Case Series - Archives of Clinical and Experimental Surgery (2022)
Laparoscopic Management of Complex Hydatid Cysts: A Case Series from a Developing Country
Hina Gupta1*, Ranjeet Ahirwar1 and Ram Mohan Shukla22Department of Pediatric Surgery, M.G.M. Medical College and M.Y. Hospital, Madhya Pradesh, India
Hina Gupta, Department of General Surgery, M.G.M. Medical College and M.Y. Hospital, Madhya Pradesh, India, Tel: +918379949489, Email: guptahina1996@gmail.com
Received: 15-Nov-2022, Manuscript No. EJMACES-22-79910; Editor assigned: 18-Nov-2022, Pre QC No. EJMACES-22-79910 (PQ); Reviewed: 05-Dec-2022, QC No. EJMACES-22-79910; Revised: 12-Dec-2022, Manuscript No. EJMACES-22-79910 (R); Published: 20-Dec-2022
Abstract
Hydatid cyst, also known by the name, Cystic Echinococcosis is a zoonotic disease caused by echinococcus species, by the larval stage of Echinococcus Granulosus and Echinococcus Multilocularis, a tape worm affecting dogs, sheep, cattle (definitive host) and human (incidental host). Most of the human infections are asymptomatic as the infection involves a slowly growing cyst in visceral organs, commonly involving liver and lungs. The aim of the study is to access presentation patterns, characteristics, radiological investigations and laparoscopic management of complex hydatid cysts affecting liver and spleen. We present a case series of five such complex hepatic and splenic hydatid cysts over a duration of one year in our institute. Majority of the patients were females who presented with long history of pain in abdomen, vomiting, had contact with cattle, underwent radiological investigations and were operated by laparoscopic approach with uneventful post-operative course and minimal complications.
Keywords
Hydatid cyst; Echinococcosis; Definitive host; Incidental host; Laparoscopic managementbronchiole
Introduction
Human echinococcosis, the term given for the zoonotic disease transmitted by dogs and cattle (definitive host) in a livestock raising areas accidentally affecting the humans by the Echinococcus species of Cestode parasite (tape worm) [1]. The species of echinococcus affecting humans are Echinococcus granulosus, Echinococcus multilocularis. This disease has incidence of 1 to 200 cases per 100000 population with a greater number of cases observed in Andhra Pradesh and Tamil Nadu. It is found in livestock raising areas with poor hygiene [2]. The common organs involved by the disease are liver, lungs and less frequently spleen, kidney, heart, bones, and others. Majority of the patients affected by the disease are asymptomatic. Echinococcosis can be treated by various modalities, like, medical management, PAIR, surgery, but surgery remains the gold standard among various evolving new procedures. [3] In today’s world, laparoscopic approach is preferred approach which was used in all of our patients.
Case Presentation
The present study was carried over a duration of one year from September 2021 to October 2022 in which five cases of Echinococcus were studied. All the cases were subjected to detailed history and physical examination, Ultrasound (USG) and Computed Tomography (CT) Scan. Patients were operated laparoscopically after a preoperative course of albendazole for 28 days.
Case 1
A 23 years old female presented with pain in abdomen for 4-5 years in left hypochondrium, insidious in onset, gradually progressive in intensity, radiating to whole abdomen which aggravated in last 10 days. History of contact with cattle (buffalo) present.
On examination (O/E): Per abdomen (P/A)-soft, non-tender, bowel sounds present, no guarding or rigidity was present.
Ultrasound (USG) abdomen: showed 10 × 9 cm and 10 × 7 cm lesion in right lobe of liver containing fluid with echoes.
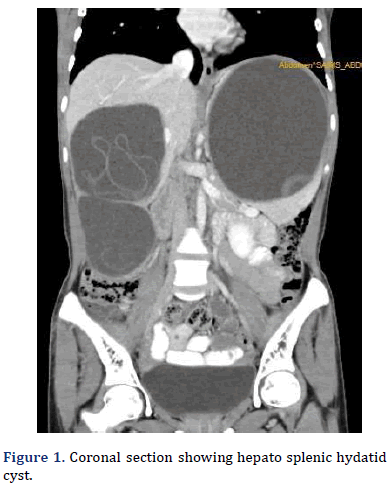
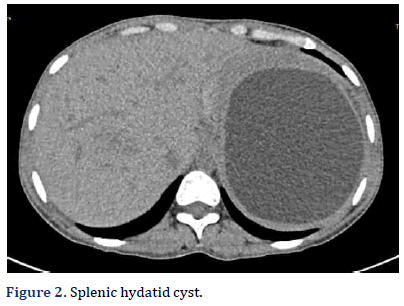
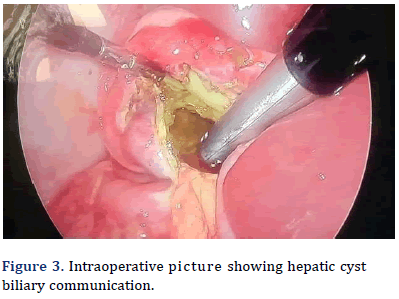
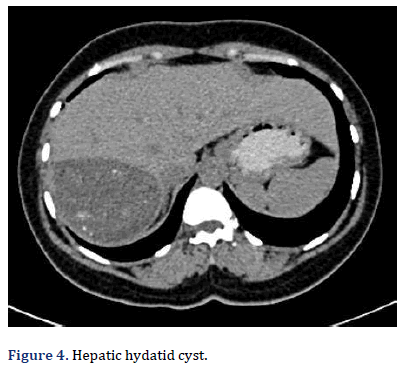
Contrast Enhanced Computed Tomography (CECT) abdomen (W/A): Two matted thick walled hypodense cystic lesions were seen in right lobe of liver, measuring approx. 11.6 cm × 9.6 cm × 10.3 cm containing 570 cc fluid and 9 cm × 7.7 cm × 6.7 cm cyst cavity containing 230 cc of fluid. Multiple curvilinear hyperdense thin mem- brane giving rise to water lily sign. Post contrast no internal enhancement was suggestive of hydatid cyst (type 2). In Figure 1 Cystic lesion is seen in the upper pole of splenic parenchyma, which measures approx. 14 cm × 14 cm × 11.6 cm containing around 1140 cc. Patient was operated with laparoscopic hepatic par- tial pericystectomy with abdominal drain placement in cystic cavity and laparoscopic marsupialization of splenic cyst with omentopexy (Figures 2-4 and Table 1). Patient was discharged on Post-Operative Day (POD) 6 with drain in situ (Figure 4 and Table 1).
| POD | QUANTITY (in ml) | TYPE |
|---|---|---|
| POD 0 | 280 | Bilious |
| POD 1 | 250 | Bilious |
| POD 2 | 180 | Bilious |
| POD 3 | 140 | Bilious |
| POD 4 | 100 | Bilious |
| POD 5 | 80 | Bilious |
Case 2
A 35 years female presented with pain in epigastrium for 1 year which was initially at epigastric region radiating to left hypochondrium, which was insidious in onset, gradual in progression and associated with post prandial fullness, vomiting and retro-sternal burn.
O/E: Per abdomen was soft, non-tender, bowel sounds present with no palpable organomegaly.
USG abdomen: showed 8 cm × 8 cm lesion with internal foci of calcification in right lobe of liver.
CECT W/A: revealed a lesion in right hepatic lobe involving the segment VI/VII of 7.2 cm × 8.6 cm × 6.9 cm abutting the inferior vena cava and right branch of the main portal vein. (type 1/CE1). Multiple small internal foci of calcifications were seen.
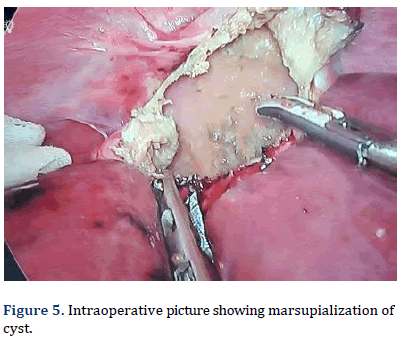
Laparoscopic marsupialization of hydatid cyst was done. as shown in Figure 5 and hydatid cyst fluid was sent for Routine and Microscopy examination. Post operatively patient was stable and doing well after 3 months of follow up (Figure 6).
Case 3
A 26 years female presented with pain in right hypochondrium for 2 months which was initially at right hypochondrium and then radiated to whole abdomen, was insidious in onset, gradual in progression and associated with on/off fever for 1 month.
O/E: Per Abdomen (P/A)- soft, non-tender, bowel sounds present with no palpable organomegaly.
USG abdomen: showed thick walled hypodense cystic lesion of 9 × 8 cm in right lobe of liver.
CECT W/A: revealed lesion seen in right he- patic lobe approx. 9.2 cm × 9.1 cm × 6.9 cm with thick wall and internal floating membrane with dense focal calcification reaching upto sub capsular space suggestive of right hepatic hydatid cyst. (TYPE2/CE3) Laparoscopic hydatid cyst marsupialization was done. Post operatively patient was stable on follow up visits.
Case 4
A 55 years female presented with pain over right hypochondrium for 2 years which increased progressively for 1 year. Pain was insidious in onset, gradually progressive. Patient had history of contact with dogs.
O/E: Per abdomen was soft, non-tender, bowel sounds present with liver palpable upto 12 cm below the costal margin.
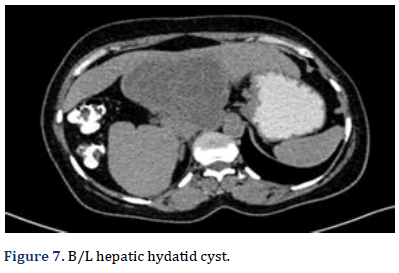
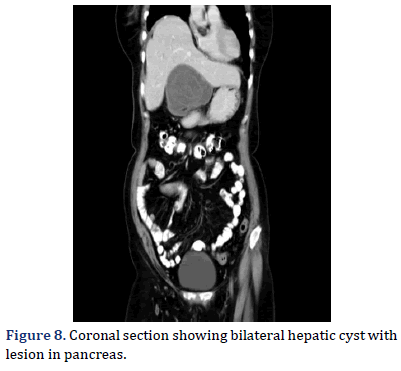
CECT W/A: revealed cystic lesion with float- ing internal membranes and no internal vascularity in segment II and III and hyperechoic lesion in segment VII of liver measuring 4 cm × 3 cm. Cystic lesion with wall calcification was is seen in segment VII and VIII of right lobe of liver and extending/ protruding in right subdiaphragmatic region. (Type 5/CE 5) and lesion with internal septations in inferior aspect of segment IVB (type 2/CE3).
Tiny cystic lesion of size 1.2 cm × 1.0 cm was seen in the body/tail region of the pancreas (Figures 7 and 8).
Patient was taken for laparoscopic hydatid cyst excision with omentopexy was done. At 3 months follow up, patient is doing well.
Case 5
A 42 years old female complained of pain and swelling in lateral aspect of left chest wall for 8 months.
Swelling was insidious in onset, gradually increasing in size with no pain. Patient had history of contact with cattle (goat). Also, she gave previous surgical history of exploratory laparotomy with marsupialization and omentoplasty done for Left Lobe liver hydatid cyst in 2011 elsewhere. On post-operative day 3 of marsupialization and omentopexy, she developed intestinal obstruction for which Re-exploration with adhesiolysis was done.
O/E: A bucket scar mark was seen in right subcostal re- gion and a midline incision scar mark present with no palpable organomegaly. A swelling of around 10 cm × 6 cm was present over lateral aspect of left chest wall extending from 5th to 7th intercostal space vertically and extending from anterior axillary line to posterior axillary line horizontally.
On palpation, swelling was non-tender with no local rise of temperature, soft in consistency, non-mobile, fluctuant and non-transilluminant.
USG abdomen: showed multiple well defined anechoic clustered cystic lesions in splenic parenchyma extending to left hypochondrium and left lumbar region. Few of them showed peripheral calcification suggestive of splenic hydatidosis leading to peritoneal hydatidosis.
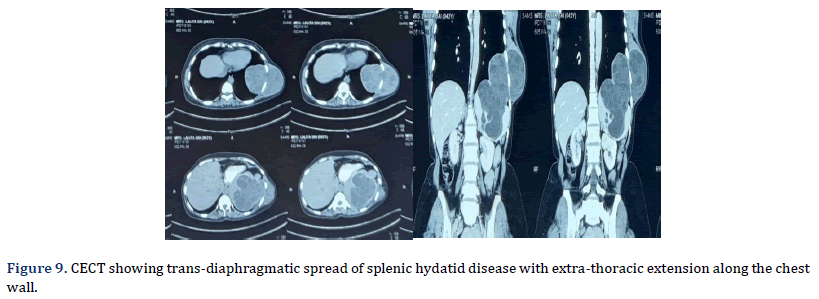
CECT whole abdomen revealed lobulated cystic lesion involving spleen, extending in left lower chest cavity and across the chest wall into the subcutaneous planes. The lesion shows multiple variable sized daughter cysts suggestive of di-aphragmatic/transdiaphragmatic spread of splenic hy-datid disease with extra-thoracic extension along the chest wall (TYPE3/CE2) (Figure 9).
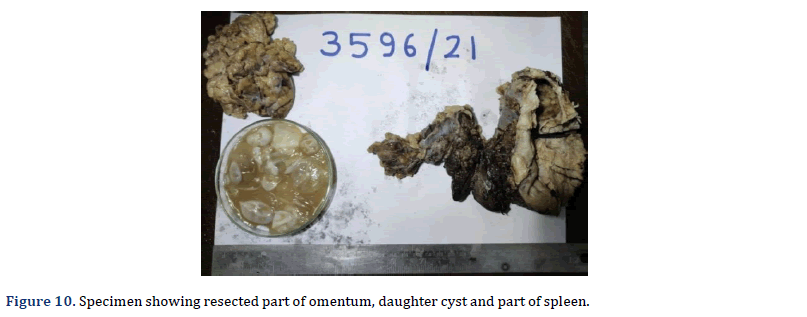
Patient was taken up for diagnostic laparoscopy in which excision of hepatic cyst with splenectomy was done (Figure 10).
Patient discharged in stable condition on tablet albendazole 400 mg twice a day to be continued for 3 months with a gap in between to prevent bone marrow suppression. Patient was doing well on follow up (Table 2).
| Case | Presentation | Cect | Procedure |
|---|---|---|---|
| 1. | pain in abdomen since 4-5 yrs with increase severity since 10 days | two lesions in right lobe of 570cc and 230 cc and lesion in upper pole of spleen of 1140cc | Laparoscopic marsupialization of splenic cyst and hepatic cyst with partial pericystectomy with omentopexy of splenic cyst with abdominal cyst |
| 2. | Pain in epigastrium and left hypochondrium | Type1 ce1 lesion in right hepatic lobe | Laparoscopic hydatid cyst marsupialization |
| 3. | Pain over right hypochondrium | Type 2 ce3 in right lobe of liver | Laparoscopic hydatid cyst marsupialization |
| 4. | Pain over right hypochondrium since 2 years | Type 5/CE5 lesion in right lobe of liver | Exploratory lap with hydatid cyst excision with omentopexy |
| 5. | Swelling in lateral aspect of left chest wall | Lobulated cystic lesion in spleen involving diaphragm extending upto lower thorax to subcutaneous diaphragmatic defect | Exploratory laparotomy with splenectomy along with excision of hydatid cyst with repair of diaphragmatic defect |
Results and Discussion
Hydatid cyst is usually an incidental finding; previously it was diagnosed with the Casoni Test but it is abandoned now due to low sensitivity. When incidentally collapsed cysts inside cyst wall are seen on ultrasound in a suspected case of hydatid disease, they can be confirmed with CT scan imaging [4,5].
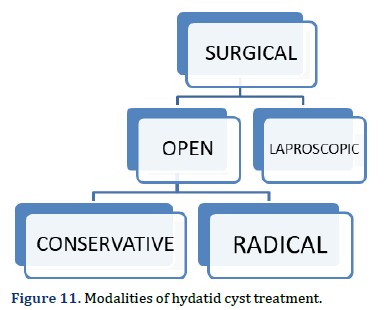
In our study, patient’s age group was ranging from 20-60 years; all five were females, showing female preponderance for the disease. Patients had chronic history of dull aching abdominal pain and a positive history of contact with cattle which lead to the differential diagnosis of hydatid cyst as a possibility. The clinical spectrum of hydatid cyst depends upon the organ involved. For further evaluation, radiological investigations (USG and CECT scan) were done. Laparoscopic approach for the management of these hydatid cysts was chosen. Marsupialization of the cysts was done with drain placement in most of the cases. Patients were given post-operative course of albendazole for 3 months with a gap of 2 weeks in between. (Figure 11).
Hydatid cyst disease can be managed medically with albendazole, carbamates, mebendazole and tapered according to the size of the cyst cavity. Out of all these drugs, albendazole is found to be more effective ow- ing to better penetration, absorption and being scoliocidal. There can be side effects due to drugs like, mild abdominal pain, vomiting, pruritis, leukopenia.
Echinococcosis can also be managed surgically if medical management is not effective or if the cyst is large and symptomatic. Open and laparoscopic surgical approaches are available for the treatment. Marsupialization, cystectomy, peri-cystectomy, lobectomy, hepatectomy can be done surgically to treat the disease. There are conditions in which surgery is avoided if;
• There are multiple cysts localised in several organs.
• Homogenously calcified cyst walls [6].
Through our short study, in a resource limited setup, we would like to share our results of laparoscopic surgery that we obtained in complex hepatic and splenic hydatid cysts. In majority of the patients, marsupialization was done with omentopexy and in some cases; splenectomy was done according to the presentation. None of the patients had spillage ,anaphylaxis, peritoneal spread or conversion to open surgery during our procedure or in follow ups. Baskaran V, et al., [7] had five intraoperative spillage, and Chowbey PK, et al., [8] had one trocar-induced bowel perforation whereas no such complications were observed in our cases. One of the patients who had peritoneal spread due to previous open surgery had no further complications during follow up. Post-operative course was uneventful with early mobilization, no wound complications, short hospital stay and no recurrence as compared to Sokouti M et.al and D S Samala. [9,10] Patients were followed up for a duration of 6 months.
Conclusion
Laparoscopic surgery is an emerging modality for the treatment of hydatid cyst in developing countries. It is a challenge to operate echinococcosis with such high infectivity and chances of spillage and allergic reactions. But, with less operative time, shorter hospital stays, early resumption of daily activities, low morbidity and successful results, laparoscopic management is becoming the preferred modality of treatment of echinococcosis even in developing countries.
References
- Williams NS, Bulstrode CJK, O'Connell PR. Baily and Love’s Short Practice of Surgery, 17th edn. Hodder Arnold; 1977:859-863.
- Reddy CR, Narasiah IL, Parvathi G, Rao MS. Epidemiology of hydatid disease in Kurnool. Indian J Med Res 1968;56(8):1205-20.
[Google Scholar] [Pubmed]
- El Malki HO, El Mejdoubi Y, Souadka A, Zakri B, Mohsine R, Ifrine L, et al. Does primary surgical management of liver hydatid cyst influence recurrence? T Gastrointest Surg 2010;14:1121-7.
- Lardière-Deguelte S, Ragot E, Amroun K, Piardi T, Dokmak S, Bruno O, et al. Hepatic abscess: Diagnosis and management. J Visc Surg 2015;152(4):231-43.
[Crossref] [Google Scholar] [Pubmed]
- Rasheed K, Zargar SA, Telwani AA. Hydatid cyst of spleen: A diagnostic challenge. N Am J Med Sci 2013;5(1):10–20.
[Crossref] [Google Scholar] [Pubmed]
- Malik AA, ul Bari S, Younis M, Wani KA, Rather AA. Primary splenic hydatidosis. Indian J Gastroenterol 2011;30(4):175–177.
[Crossref] [Google Scholar] [Pubmed]
- Baskaran V, Patnaik PK. Feasibility and safety of laparoscopic management of hydatid disease of the liver. JSLS 2004;8(4):359–363.
[Google Scholar] [Pubmed]
- Chowbey PK, Shah S, Khullar R, Sharma A, Soni V, Baijal M, et al. Minimal access surgery for hydatid cyst disease: Laparoscopic, thoracoscopic, and retroperitoneoscopic approach. J Laparoendosc Adv Surg Tech 2003;13(3):159–165. doi: 10.1089/109264203766207672.
- Sokouti M, Sadeghi R, Pashazadeh S, Abadi SEH, Sokouti M, Ghojazadeh M, et al. A systematic review and meta-analysis on the treatment of liver hydatid cyst using meta-MUMS tool: comparing PAIR and laparoscopic procedures. Arch Med Sci 2019;15(2):284-308.
[Crossref] [Google Scholar] [Pubmed]
- Samala DS, Gedam MC, Gajbhiye R. Laparoscopic Management of Hydatid Cyst of Liver with Palanivelu Hydatid System over a Period of 3 Years: A Case Series of 32 Patients. Indian J Surg 2015;77:918-22
[Crossref] [Google Scholar] [Pubmed]
Copyright: © 2022 The Authors. This is an open access article under the terms of the Creative Commons Attribution NonCommercial ShareAlike 4.0 (https://creativecommons.org/licenses/by-nc-sa/4.0/). This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.