-2619.
[Crossref] [Google Scholar] [PubMed]
- Michalewska Z, Michalewski J, Dulczewska-Cichecka K, Adelman RA, Nawrocki J. Temporal inverted internal limiting membrane flap technique versus classic inverted internal limiting membrane flap technique: A comparative study. Retina 2015;35(9):1844-1850.
[Crossref] [Google Scholar] [PubMed]
- Mahalingam P, Sambhav K. Surgical outcomes of inverted internal limiting membrane flap technique for large macular hole. Indian J Ophthalmol 2013;61(10):601-603.
[Crossref] [Google Scholar] [PubMed]
- Velez-Montoya R, Ramirez-Estudillo JA, Sjoholm-Gomez de Liano C, Bejar-Cornejo F, Sanchez-Ramos J, Guerrero-Naranjo JL, et al. Inverted ILM flap, free ILM flap and conventional ILM peeling for large macular holes. Int J Retina Vitreous 2018;4(1):1-9.
[Crossref] [Google Scholar] [PubMed]
- Shen Y, Lin X, Zhang L, Wu M. Comparative efficacy evaluation of inverted internal limiting membrane flap technique and internal limiting membrane peeling in large macular holes: A systematic review and meta-analysis. BMC Ophthalmol 2020;20(1):1-10.
[Crossref] [Google Scholar] [PubMed]
- Yu JG, Wang J, Xiang Y. Inverted internal limiting membrane flap technique versus internal limiting membrane peeling for large macular holes: A meta-analysis of randomized controlled trials. Ophthalmic Res 2021;64(5):713-722.
[Crossref] [Google Scholar] [PubMed]
- Ioannidis JP, Patsopoulos NA, Evangelou E. Heterogeneity in meta-analyses of genome-wide association investigations. PloS one 2007;2(9):e841.
[Crossref] [Google Scholar] [PubMed]
- Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. Bmj 1997;315(7109):629-634.
[Crossref] [Google Scholar] [PubMed]
- Baumann C, Kaye S, Iannetta D, Sultan Z, Dwivedi R, Pearce I, et al. Effect of inverted internal limiting membrane flap on closure rate, postoperative visual acuity, and restoration of outer retinal layers in primary idiopathic macular hole surgery. Retina 2020 ;40(10):1955-1963.
- Ventre L, Fallico M, Longo A, Parisi G, Russo A, Bonfiglio V, et al. Conventional internal limiting membrane peeling versus inverted flap for small-to-medium idiopathic macular hole: A randomized trial. Retina 2022;42(12):2251-2257.
[Crossref] [Google Scholar] [PubMed]
- Leisser C, Ruiss M, Pilwachs C, Findl O. ILM peeling with ILM flap transposition vs. classic ILM peeling for small and medium macula holes—a prospective randomized trial. Spektrum Augenheilkd 2023;37(1):9-14.
[Crossref] [Google Scholar] [PubMed]
- Chang Su. Analysis of the efficacy of two different surgical procedures for treating MH. Hebei medicine 2018;24:973.
- Chou HD, Liu L, Wang CT, Chen KJ, Wu WC, Hwang YS, et al. Single-layer inverted internal limiting membrane flap versus conventional peel for small-or medium-sized full-thickness macular holes. Am J Ophthalmol 2022;235:111-119.
[Crossref] [Google Scholar] [PubMed]
- Baumann C, Dervenis N, Kirchmair K, Lohmann CP, Kaye SB, Sandinha MT, et al. Functional and morphological outcomes of the inverted internal limiting membrane flap technique in small-sized and medium-sized macular holes< 400 µm. Retina 2021;41(10):2073-2078.
- Yamada K, Oishi A, Kusano M, Kinoshita H, Tsuiki E, Kitaoka T. Effect of inverted internal limiting membrane flap technique on small-medium size macular holes. Scientific Reports 2022;12(1):731.
- Kase S, Saito W, Mori S, Saito M, Ando R, Dong Z, et al. Clinical and histological evaluation of large macular hole surgery using the inverted internal limiting membrane flap technique. Clinical ophthalmology 2016;11:9-14.
[Crossref] [Google Scholar] [PubMed]
- Narayanan R, Singh SR, Taylor S, Berrocal MH, Chhablani J, Tyagi M, et al. Surgical outcomes after inverted internal limiting membrane flap versus conventional peeling for very large macular holes. Retina 2019;39(8):1465-1469.
[Crossref] [Google Scholar] [PubMed]
- Rizzo S, Tartaro R, Barca F, Caporossi T, Bacherini D, Giansanti F, et al. Internal limiting membrane peeling versus inverted flap technique for treatment of full-thickness macular holes: A comparative study in a large series of patients. Retina 2018;38:S73-78.
[Crossref] [Google Scholar] [PubMed]
- Michalewska Z, Michalewski J, Adelman RA, Nawrocki J. Inverted internal limiting membrane flap technique for large macular holes. Ophthalmology 2010;117(10):2018-2025.
[Crossref] [Google Scholar] [PubMed]
- Cornish KS, Lois N, Scott NW, Burr J, Cook J, Boachie C, et al. Vitrectomy with internal limiting membrane peeling versus no peeling for idiopathic full-thickness macular hole. Ophthalmology 2014;121(3):649-655.
[Crossref] [Google Scholar] [PubMed]
- Shiode Y, Morizane Y, Matoba R, Hirano M, Doi S, Toshima S, et al. The role of inverted internal limiting membrane flap in macular hole closure. Invest Ophthalmol Vis Sci 2017;58(11):4847-4855.
[Crossref] [Google Scholar] [PubMed]
- Iwasaki M, Kinoshita T, Miyamoto H, Imaizumi H. Influence of inverted internal limiting membrane flap technique on the outer retinal layer structures after a large macular hole surgery. Retina 2019;39(8):1470-1477.
[Crossref] [Google Scholar] [PubMed]
- Landa G, Gentile RC, Garcia PM, Muldoon TO, Rosen RB. External limiting membrane and visual outcome in macular hole repair: Spectral domain OCT analysis. Eye(Lond) 2012;26(1):61-69.
[Crossref] [Google Scholar] [PubMed]
- Chalam KV, Murthy RK, Gupta SK, Brar VS, Grover S. Foveal structure defined by spectral domain optical coherence tomography correlates with visual function after macular hole surgery. Eur J Ophthalmol. 2010;20(3):572-577.
[Crossref] [Google Scholar] [PubMed]
- Wakabayashi T, Fujiwara M, Sakaguchi H, Kusaka S, Oshima Y. Foveal microstructure and visual acuity in surgically closed macular holes: spectral-domain optical coherence tomographic analysis. Ophthalmology 2010;117(9):1815-1824.
[Crossref] [Google Scholar] [PubMed]
- Bottoni F, Parrulli S, Mete M, D’Agostino I, Cereda M, Cigada M, et al. Large idiopathic macular hole surgery: remodelling of outer retinal layers after traditional internal limiting membrane peeling or inverted flap technique. Ophthalmologica 2020;243(5):334-341.
[Crossref] [Google Scholar] [PubMed]
- Itoh Y, Inoue M, Rii T, Hiraoka T, Hirakata A. Significant correlation between visual acuity and recovery of foveal cone microstructures after macular hole surgery. Am J Ophthalmol 2012;153(1):111-119.
[Crossref] [Google Scholar] [PubMed]
- Iwasaki M, Ando R, Aoki S, Miyamoto H. Restoration process of the outer retinal layers after surgical macular hole closure. Retina 2022;42(2):313-320.
[Crossref] [Google Scholar] [PubMed]
- Yang J, Xia H, Liu Y, Wang X, Yuan H, Hou Q, et al. Ellipsoid zone and external limiting membrane-related parameters on spectral domain-optical coherence tomography and their relationships with visual prognosis after successful macular hole surgery. Front Med (Lausanne) 2021;8:779602.
[Crossref] [Google Scholar] [PubMed]
- Ramtohul P, Parrat E, Denis D, Lorenzi U. Inverted internal limiting membrane flap technique versus complete internal limiting membrane peeling in large macular hole surgery: A comparative study. BMC ophthalmol 2020;20(1):1-8.
[Crossref] [Google Scholar] [PubMed]
- Hu XT, Pan QT, Zheng JW, Zhang ZD. Foveal microstructure and visual outcomes of myopic macular hole surgery with or without the inverted internal limiting membrane flap technique. Br J Ophthalmol 2019;103(10):1495-1502.
[Crossref] [Google Scholar] [PubMed]
- Horiguchi M, Tanikawa A, Mizuguchi T, Tanaka H, Sugimoto M, Shimada Y, et al. The effect of an inverted internal limiting membrane flap on retinal function after macular hole surgery. Ophthalmol Retina 2017;1(5):421-427.
[Crossref] [Google Scholar] [PubMed]
Copyright: © 2023 The Authors. This is an open access article under the terms of the Creative Commons Attribution Non Commercial Share Alike 4.0 (https://creativecommons.org/licenses/by-nc-sa/4.0/) This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.








 ): Yes (low risk of bias); (
): Yes (low risk of bias); ( ): Unclear; (
): Unclear; ( ): No (high risk of bias)
): No (high risk of bias)