Case Report - Archives of Clinical and Experimental Surgery (2022)
Laparoscopic Cholecystectomy in a Patient with Lumbar Peritoneal Shunt (LP Shunt): A Case Report
Musharraf Husain, Tajamul Rashid*, Sanjana Agarwal, Sonali Ohri and Nikhat SartajTajamul Rashid, Department of General Surgery, Hamdard Institute of Medical Sciences and Research, New Delhi, India, Email: doc.tajamul@gmail.com
Received: 05-Apr-2022, Manuscript No. EJMACES-22-62389; Editor assigned: 08-Apr-2022, Pre QC No. EJMACES-22-62389 (PQ); Reviewed: 22-Apr-2022, QC No. EJMACES-22-62389; Revised: 27-Apr-2022, Manuscript No. EJMACES-22-62389 (R); Published: 05-May-2022
Abstract
Background: Benign Intracranial Hypertension is a condition causing symptomatic raised intracranial pressure and many such patients are managed by ventriculoperitoneal or lumbar peritoneal shunts. Performing laparoscopic procedures in patients with ventriculoperitoneal or lumbar peritoneal shunt was considered to be risky and was avoided. There are very few documented cases worldwide in which laparoscopic cholecystectomy has been carried out in patients with a lumbar peritoneal shunt.
Case report: A 39 years old female patient presented to the surgery department of the HAH Centenary Hospital, New Delhi with complaints of pain in the right upper abdomen on and off for one year. Consequently, on evaluation she was diagnosed as a case of symptomatic cholelithiasis and was planned for elective laparoscopic cholecystectomy. She was previously diagnosed with Benign Intracranial hypertension and was managed by lumbar peritoneal shunt at the level of L4-L5. A 4 Port standard laparoscopic cholecystectomy was done taking care of not damaging the shunt. Intraoperative and postoperative courses were uneventful.
Conclusion: Based on our experience, we suggest that laparoscopic procedures like cholecystectomy can be safely and successfully performed in patients with Lumbar Peritoneal shunt after getting neurosurgery clearance. No clamping of shunt or alteration of technique is required during the procedure.
Keywords
Benign intracranial hypertension; Laparoscopic cholecystectomy; Lumbar peritoneal shunt
Introduction
Benign Intracranial Hypertension or pseudotumor cerebri is a condition causing symptomatic raised intracranial pressure. Most patients can be managed conservatively but ventriculoperitoneal or lumbar peritoneal shunting may be required in patients with visual field loss.
Earlier, performing laparoscopic procedures in patients with ventriculoperitoneal or lumbar peritoneal shunt was considered to be risky and was preferably avoided. As per the literature, creating pneumoperitoneum would increase the intra-abdominal pressure which could further increase the intracranial pressure even causing hindbrain herniation in few cases [1]. There are very few documented cases worldwide in which successful laparoscopic cholecystectomy has been carried out in patients with a lumbar peritoneal shunt. To our knowledge, ours is the only documented case in India of a laparoscopic cholecystectomy in a patient with lumbar peritoneal shunt.
Case Report
A 39 years old female patient presented to the surgery department of the HAH Centenary Hospital, New Delhi with complaints of pain in the right upper abdomen on and off for one year. She was previously diagnosed with Benign Intracranial hypertension in November 2020 when she had presented to the Neurosurgery OPD with complaints of headache and blurring of vision for 2 months, progressing to complete loss of vision. Decision was taken to insert a Lumbar Peritoneal shunt at the L4-L5 level in this patient on 7th November 2020. The procedure was uneventful without any neurological complications. Patient had no other known comorbidities and had undergone a lower segment caesarean section nine years ago.
In August 2021, the patient presented to the surgery OPD with an ultrasound whole abdomen report showing multiple calculi in the gall bladder lumen, maximum size being 16.3 mm with CBD normal in size, suggestive of cholelithiasis. Patient was counselled to undergo laparoscopic cholecystectomy and relevant preoperative workup was done. Her baseline investigations were unremarkable and neurosurgery clearance was taken prior to surgery.
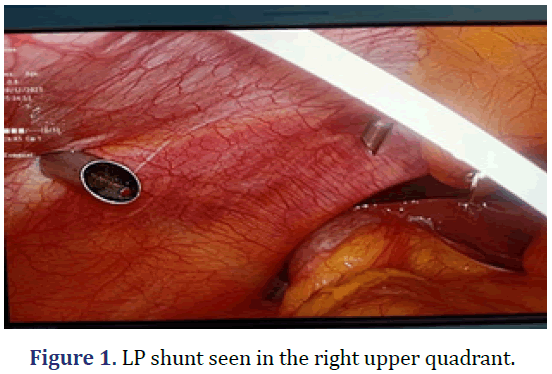
Informed consent for surgery was taken from the patient and the chances for conversion to open procedure were explained to the patient in her local language. On the day of surgery, prophylactic antibiotic Ceftriaxone 1 gm was given intravenously within 60 minutes of the surgical incision. Under aseptic precautions, pneumoperitoneum was created via Supraumbilical port and a routine laparoscopic cholecystectomy was performed using the standard four ports (made under direct vision) by an experienced faculty member taking care of avoiding the port insertion within or close to the site of lumbar peritoneal shunt. The shunt catheter was seen in the right upper side of abdomen with minimal adhesions seen at the point of entry which were left untouched (Figure 1). The insufflation pressure was maintained at 10 mm Hg for the entire duration of surgery. Intraoperatively, dense omental adhesions were present around Calot’s triangle and the gall bladder was thick walled containing multiple calculi in the lumen. CBD and liver were grossly normal. Extreme care was taken to avoid intraoperative perforation of gallbladder and thereby spillage of contents in the peritoneal cavity that could potentially infect the LP shunt. The specimen was carefully delivered via epigastric port. The total duration of the procedure was 50 minutes with minimal blood loss. No drain was placed in the abdominal cavity.
Postoperative period was uneventful and the patient was neurologically stable. Two doses of Ceftriaxone 1 gm were given intravenously in the immediate postoperative period and was discharged on the second postoperative day. Histopathology report confirmed the features of chronic cholecystitis.
Discussion
Benign Intracranial Hypertension or pseudotumor cerebri is a condition causing symptomatic raised intracranial pressure without ventricular enlargement. The patient, most commonly is a young, overweight woman presenting with complaints of headache and visual deterioration. Most cases are self-limiting. Conservative management includes lifestyle changes and medications like acetazolamide to decrease the CSF production. Ventriculoperitoneal or lumbar peritoneal shunting may be required in patients with visual field loss [2].
Lumbar Peritoneal shunt is used for diversion of CSF fluid from the lumbar thecal sac into the peritoneal cavity. It can be safely and effectively used in many conditions like communicating hydrocephalus, benign intracranial hypertension, growing skull fractures, increased intracranial pressure due to chronic meningitis, syringomyelia etc. Being a completely extracranial procedure, it is considered to have a considerable advantage over a ventriculoperitoneal shunt with fewer complications like infection and malfunction [3]. As per the study by K. Abubaker et al., LP shunts provided a slightly higher immediate postoperative symptoms relief as compared to VP shunts with a lower failure rate (11% vs. 14%). But LP shunts were noted to have a higher revision rates and other shunt-related complications [4].
Schwed et al. described a case of massive subcutaneous emphysema in a patient with recent ventriculoperitoneal catheters after undergoing routine laparoscopic cholecystectomy. The total lung compliance can reduce up to 20% in patients without any known pulmonary disease during any uncomplicated laparoscopic procedure. It was suggested by this study to delay the elective laparoscopic surgeries till the tract is fibrosed and sealed, although there was no mention of the exact timing to conduct the procedure [5].
In 1998, Baskin et al. reported the first case of ventriculoperitoneal shunt failure in a patient having shunt-dependent hydrocephalus who underwent a feeding jejunostomy laparoscopically. It was believed that shunt blockage was due to impacted soft tissue or due to an air lock produced in the distal shunt tubing during intraperitoneal insufflation. To prevent shunt related complications, externalization of the distal shunt catheter was advised for the entire duration of surgery. This maneuver would ensure continuous CSF drainage during the procedure and reduce the risk of retrograde insufflation as recommended by the authors [6].
Jackman et al. analysed 18 patients with ventriculoperitoneal shunt who underwent various laparoscopic procedures, for signs of raised intracranial pressure both intraoperatively and postoperatively. No patient required invasive intracranial monitoring and there were no reported cases of bradycardia, hypertension or hypercapnia during the course of any laparoscopic procedure [7].
Possible risks in patients with LP shunt who undergo laparoscopic cholecystectomy are shunt blockage, infection, subcutaneous emphysema, puncture of the catheter and conversion to open. Now a days, with the advent of modern shunt systems with no reflow-valves, chances of retrograde insufflation by CO2 during laparoscopy has decreased considerably. Pressures up to 350 mm Hg can be easily tolerated with no retrograde flow and with no increase in the intracranial pressure [8,9].
Kerwat et al. reported the first successful laparoscopic cholecystectomy in a patient with Lumboperitoneal shunt. During the procedure, an endoclip was used to clamp the LP shunt which was removed at the end of the surgery and the use of nitrous oxide was excluded by the anaesthesia team to avoid the chances of development of iatrogenic tension pneumoencephalus [10]. Three more studies reported cases of successful laparoscopic cholecystectomy in patients with LP shunt but CSF shunts were clamped in almost all cases [8, 9, 11]. In the study by Yoshihara et al. only in one case (out of four) and in the case described by Rumba et al. were the shunts left unclamped [8,9].
To the best of our knowledge, this is the first reported case in India of a laparoscopic cholecystectomy done in a patient with Lumbar Peritoneal shunt. Intraoperatively, no alterations were made in the port placement nor were clamping of the shunt done. There was no postoperative neurological deficit and no shunt related complications were documented.
Conclusion
As per our knowledge and after through search of the published literature, this probably is the first reported case in India of laparoscopic cholecystectomy done in a patient with Lumbar Peritoneal shunt. Based on our experience, we suggest that laparoscopic procedures like cholecystectomy can be safely performed in patients with Lumbar Peritoneal shunt after getting neurosurgery clearance. No clamping of shunt or alteration of technique is required during the procedure.
Conflict of Interest
None
Ethical Clearance
Not applicable
Consent of the patient
Applicable and taken
Funding
None
References
- Cobianchi L, Dominioni T, Filisetti C, Zonta S, Maestri M, Dionigi P, et al. Ventriculoperitoneal shunt and the need to remove a gallbladder: Time to definitely overcome the feeling that laparoscopic surgery is contraindicated. Ann Med Surg (Lond) 2014;3(3):65-7.
[Crossref] [Google Scholar] [Pubmed]
- Weisberg LA. Benign intracranial hypertension. Medicine 1975; 54(3):197-207.
- Yadav YR, Parihar V, Sinha M. Lumbar peritoneal shunt. Neurol India 2010;58(2):179.
[Crossref] [Google Scholar] [Pubmed]
- Abubaker K, Ali Z, Raza K, Bolger C, Rawluk D, O'Brien D, et al. Idiopathic intracranial hypertension: lumboperitoneal shunts versus ventriculoperitoneal shunts–case series and literature review. Br J Neurosurg 2011;25(1):94-9.
[Crossref] [Google Scholar] [Pubmed]
- Schwed DA, Edoga JK, McDonnel TE. Ventilatory impairment during laparoscopic cholecystectomy in a patient with a ventriculoperitoneal shunt. J Laparoendosc Surg 1992;2(1):57-9.
[Crossref] [Google Scholar] [Pubmed]
- Baskin JJ, Vishteh AG, Wesche DE, Rekate HL, Carrion CA. Ventriculoperitoneal shunt failure as a complication of laparoscopic surgery. JSLS 1998;2(2):177.
[Google Scholar] [Pubmed]
- Jackman SV, Weingart JD, Kinsman SL, Docimo SG. Laparoscopic surgery in patients with ventriculoperitoneal shunts: safety and monitoring. J Urol 2000;164(4):1352-4.
[Crossref] [Google Scholar] [Pubmed]
- Yoshihara T, Tomimaru Y, Noguchi K, Nagase H, Hamabe A, Hirota M, et al. Feasibility of laparoscopic cholecystectomy in patients with cerebrospinal fluid shunt. Asian J Endosc Surg 2017;10(4):394-8.
[Crossref] [Google Scholar] [Pubmed]
- Rumba R, Vanags A, Strumfa I, Pupkevics A, Pavars M. Laparoscopic cholecystectomy for a patient with a lumboperitoneal shunt: A rare case. Chirurgia 2016;111(3):263-5.
[Google Scholar] [Pubmed]
- Kerwat RM, Murali Krishnan VP, Appadurai IR, Rees BI. Laparoscopic cholecystectomy in the presence of a lumboperitoneal shunt. J Laparoendosc Adv Surg Tech A 2001;11(1):37-9.
[Crossref] [Google Scholar] [Pubmed]
- Charalabopoulos A, Botha AJ. Laparoscopic cholecystectomy in the presence of lumboperitoneal shunt. Case Rep Surg 2013; 2013:1-3.
[Crossref] [Google Scholar] [Pubmed]
Copyright: © 2022 The Authors. This is an open access article under the terms of the Creative Commons Attribution NonCommercial ShareAlike 4.0 (https://creativecommons.org/licenses/by-nc-sa/4.0/). This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.