Research Article - Archives of Clinical and Experimental Surgery (2024)
Laparoscopic Approach to Acute Abdomen: A Multicenter Study
Abdelmoneim Mohammed Ali Eljacki*Abdelmoneim Mohammed Ali Eljacki, Sudan Medical Specializaion Board, Khartoum, Sudan, Tel: +249912479792, Email: Yousifdafair@yahoo.com
Received: 13-Mar-2024, Manuscript No. EJMACES-24-129343; Editor assigned: 15-Mar-2024, Pre QC No. EJMACES-24-129343 (PQ); Reviewed: 29-Mar-2024, QC No. EJMACES-24-129343; Revised: 05-Apr-2024, Manuscript No. EJMACES-24-129343 (R); Published: 15-Apr-2024
Abstract
Background: Laparoscopy has become a routine procedure in managing acute abdominal disease and can be considered an excellent therapeutic and additional diagnostic tool in selected cases.
Objective: To identify the diagnostic and therapeutic value of laparoscopy in the management of acute abdomen in Khartoum state.
Methods: The study was a prospective, descriptive, cross-sectional hospital-based study. Conducted in Six centers around Khartoum state, in a period from October 2017 to October 2018. Patients whose laparoscopy was used for either diagnostic or therapeutic purposes in Acute abdomen were selected.
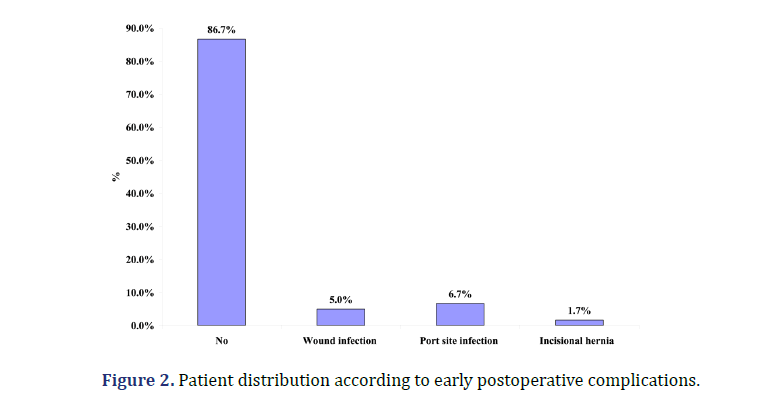
Results: The mean age was 29 ± 2.3 years. The duration of symptoms in 42 (70%) of the patients was 24-48 hours. The common three clinical diagnosis were acute cholecystitis 18 (30%), acute appendicitis 13 (21.7%) and uncertain diagnosis 11 (18.3%). The most common operative findings were pathology of the appendix 14 (23.3%) and gallbladder 14 (23.3%). Sensitivity, specificity, and accuracy of laparoscopy in the acute abdomen were 93.5%, 42.9%, and 81.8% respectively. Indicate good sensitivity specificity and high accuracy. The only reported immediate complication of the laparoscopic approach was bleeding in one patient. Unnecessary laparotomy was avoided in 10 cases (16.6%), 3 lap adhesiolysis, 4 cases of perforated duodenal ulcer,3 out of them found sealed, and in 1 case graham patch was done . 1 case of foreign body(pin) removal after trauma with pin gun, 1 case of ectopic pregnancy and I case of cholecystostomy tube. Diagnosis was confirmed in 11 (18.3%) of cases which were put in the category of uncertain diagnosis preoperatively.The reported late complications were port site infection 4 (6.7%), and incisional hernia 1 (1.7%). The duration of surgery was less than 2 hours in 38 (63.3%). 47 (78.3%) of the patients started oral feeding in less than 24 hours. Hospital stays in 48(80%) of the patients were 1-2 days.
Conclusion: The emergency laparoscopy for the acute abdomen is safe and accurate; these techniques reduce the rate of unnecessary laparotomy and avoid a delay in diagnosis.
Keywords
Acute abdomen; Laparoscopy; Obstruction; Peritonitis
Introduction
Laparoscopy is used frequently in the diagnosis and treatment of acute abdominal pain. It’s particularly helpful in the evaluation of women with right lower quadrant pain and can prevent unnecessary laparotomy in case of diagnostic uncertainty. [1] In the last decade, laparoscopy was used frequently during emergency surgery. In 2006 the European Association for Endoscopic Surgery (EAES) published a consensus statement supported by evidence for the use of laparoscopy in abdominal emergencies.
EAES decided to revisit the clinical recommendations for the role of laparoscopy in abdominal emergencies in adults, with the primary intent being to update the EAES indications and supplement the existing guidelines on specific diseases and to attain the following objectives:
1. Establish the preferred diagnostic procedures, selection of patients, if applicable, and the suitability of the laparoscopic approach responsible for acute abdominal disease settings.
2. Assess the indication, morbidity, duration of hospital stays, costs, and recovery time from laparoscopic treatment for acute abdominal settings.
3. Define the optimal practice in laparoscopy for each abdominal emergency and provide recommendations that reflect good practice [2].
Clinical examination often fails to yield a diagnosis, particularly when the symptoms and signs are compounded by obesity. This problem is more common, in but not exclusive to, female patients. Blood investigations may be diagnostic for acute pancreatitis, but in most other scenarios, they simply indicate the presence of an inflammatory process. Radiology may suggest a diagnosis, but both radiography and ultrasound have a false-negative rate [3].
The role of diagnostic and therapeutic laparoscopy in the acute abdomen is now well established. Compared to preoperative radiological investigation or a watch-and-wait policy, laparoscopy yields an accurate diagnosis in more patients. It also provides greater visualization of other intra-abdominal organs in patients undergoing gridiron incision for appendectomy although laparoscopy is not a substitute for good clinical judgment; early laparoscopy reduces the incidence of negative laparotomy and serious complications and helps in planning abdominal incisions [4].
In Sudan laparoscopic surgery was introduced in 1995, was limited to a few centers and procedures mainly involve elective cholecystectomy. Currently, the use of laparoscopy spreads all over the country and major centers facilitate more advanced procedures [5].
Materials and Methods
This is a descriptive observational study conducted in major Sudanese Private hospitals; Albaraha Hospital, Alsaha Hospital, Alzytona Hospital, Royal Care Hospital, and Doctors Clinic, in the period from October 2017 to October 2018. All the hospitals mentioned above have well-equipped laparoscopy instruments and the consultant Surgeons are trainees in performing laparoscopic procedures. Patients were studied to understand the common site of abdominal pain, duration of the symptoms, Associated conditions, Indications, and contraindications for the laparoscopic approach in acute abdominal conditions, and patients’ factors that favor the laparoscopic approach and outcomes.
Inclusion and exclusion criteria
We include all Patients who underwent laparoscopic procedures for acute abdominal pain in the above-mentioned hospitals during the study period and had diagnostic/therapeutic laparoscopy to investigate Acute abdominal conditions such as Acute abdominal infections, perforations, and trauma surgery as well. Exclusion criteria are Patients who underwent open procedures and patients who were unwilling to participate in the study.
Data was collected using a structured questionnaire. All patients were followed up at the outpatient clinic in r 4-6 weeks from discharge, to assess their recovery and elicit any complications. A successful therapeutic procedure is the ability of the surgeon to complete the procedure without any need to convert to an open procedure or develop intra or early post-operative complications.
Data were analyzed with Statistical Package for the Social Sciences (SPSS) version 24. Qualitative data were analyzed using a correlation test and simple linear regression, and the P-value was considered significant if less than 0.05. Written informed consent was obtained from each participant, and ethical clearance was obtained from the ethical committee of the Sudan Medical Specialization Board, as well as hospital administration approval.
Results
The most common age group was between (15-30) years 24 (40%), with a male-to-female ratio of (25 (41.7%) to 35 (58.3%). Many of the patients were married 38 (63.3%) (Table 1). The two common sites of abdominal pain were right hypochondria 23 (38.3%) and RIF pain 22 (36.7%). In most of the patients 42 (70%) the duration of symptoms was 24-48 hours. Abdominal pain is the most common presenting symptom. Moreover, dull aching was the common character of pain in 33 (55%) followed by colicky 23 (38.3%) and stabbing 4 (6.7%) (Table 2). Furthermore, the other reported symptoms are vomiting 59 (98.3%), nausea 56 (93.3%), fever 53 (88.3%), and abdominal distension 7 (11.7%) (Table 3). History of similar condition was reported in 29 (48.3%) of the patients, and history of abdominal surgery included C/S 11 (18.3%), appendectomy 3 (5%), and Laparoscopic cholecystectomy (1.7%) were also elicited. The reported co-morbidities were diabetes mellitus 17 (28.3%), hypertension 3 (5%), asthma 2 (3.3%), and Alzheimer’s 1 (1.7%) (Figure 1).
| N | % | ||
|---|---|---|---|
| Age group | 15-30 years | 24 | 40 |
| 31-40 years | 18 | 30 | |
| 51-60 years | 9 | 15 | |
| 41-50 years | 6 | 10 | |
| <15 years | 3 | 5 | |
| Total | 60 | 100 | |
| Gender | Male | 25 | 41.7 |
| Female | 35 | 58.3 | |
| Total | 60 | 100 | |
| Marital status | Married | 38 | 63.3 |
| Single | 22 | 36.7 | |
| Total | 60 | 100 |
| N | % | ||
|---|---|---|---|
| Site of abdominal pain | |||
| RT hypochondria | 23 | 38.3 | |
| RIF pain | 22 | 36.7 | |
| Epigastric | 8 | 13.3 | |
| Central | 4 | 6.7 | |
| Lower abdomen | 3 | 5 | |
| Total | 60 | 100 | |
| Duration of symptom | 24-48 hrs | 42 | 70 |
| 48-72 hrs | 9 | 15 | |
| 6-12 hrs | 4 | 6.7 | |
| 12-24 hrs | 4 | 6.7 | |
| 1-6 hrs | 1 | 1.7 | |
| Total | 60 | 100 | |
| Character of pain | Dull aching | 33 | 55 |
| Colicky | 23 | 38.3 | |
| Stabbing | 4 | 6.7 | |
| Total | 60 | 100 |
Pulse rate and blood pressure were normal in 48 (80%) and 44 (73.3%), pallor reported in 2 (3.3%) of the patients, and none of the patients were presented with jaundice. Abdominal examination revealed signs of peritonitis in 16 (26.7%), generalized 14 (23.3%), abdominal distention 6 (10%). Localized pain in Rt hypochondrial 22 (36.7%), RIF 15 (25%),epigas tric 2 (3.3%) and lower abdomen 2 (3.3%) (Table 4). Abdomen US, X-ray and abdomen CT(Computed Tomography) were done for 53 (88.3%), 17 (28.3%) and 5 (8.3%) of the patients respectively (Table 5). The common three clinical diagnosis were acute cholecystitis 18 (30%), acute appendicitis 13 (21.7%) and uncertain diagnosis 11(18.3%) (Table 6).
| Yes | No | Total | ||||
|---|---|---|---|---|---|---|
| Symptoms (n=60) | N | % | N | % | N | % |
| Nausea | 56 | 93.3 | 4 | 6.7 | 60 | 100 |
| Vomiting | 59 | 98.3 | 1 | 1.7 | 60 | 100 |
| Fever | 53 | 88.3 | 7 | 11.7 | 60 | 100 |
| Abdominal distension | 7 | 11.7 | 53 | 88.3 | 60 | 100 |
| Abdominal distention | N | % | |
| Yes | 6 | 10 | |
| No | 54 | 90 | |
| Total | 60 | 100 | |
| Generalized peritonitis | Yes | 14 | 23.3 |
| No | 46 | 76.7 | |
| Total | 60 | 100 | |
| Bowel sound | No | 1 | 1.7 |
| Yes | 59 | 98.3 | |
| Total | 60 | 100 | |
| Localized peritonitis | No | 18 | 30 |
| Rt hypo colon | 22 | 36.7 | |
| Lower abdomen | 2 | 3.3 | |
| Epigastric left | 2 | 3.3 | |
| RTF | 15 | 25 | |
| Umbilical | 1 | 1.7 | |
| Total | 60 | 100 |
The most common operative findings were inflammation of the appendix 14 (23.3%) and gallbladder 14 (23.3%) in addition to other findings reported in Table 7. The laparoscopic findings and clinical diagnosis correlation showed that the two procedures were identical in 32 (53.3%) of the cases and different in 28 (46.7%). Indicates laparoscopy is diagnostic in 28 cases out of the total 60 cases under the study. P value= 0.017<0.05 indicates significant. Therapeutic success was reported in 51 (85%) of the patients, in most of the patients 18 (30%) lap chole was done. Need for conversion (n=9) was due to adhesion 4 (44.4%), biliary leak 1 (11.1%), not clear anatomy 3 (33.3%) and bowel stuck together in 1 (11.1%). Other operations needed (n=9) were open chole 5 (55.6%), laparotomy 2 (22.2%) and open appendectomy 2 (22.2%) (Table 8).
| Done | Not done | Total | ||||
|---|---|---|---|---|---|---|
| Imaging | N | % | N | % | N | % |
| X-ray | 17 | 28.3 | 43 | 71.7 | 60 | 100 |
| Abd USS | 53 | 88.3 | 7 | 11.7 | 60 | 100 |
| Abd CT | 5 | 8.3 | 55 | 91.7 | 60 | 100 |
| Clinical diagnosis | N | % |
|---|---|---|
| Acute appendicitis | 13 | 21.7 |
| Acute cholecystitis | 18 | 30 |
| Perforated viscous | 4 | 6.7 |
| Uncertain diagnosis | 11 | 18.3 |
| Biliary leak | 1 | 1.7 |
| Acute cholecystitis+Mucocele | 1 | 1.7 |
| Empyema gallbladder | 2 | 3.3 |
| Appendix mass | 2 | 3.3 |
| Adhesive obstruction | 2 | 3.3 |
| Mucocele of the gallbladder | 2 | 3.3 |
| Diverticulitis | 1 | 1.7 |
| Foreign body (trauma) | 1 | 1.7 |
| Ruptured ovarian cyst | 1 | 1.7 |
| Complicated appendix | 1 | 1.7 |
| Total | 60 | 100 |
| Operative findings | N | % |
|---|---|---|
| Inflamed appendix | 14 | 23.3 |
| Mucocele of appendix | 1 | 1.7 |
| Sub hepatic appendix | 2 | 3.3 |
| Inflamed gall bladder | 14 | 23.3 |
| Distended gall bladder, with edema | 2 | 3.3 |
| Contracted gall bladder | 2 | 3.3 |
| Hemorrhagic ovarian cyst | 1 | 1.7 |
| PID, tubal abscess | 1 | 1.7 |
| Ruptured ovarian cyst | 2 | 3.3 |
| Adhesive intestinal obstruction | 3 | 5 |
| Foreign body | 1 | 1.7 |
| Bowel matted together | 1 | 1.7 |
| inflamed appendix with band adhesion | 1 | 1.7 |
| Ectopic pregnancy | 1 | 1.7 |
| Mucocele gall bladder | 2 | 3.3 |
| Empyema gall bladder | 4 | 6.7 |
| Biliary peritonitis | 1 | 1.7 |
| Torsion ovarian cyst | 1 | 1.7 |
| appendicular mass | 2 | 3.3 |
| Perforated DU | 1 | 1.7 |
| Sealed perforated DU | 3 | 5 |
| Total | 60 | 100 |
| Therapeutic success | N | % | |
|---|---|---|---|
| Yes | 51 | 85 | |
| No | 9 | 15 | |
| Total | 60 | 100 | |
| Type of Lap procedures done | Lap adheisolysis | 3 | 5 |
| Lap chole | 18 | 30 | |
| lap cholecystostomy tube | 1 | ||
| Lap salpingectomy | 1 | 1.7 | |
| Lap graham patch | 1 | 1.7 | |
| Lap wash and drain | 3 | 5 | |
| Lap foreign body removal | 1 | 1.7 | |
| Lap cyst excision | 1 | 1.7 | |
| Lap appendectomy | 22 | 1.7 | |
| Total | 60 | 100 | |
| Need for conversion open | No | 51 | 85 |
| Yes | 9 | 15 | |
| Total | 60 | 100 | |
| Causes of conversion | Dilated bowel, source of leak unknown | 1 | 11.1 |
| Adhesion | 4 | 44.4 | |
| The bowel was matted together | 1 | 11.1 | |
| Anatomy not clear | 3 | 33.3 | |
| Total | 9 | 100 | |
| Need other operation | No | 51 | 90 |
| Yes | 9 | ||
| Total | 60 | 100 | |
| Operations | Laparotomy | 2 | 22.2 |
| Open chole | 5 | 55.6 | |
| Open appendectomy | 2 | 22.2 | |
| Total | 9 | 100 |
Laparotomy was avoided in 10 cases (16.6%), three (30%) of them were laparoscopic adhesiolysis, four (40%) cases of perforated duodenal ulcer, three out of them were found sealed, and an omental patch was done in one condition. A case of foreign body(pin) removal after trauma with a pin gun, Another case of ectopic pregnancy, and a case of cholecystostomy tube. Diagnosis was confirmed in 11 (18.3%) of cases which were put in the category of uncertain diagnosis preoperatively.
The duration of surgery was less than 2 hours in 38 (63.3%), and 2-3 hours in 22 (36.7%). Only one patient develops intraoperative bleeding. Most of the patients 47 (78.3%) started oral feeding in less than 24 hours, 10 (16.7%) 24-48 hours and 3 (5%) more than 48 hours. Most of the patients 48 (80%) were discharged after 48 hours. The reported post operative complications were port site infection 4 (6.7%), wound infection 3 (5%), incisional hernia 1 (1.7%) (Figure 2).
Discussion
In this multicenter study, 60 patients were enrolled to identify the diagnostic and therapeutic value of laparoscopy in the management of acute abdomen in a private hospital in Khartoum state. Demographic data of the patients showed that the common age group was 15-30 years in 24 (40%). The mean age was 29 ± 2.3 years in conscience with another study conducted in the same area evaluating the safety of elective laparoscopic cholecystectomy in a cohort of Sudanese patients [6].
Considering clinical variables, the study showed that the common three clinical diagnoses were acute cholecystitis 18 (30%), acute appendicitis 13 (21.7%), and uncertain diagnosis 11 (18.3%). Ahmad et al., in Saudi patient reported that 25 (28.4%) patients presented with Non-Specific Abdominal Pain (NSAP) in the lower abdomen [7]. Another study by Al Qahtani et al., in Saudi Arabia showed that 99 (78.4%) patients. Patients who were presented with unexplained/ nonspecific abdominal pain in the lower part of the abdomen accounted for 29% (n=37) [8].
The laparoscopic findings and clinical diagnosis correlation showed that the two procedures were identical in 32 (53.3%) of the cases and different in 28 (46.7%), which indicates that laparoscopy is diagnostic in 28 cases out of the total 60 cases under the study. P value=0.017<0.05 indicates significant findings, like the study conducted by Babannavar et al., and the conclusion was Laparoscopy diagnostic in 50 patients (100%). Laparoscopy could accomplish treatment in 47 patients (94%). Unnecessary and non-therapeutic laparotomies were avoided in 7 patients (14%) [9]. Ankur in India found that 76 (34%) patients suffered from gynecological pathology, followed by inflammation of the appendix in 62 (28%) [10]. A definitive clinical diagnosis of appendicitis is exempted from the study. Seven patients showed negative laparoscopy and five patients are needed to convert to open procedure [10].
Faisal and Muhammad in Pakistan assessed the diagnostic and therapeutic utility of laparoscopic surgery in unexplained acute abdominal conditions. Accurate diagnosis was established successfully in all patients. The outcome of diagnostic laparoscopy was uncomplicated acute appendicitis in 31 (58.49%) patients, complicated acute appendicitis in 5 (9.43%) patients, acute cholecystitis in 1 (1.88%) patient, pancreatic necrosis in 1 (1.88%) patient, mesenteric adenitis in 2 (3.77%) patients, caecal mass in 2 (3.77%) patients, dual pathologies in 5 (9.43%) patients, and gynaecological emergencies in 6 (11.32%) patients [11]. Zarin et al., studied the role of laparoscopy in patients presented with acute abdomen to find the extent of its diagnostic and therapeutic role in Pakistan [12]. Out of their total sample, Laparoscopy was successful in diagnosing all cases. After diagnosis 212 (88.3%) patients were managed primarily by laparoscopy at the same procedure while 28 (11.7%) patients were subjected to an open procedure [12].
Conversion to open surgery occurs in nine cases, with intraoperative bleeding reported in a single case. The reported post operative complications were port site infection 4 (6.7%), wound infection 3 (5%), incisional hernia 1(1.7%). The same conclusions approached by Elsamani et al., in Khartoum reported that the conversion rate into open surgery was reported at 10% (7/70) [6]. However, it’s (15%) higher than Ankur who reported five patients were converted to an open procedure [10]and Alsammani et al., reported conversion rate from laparoscopic to open surgery was 1.35% (4 patients) [13].
Good clinical outcome was the general feature of laparoscopy in this study. The duration of surgery was less than 2 hours in 38 (63.3%), and 2-3 hours in 22 (36.7%). Most of the patients 47 (78.3%) started oral feeding after less than 24 hours and most of them 48 (80%) discharged after 1-2 days again like the study conducted by Elsamani et al., which concluded that the mean time for surgery was 90.7 ± 32 minutes. Another study by Abbas et al., in Egypt showed similar statistically significant results in terms of shorter hospital stays, and readmission rate, with a lower morbidity rate recorded [6,14].
Conclusion
Emergency laparoscopy can be used for the diagnosis and/or management of a wide variety of acute abdomen. Laparoscopy decreases overall hospital stay and avoids increased complications, conversion to open procedure, and mortality.
What is already known on this topic?
• Use of laparoscopy is safe and effective in acute abdomen conditions worldwide.
• No published research about the role of laparoscopy in diagnosis and managing acute abdominal conditions.
What does this study add?
• Laparoscopy is Safe in diagnosis and managing acute abdominal conditions.
• Laparoscopy is associated with minimum intraoperative complication and early post-operative oral intake.
• Laparoscopy is associated with less hospital stay, less postoperative complication, and early return to activity.
Competing Interests
None
Authors’ Contributions
AMAE, MEH conceived the idea of the study. AMAE, YAA, and MEH contributed equally to data collection and data analysis. AMAE, YAA, and MEH contributed to the manuscript writing and review of the manuscript. All authors approved the manuscript.
Acknowledgments
None
References
- Sözüer EM, Bedirli A, Ulusal M, Kayhan E, Yilmaz Z. Laparoscopy for diagnosis and treatment of acute abdominal pain. J Laparoendosc Adv Surg Tech A 2000;10(4): 203-207.
[Crossref] [Google Scholar] [Pubmed]
- Agresta F, Ansaloni L, Baiocchi GL, Bergamini C, Campanile FC, Carlucci M, et al. Laparoscopic approach to acute abdomen from the Consensus Development Conference of the Società Italiana di Chirurgia Endoscopica e nuove tecnologie (SICE), Associazione Chirurghi Ospedalieri Italiani (ACOI), Società Italiana di Chirurgia (SIC), Società Italiana di Chirurgia d’Urgenza e del Trauma (SICUT), Società Italiana di Chirurgia nell’Ospedalità Privata (SICOP), and the European Association for Endoscopic Surgery (EAES). Surg Endosc 2012;26: 2134-2164.
[Crossref] [Google Scholar] [Pubmed]
- Golash V, Willson PD. Early laparoscopy as a routine procedure in the management of acute abdominal pain: A review of 1,320 patients. Surg Endosc 2005;19: 882-885.
[Crossref] [Google Scholar] [Pubmed]
- Chung RS, Diaz JJ, Chari V. Efficacy of routine laparoscopy for the acute abdomen. Surg Endos 1998;12: 219-222.
[Crossref] [Google Scholar] [Pubmed]
- Musa AM, Adam MA, Hamza AA. Audit of laparoscopic cholecystectomy Omdurman teaching hospital. Sudan J Med Sci 2008;3(1): 21-24.
- Elsamani E, Elrahim WE, Khalil EA, Saad EA, Awadelkarim AM, Elsiddig KE, et al. Early laparoscopic cholecystectomy for acute cholecystitis in a cohort of Sudanese patients: Outcome and complications in minimum resource-settings. J Surg 2017;6(3): 555-694.
- Ahmad MM, Dar HM, Waseem M, Nazir I, Jeelani A. Role of laparoscopy in nonspecific abdominal pain. Saudi Surg J 2014 ;2(3): 71-74.
- Al Qahtani FA, Al Selaimy HM, and Al Muqrin SM. Laparoscopy role in diagnosis and management of unexplained/nonspecific abdominal pain. Int J Adv Res 2017; 5(1): 205-209.
[Crossref]
- Babannavar PB, Thejeswi P, Rao SP, Aravindan R, HS SR. Role of laparoscopy in diagnosis and management of acute Abdomen-in South Indian population. The Internet J Surg 2013;30(4).
- Ankur J. Evaluation of the role of diagnostic laparoscopy innon specific abdominal pain and its correlation with clinical and radiographic findings IOSR-JDMS 2018; 17(9): 9-44.
- Faisal MS, Muhammad SD. Utility and outcome of diagnostic laparoscopy in unexplained acute abdominal conditions. J Sheikh Zayed Med College (JSZMC) 2016;7(2): 960-964.
- Zarin M, Zeb J, Khan MA, Maroof SA, Ibrar S. Acute abdomen: Role of laparoscopy in acute abdomen. The Prof Med J 2019;26(03): 438-442.
- Alsammani MB, Alhaj MA, Alawad AA. Preliminary experience with laparoscopic surgery in sudanese low-resourced teaching hospital. Med J 2015;2(6): 94-99.
- Abbas A, Borham W, El Ghadban H, Abdelatif M, Samir M, Dawoud I, et al. Early laparoscopy in the management of acute non specific abdominal pain: Is it mandatory. Ann Emerg Surg 2017;2(5): 1023.