Research Article - Archives of Clinical and Experimental Surgery (2023)
Is Configuration of the Orifice A Better Predictor of Success in Endoscopic Management of Vesicoureteric Reflux?: A Pilot Study
Vinod Raj*, Ram Mohan Shukla, Maneesh Kumar Joleya, Pooja Tiwari, Shashi Shankar Sharma, Ashok K Laddha, Manoj Joshi and Brijesh K LahotiVinod Raj, Department of Pediatric Surgery, MGM Medical College, Indore, India, Email: doc.vraj89@gmail.com
Received: 14-Jul-2023, Manuscript No. EJMACES-23-111132; Editor assigned: 17-Jul-2023, Pre QC No. EJMACES-23-111132 (PQ); Reviewed: 31-Jul-2023, QC No. EJMACES-23-111132; Revised: 07-Aug-2023, Manuscript No. EJMACES-23-111132 (R); Published: 14-Aug-2023
Abstract
Introduction: Management of Vesico Ureteral Reflux (VUR) has always been dictated by grade of reflux, higher the grade of reflux, lesser the inclination towards Endoscopic Management Vesico Ureteral Reflux (EMVUR). Results published from world-wide have shown that large number of high-grade refluxes are amenable to EMVUR while results with all lower grades of reflux is not uniformly successful. So, there are more factors at play than just grade of reflux which contributes to successful EMVUR. With this in mind, we formulated two hypotheses. 1. The radiological grade of VUR does not always correlate to the cystoscopic configuration of the orifice. 2. The configuration of the orifice is a better predictor of success than grade of reflux in EMVUR. This is a pilot study to confirm our hypotheses.
Materials and methods: A retrospective observational study. Cases of primary VUR with breakthrough Urinary Tract Infection (UTI) on antibiotic prophylaxis were subjected to EMVUR. All cases treated by single surgeon at same institute. Data regarding age, gender, pre-operative Micturating Cysto-Urethrogram (MCU), intraoperative cystoscopic video, post-operative MCU were collected and only those patients with all above data included in analysis.
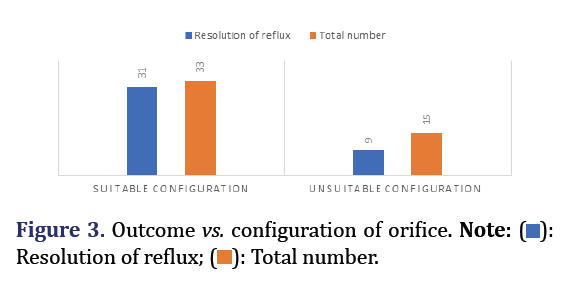
Observations: 48 Renal Refluxing Units (RRU) included which ranged between grade 2 to grade 4. Among these, 40 were treated successfully by EMVUR. Among 48 orifices, 33 were termed as suitable and 15 as unsuitable configuration. The success of EMVUR was statistically more significant when compared with configuration of orifice rather than grade of reflux.
Conclusion: This pilot study proved our hypotheses beyond doubt. Cystoscopic grading of ureteric orifice before EMVUR is necessary to predict successful outcome.
Keywords
Vesicoureteric reflux; Endoscopic management; Cystoscopic grading; Ureteric orifice
Introduction
Vesicoureteric reflux is the most common urological abnormality encountered in the pediatric surgical practice [1]. The spontaneous resolution of VUR is reported in children below the age of 5 years and this depends on the grade of reflux and the type of ureteric orifice [2]. The need for surgical invention arises when there is breakthrough UTI on antibiotic prophylaxis. The surgical management has always been dictated by grade of reflux, higher the grade lesser is the inclination towards endoscopic management vs. open surgical procedures [3].
In the recent decade, having treated increasing number of VUR endoscopically, we observed that the radiological grade of reflux does not always correlate to cystoscopic appearance of ureteric orifice. In simple words, we noted cases which had grade 2 reflux on MCU had a wide patulous ureteric orifice while cases of grade 4 reflux had a “normal” looking ureteric orifice. The post-operative outcomes of these scenarios compelled us to think and we came up with two hypotheses.
- The cystoscopic configuration of ureteric orifice does not always correlate with radiological grade of reflux on MCU.
- The cystoscopic configuration of ureteric orifice is a better predictor of success than grade of reflux following endoscopic management.
With these observations and hypotheses, we anticipated that there is more than just grade of reflux which is influencing the outcomes of endoscopic injections and we went on a quest to discover these probable factors at play.
Materials and Methods
This is a retrospective observational study. All the cases with primary VUR with breakthrough UTI on antibiotic prophylaxis were subjected to endoscopic management. All these cases were treated by single surgeon at the same institute. The data regarding the age, gender, pre-operative MCU, intraoperative cystoscopic video, post-operative MCU were collected and only those patients with all the above data were included in the analysis.
The intraoperative cystoscopic video of the procedure were analysed by the principle investigator without the knowledge of the post procedure outcome and identity of the patient. Based on the cystoscopic appearance of the ureteric orifice, these were categorised into two groups. First were the suitable configuration where the orifice was facing towards the camera, the rim of the orifice was clearly seen, and injection could be placed easily underneath such orifices irrespective of the size of the ureteric opening. The second group were that who were facing laterally, present ectopically or on a mound and it was difficult for placing the injecting needle underneath them irrespective of the size of ureteric orifice.
- Suitable configuration: Facing the camera, entire rim seen, easy for injection.
- Unsuitable configuration: Facing laterally, present on a mound, difficult to injection.
The pre-operative radiological grade and assigned ureteric orifice configuration were compared to find out the coefficient of correlation between the two. Further the post procedure outcome on MCU was compared with the cystoscopic configuration of ureteric orifice and radiological grade of reflux on MCU separately. All the data were tabulated and analysed using SPSS 23. Linear regression and logistic regression tests were applied to test our hypotheses.
Observations and Results
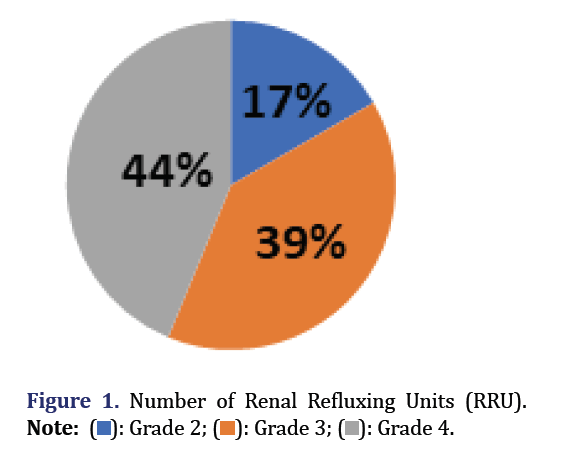
There were a total of 48 renal refluxing units which were treated satisfying the above inclusion criteria. Of these, 8 were of grade 2, 19 were of grade 3 and 21 belonged to grade 4 VUR (Figure 1). After going through their cystoscopic videos, these ureteric orifices were classified into suitable and unsuitable configuration based on the above definitions. Among the 48 orifices, 33 orifices were termed as suitable configuration while the rest were classified as unsuitable. Of the 48 RRU, 40 were treated successfully by endoscopic management while the rest 8 opted for open surgical management after a failed injection.
We have tabulated the pre-operative MCU, intra-operative cystoscopic appearance of orifice and post-operative outcome following injection. In this table, the reader can find the discordance between MCU grade of reflux and cystoscopic appearance of orifice vividly which is in favour of first hypotheses (Supplementary Table 1). To assess our second hypothesis, we analysed the rates of resolution taking into consideration the radiological grade of reflux and cystoscopic configuration of orifice separately.
Coming to our results, with respect to grade of reflux, all the 8 grade 2 refluxes resolved and 16 RRU resolved among 19 grade 3 and 21 grade 4 reflux (Figure 2). With respect to configuration of orifice, 31 of 33 suitable configuration resolved while only 9 of the 15 unsuitable configuration resolved (Figure 3). Statistically, this translated into chi-square tests being positive for configuration of orifice with a p value of 0.003 (Tables 1 and 2) when compared to grade of reflux which had a p value of 0.304 (Tables 3 and 4). So, this proves our other hypothesis that configuration of orifice is a better predictor of success than grade of reflux in endoscopic management of VUR.
| Outcome | Suitable | Unsuitable | Total |
|---|---|---|---|
| Resolved | 31 | 9 | 40 |
| Persistent | 2 | 6 | 8 |
| Total | 33 | 15 | 48 |
| Value | Df. | Asymp. sig | |
|---|---|---|---|
| Pearson chi-square | 8.553 | 1 | 0.003 |
| Continuity correlation | 6.284 | 1 | 0.12 |
| Likelihood ratio | 7.974 | 1 | 0.005 |
| Valid cases | 48 |
| Outcome | Grade 2 | Grade 3 | Grade 4 | Total |
|---|---|---|---|---|
| Resolved | 8 | 16 | 16 | 40 |
| Persistent | 0 | 3 | 5 | 8 |
| Total | 8 | 19 | 21 | 48 |
| Value | df | Asymp. sig | |
|---|---|---|---|
| Pearson chi-square | 2.382 | 2 | 0.304 |
| Continuity correlation | 3.627 | 2 | 0.163 |
| Likelihood ratio | 2.221 | 1 | 0.138 |
| Valid cases | 48 |
Discussion
The rates of resolution of reflux following endoscopic management varies across different studies and different grades of reflux [4]. Higher rates of resolution are seen in higher grades of reflux as reported by Puri et al. [5]. Recently published results from Rao et al. also showed higher resolution rate in higher grade reflux [6]. This is in contrast with the earlier seen results which had poor success rate in higher grade of reflux. Although the technique of injection has improved with improved cystoscopes with better vision and better implantable materials, we feel there is more than just grade of reflux which predicts successful outcome following endoscopic management and we are on a quest to find out these probable factors at work.
Radiological grade of reflux on MCU depends on the degree of dilatation of ureters and the extent of reflux into the renal system [7]. This indirectly indicates the propensity for developing pyelonephritis. The principle of surgical correction of VUR, which is creating a submucosal tunnel and muscle backing, depends on the size of bladder and dilatation of ureters which is seen on an MCU [8]. The principle of endoscopic management is creating a backing for the intramural ureteric wall by injection of implant which is influenced by clear visualization of orifice [9]. Hence, logically, for successful injection, orifice configuration is more important than radiological grade of VUR.
There are very few studies available in the literature which talks about the effects of configuration of orifice or location of the orifice. The two studies that we came across are Yucel et al. and Alizadeh et al. which focus on the location of orifice and configuration of the orifice respectively. Yucel et al. concluded by saying that laterally placed ureteric orifice may decrease the efficacy of injection due to greater likelihood of a faculty injection while Alizadeh et al. found no relationship between configuration of orifice and resolution of reflux [10, 11].
We would like to point out to the readers that the configurations which Alizadeh et al. took into consideration were the types of ureteric orifices laid down by Lyon et al. and not the configuration that we are stressing upon in this study [2]. The present study, although being a retrospective analysis, has shown that there is more than just radiological grade of reflux on MCU which decides the outcome of endoscopic management.
Cystoscopic grading of ureteric orifice before performing endoscopic management is necessary to predict a successful outcome. This comprises the configuration of orifice which can be either suitable or unsuitable, with suitable configuration faring better than unsuitable.
We are currently performing a prospective trial to validate our hypotheses and build a scoring system, which would include cystoscopic configuration of ureteric orifice and radiological grade of reflux on MCU, helping us to construct a guideline to recommend either endoscopic management or open surgical management for each case of VUR.
Conclusions
This pilot study proves both our hypotheses that cystoscopic configuration of orifice does not always correlate with radiological grade of VUR and Cystoscopic configuration of orifice is a better predictor of success than radiological grade of VUR in endoscopic management beyond doubt. This directs future research with larger numbers, standardization of definitions for categorizing the ureteric orifice configuration.
Ethical Consideration
Institutional Ethics Committee approval obtained for the study dated 5th June 2019.
Acknowledgment
None to declare
Funding/Support
None to declare
Conflict of Interest
None to declare
References
- Routh JC, Vandersteen DR, Pfefferle H, Wolpert JJ, Reinberg Y. Single center experience with endoscopic management of vesicoureteral reflux in children. J Urol 2006;175(5):1889-1893.
[Crossref] [Google Scholar] [Pubmed]
- Lyon RP, Marshall S, Tanagho EA. The ureteral orifice: Its configuration and competency. J Urol 1969;102(4):504-509.
[Crossref] [Google Scholar] [Pubmed]
- Yap TL, Chen Y, Nah SA, Ong CC, Jacobsen A, Low Y, et al. STING versus HIT technique of endoscopic treatment for vesicoureteral reflux: A systematic review and meta-analysis. J Pediatr Surg 2016;51(12):2015-2020.
[Crossref] [Google Scholar] [Pubmed]
- Kirsch AJ, Arlen AM. Evaluation of new Deflux administration techniques: intraureteric HIT and Double HIT for the endoscopic correction of vesicoureteral reflux. Expert Rev Med Devices 2014;11(5):439-446.
[Crossref] [Google Scholar] [Pubmed]
- Chertin B, de Caluwé D, Puri P. Endoscopic treatment of primary grades IV and V vesicoureteral reflux in children with subureteral injection of polytetrafluoroethylene. J Urol 2003 1;169(5):1847-1879.
[Crossref] [Google Scholar] [Pubmed]
- Rao KL, Menon P, Samujh R, Mahajan JK, Bawa M, Malik MA, et al. Endoscopic Management of Vesicoureteral Reflux and Long-term Follow-up. Indian Pediatri 2018;55(12):1046-1049.
[Google Scholar] [Pubmed]
- Lebowitz RL, Olbing H, Parkkulainen KV, Smellie JM, Tamminen-Möbius TE. International system of radiographic grading of vesicoureteric reflux. Pediatr Radiol 1985;15:105-109.
[Crossref] [Google Scholar] [Pubmed]
- Dewan PA. Ureteric reimplantation: A history of the development of surgical techniques. BJU Int 2000;85(8):1000-1006.
[Crossref] [Google Scholar] [Pubmed]
- Läckgren G. Endoscopic treatment of vesicoureteral reflux: Current status. Indian J Urol 2009;25(1):34-39.
[Crossref] [Google Scholar] [Pubmed]
- Yucel S, Ucar M, Guntekin E, Kukul E, Melikoglu M, Baykara M, et al. The effect of location of the ureteric orifice on the efficacy of endoscopic injection to correct vesico‐ureteric reflux. BJU Int 2005;95(9):1314-1318.
[Crossref] [Google Scholar] [Pubmed]
- Alizadeh F, Shahdoost AA, Zargham M, Tadayon F, Joozdani RH, Arezegar H, et al. The influence of ureteral orifice configuration on the success rate of endoscopic treatment of vesicoureteral reflux. Adv Biomedi Res 2013;2:1.
[Crossref] [Google Scholar] [Pubmed]