Case Report - Archives of Clinical and Experimental Surgery (2024)
Migration of an Intrauterine Device into the Mediastinum
Qyun Zhehau and Diclyn Zichire*Diclyn Zichire, Department of Surgery, Yuncheng University, Shanxi, China, Email: Zdiclyn56@gamil.com
Received: 14-Jun-2024, Manuscript No. EJMACES-24-138955; Editor assigned: 17-Jun-2024, Pre QC No. EJMACES-24-138955 (PQ); Reviewed: 01-Jul-2024, QC No. EJMACES-24-138955; Revised: 08-Jul-2024, Manuscript No. EJMACES-24-138955 (R); Published: 15-Jul-2024
Abstract
We present the case of an otherwise healthy 23-year-old woman whose hormonal Intra Uterine Device (IUD) migrated from her uterus into her abdomen and then her mediastinum through a previously undiagnosed, asymptomatic paraesophageal hernia over a ten-month period. This is the first reported case of a translocated IUD found above the diaphragm.
Keywords
IUD migration; Hiatal hernia; IUD complication
Introduction
Intra Uterine Devices (IUDs) are among the most commonly used contraceptives in the world. They are long-acting, easily placed and reversed, and have a low rate of failure and other complications [1]. Two forms of IUD are approved by the United States Food and Drug Administration. Hormonal varieties (Kyleena, Mirena, Skyla, Liletta) release levonorgestrel, a progestin analog; the non- hormonal variety (ParaGard) releases copper ions. Contraceptive efficacy is achieved by local release of progestin or copper ions in the uterus, creating an unfavorable environment for fertilization. Hormonal IUDs are effective for three to five years depending on the brand, while the copper variety is reliable for ten years.
Most IUDs are placed by obstetrician-gynecologists, family physicians, or advanced practice professionals in the outpatient setting without sedation. IUDs are T-shaped, approximately 3 cm by 3 cm, with strings attached to the base of the device. They sit in the uterine cavity with the arms of the T oriented toward the oviducts, and are held in place by the resting tone of the myometrium [2].
IUD placement begins with direct visualization of the cervix by speculum exam. A metal or plastic uterine sound is inserted through the cervix to measure the depth of the uterus. A plastic sheath is then passed through the endocervical canal to the depth previously measured and the sterile IUD is delivered through it into the uterine cavity. The IUD strings pass through the external cervical or and remain visible by exam at the superior aspect of the vagina. When expired or when the patient no longer wishes to have an IUD, the IUD is removed from the uterus by pulling on the retrieval strings [3]. IUD placement is not routinely confirmed with imaging; however, pelvic or transvaginal ultrasound or abdominal radiography may be useful to confirm device position [4].
Complications of IUDs include infection, pain, menstrual irregularities, and migration of the device. The device may be expelled into the vagina, become embedded in the myometrium, or pass through the uterine wall into the abdominal cavity. Following passage through the uterine wall, the IUD is referred to as a translocated IUD. Risk factors for translocated IUD include postpartum amenorrhea, insertion by inexperienced practitioners, breastfeeding, and a retroflexed uterus [5]. This complication can occur during insertion if the uterus is sounded inaccurately or if the sound itself creates a false tract through the uterine wall through which the IUD is placed [5- 7]. IUD migration through the uterine wall has an incidence rate of 0.03%-0.2% [8]. IUD translocation itself is rarely a surgical emergency; it may be asymptomatic or may present with unintended pregnancy, menstrual abnormalities, or abdominal or pelvic pain. Bowel obstruction or perforation by intraabdominal translocated IUDs is extremely rare [9].
Case Presentation
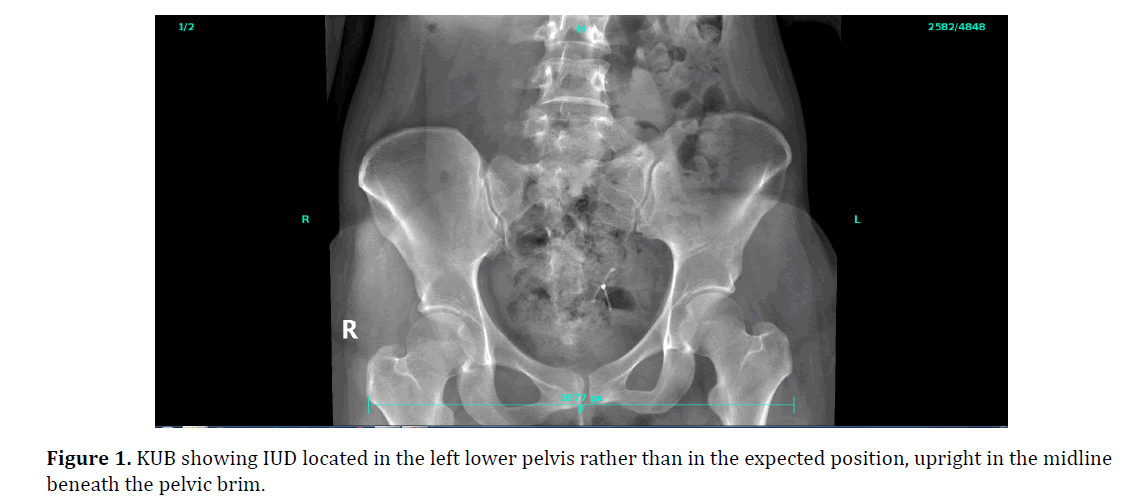
Progestin (Skyla) IUD placed for contraception. Her gynecological exam was significant for a retroflexed uterus. At her scheduled one-month follow-up visit, the retrieval strings of her IUD available through her cervix were noted to be short. Over the next six months, the patient developed menorrhagia. A pelvic ultrasound was obtained which showed that the IUD was not intrauterine. The presumption was that the device had been expelled; however, a KUB (kidney, ureter, and bladder X-ray) obtained ten months later showed the device in the left lower pelvis (Figure 1). Aside from the menorrhagia, the patient was asymptomatic and her abdominal examination was normal. She was therefore scheduled by her gynecologist for elective laparoscopic removal of the translocated IUD, hysteroscopic evaluation of the uterine cavity, and placement of a new hormonal IUD.
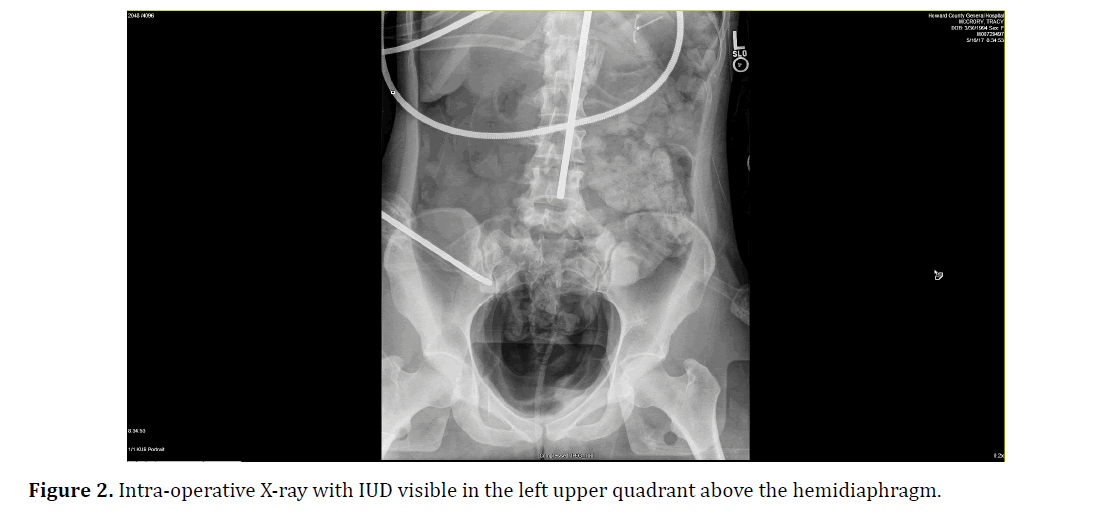
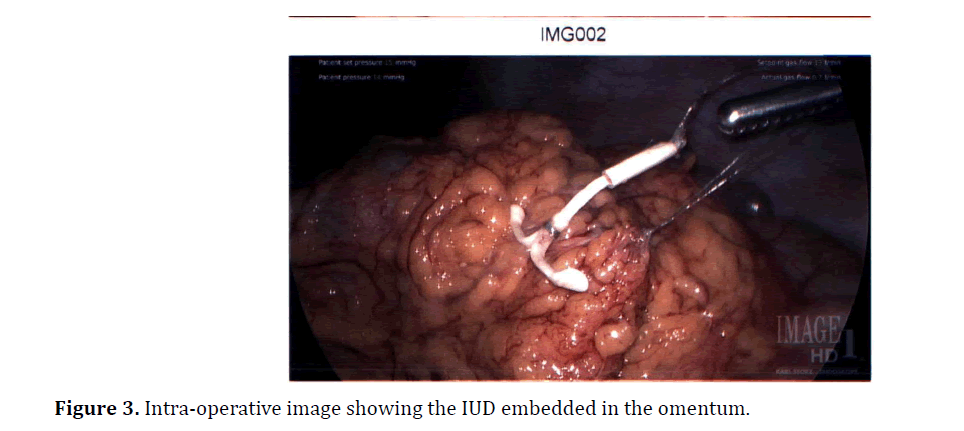
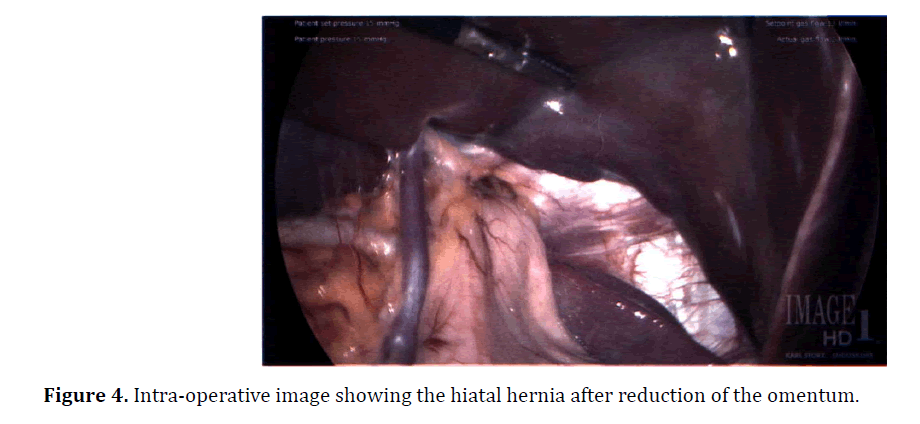
On diagnostic laparoscopy, the IUD could not be located. At this point an intra-operative general surgery consult was obtained. Intra-operative X-ray revealed the IUD in the chest, above the left hemi-diaphragm (Figure 2). An additional 5 mm port was placed in the mid-abdomen. At this point a previously undiagnosed hiatal hernia was discovered that included omentum and the upper third of the stomach. These contents were reduced. X-ray was repeated, which showed the IUD now in the mid-abdomen. Close inspection of the omentum showed the device embedded within the omentum (Figure 3). The device was removed from the abdomen through one of the laparoscopic ports (Figure 4). Hysteroscopy showed a normal intact uterine cavity without evidence of scar. A new Mirena IUD was placed in the fundus of the uterus and its position confirmed by hysteroscopy and laparoscopy.
Outcome and follow-up
The patient was discharged home from the recovery room, and her new IUD was noted to be appropriately positioned by cervical exam at a follow-up visit. Because the patient’s paraesophageal hernia was asymptomatic, she opted not to pursue repair.
Result and Discussion
Translocated IUDs have previously been reported to cause ureteral obstruction, small bowel perforation and obstruction, rectouterine fistula, and bladder perforation [10-13]. One-third to one-half of all translocated IUDs are embedded in the omentum [5,14]. To our knowledge, this is the first reported case of IUD migration into the mediastinum.
Hiatal hernias occur in the setting of defects in the phrenoesophageal membrane, which connects the diaphragm to the distal esophagus. Degeneration of this membrane allows abdominal contents to pass through the esophageal hiatus of the diaphragm and into the posterior mediastinum, which in addition to the esophagus also contains the descending aorta, azygos vein, thoracic duct, and vagus nerves. Obesity, aging, and musculofascial degeneration are thought to contribute to such enlargement of the esophageal hiatus. In 95% of hiatal hernias, the gastroesophageal junction and part or all of the stomach herniate, known as a type I or sliding hiatal hernia. Patients may present with dysphagia, epigastric fullness, or reflux; or, like the patient described in this case, may have no symptoms at all [15]. The asymptomatic nature may contribute to the current poor estimates of hiatal hernia prevalence, which range from 10%-80% [16].
The exact time of IUD translocation in this patient remains unknown, although the greatest risk for uterine perforation is during device placement. The patients at highest risk for uterine perforation during IUD placement are those recently postpartum and those breastfeeding, thought to be related to the effect of low estrogen levels on the uterine wall [9]. The patient in this case lacked these risk factors, though she did have a retroflexed uterus. There are conflicting opinions as to whether a retroflexed uterus is a risk factor for IUD migration [5,17,18]. The uterus is located between the bladder and the rectosigmoid colon and is supported in the pelvis by several ligaments. A uterus is retroflexed when the fundus is located posterior to the axis of the cervix, compared to the more common anteflexed anatomic variant in which the fundus is tilted forward [19]. This anatomy is thought to increase the risk of passing the sound through the anterior edge of the body of the uterus, instead of into the uterine cavity as intended. As in this case, it is common for the uterus to show no indications of injury on hysteroscopic exam to indicate the site of translocation; the endometrium can heal within weeks of damage [20]. Based on the prior ultrasound and pelvic exam, this patient’s IUD is known to have translocated sometime in the six-month interval following placement.
Some practitioners support conservative management of asymptomatic patients with IUD migration, arguing that the risk of complications during surgery does not justify treatment [21-23]. In contrast, the World Health Organization recommends immediate retrieval of intra-abdominal IUDs, which have the potential to cause adhesions and as such are a risk factor for chronic pelvic pain, infertility, intestinal obstruction, abscesses, and fistula formation [24]. At the time of surgery, this patient had not experienced any of these complications. However, given the demonstrated capacity of translocated IUDs to cause intra-abdominal perforations and fistulas, the presence of the IUD in this patient’s posterior mediastinum posed a clear risk to the structures therein. These possible complications favor removal of such a device, even if asymptomatic.
Conclusion
1. Hiatal hernias are commonly asymptomatic and may serve as a route for passage of abdominal contents into the posterior mediastinum.
2. IUD migration can present with pain, unintended pregnancy, abnormal uterine bleeding, or can be asymptomatic.
3. In the outpatient evaluation of a possible translocated IUD, pelvic ultrasound should be used to locate the IUD in the uterus. If the IUD is suspected to be elsewhere in the abdomen, abdominal X-ray or CT scan may be used and should be repeated just before surgery
References
- Trends in Contraceptive Use Worldwide 2015
- Kaiser Family Foundation. Intrauterine Devices (IUDs): Access for women in the US. 2016
- Bayer Pharmaceuticals. Mirena Insertion and Removal for Healthcare Professionals. 2018
- Boortz HE, Margolis DJ, Ragavendra N, Patel MK, Kadell BM. Migration of intrauterine devices: Radiologic findings and implications for patient care. Radiographics 2012;32(2):335-352.
[Crossref] [Google Scholar] [Pubmed]
- Zakin D, Stern WZ, Rosenblatt R. Complete and partial uterine perforation and embedding following insertion of intrauterine deives. I. Classification, complications, mechanism, incidence, and missing string. Obstet Gynecol Surv 1981;36(7):335.
[Crossref] [Google Scholar] [Pubmed]
- Heartwell SF, Schlesselman SA. Risk of uterine perforation among users of intrauterine devices. Obstet Gynecol 1983;61(1):31-36.
- Andersson K, Ryde-Blomqvist E, Lindell K, Odlind V, Milsom I. Perforations with intrauterine devices: Report from a Swedish survey. Contraception 1998;57(4):251-255.
[Crossref] [Google Scholar] [Pubmed]
- Heinemann K, Reed S, Moehner S, Do Minh T. Risk of uterine perforation with levonorgestrel-releasing and copper intrauterine devices in the European Active Surveillance Study on Intrauterine Devices. Contraception 2015;91(4):274-279.
[Crossref] [Google Scholar] [Pubmed]
- Kaislasuo J, Suhonen S, Gissler M, Lähteenmäki P, Heikinheimo O. Intrauterine contraception: Incidence and factors associated with uterine perforation-a population-based study. Hum Reprod 2012 ;27(9):2658-2663.
[Crossref] [Google Scholar] [Pubmed]
- Bozkurt IH, Basmaci I, Yonguc T, Aydogdu O, Aydin ME, Sefik E, et al. Hydronephrosis due to a migrated intrauterine device into the ureter: A very rare case. Eurasian J Med 2018;50(2):137.
[Crossref] [Google Scholar] [Pubmed]
- Jones D. Young woman with abdominal pain. Ann Emerg Med 2014;64(4):425.
[Crossref] [Google Scholar] [Pubmed]
- Kho KA, Chamsy DJ. Perforated intraperitoneal intrauterine contraceptive devices: Diagnosis, management, and clinical outcomes. J Minim Invasive Gynecol 2014;21(4):596-601.
[Crossref] [Google Scholar] [Pubmed]
- Tosun M, Celik H, Yavuz E, Çetinkaya MB. Intravesical migration of an intrauterine device detected in a pregnant woman. Can Urol Assoc J 2010;4(5):E141E143.
[Crossref] [Google Scholar] [Pubmed]
- Agacayak E, Tunc SY, Icen MS, Oguz A, Ozler A, Turgut A, et al. Evaluation of predisposing factors, diagnostic and treatment methods in patients with translocation of intrauterine devices. J Obstet Gynaecol Res 2015;41(5):735-741.
[Crossref] [Google Scholar] [Pubmed]
- Allaix ME, Patti MG. Esophagus and diaphragm. In: Doherty GM. Current Diagnosis and Treatment: Surgery, 14th edn New York, 2014.
- Weston AP. Hiatal hernia with cameron ulcers and erosions. Gastrointest Endosc Clin N Am 1996;6(4):671-679.
[Crossref] [Google Scholar] [Pubmed]
- Hasson HM. Clinical experience with intrauterine devices in a private practice. Adv Contracept 1985;1(1):51-61.
[Crossref] [Google Scholar] [Pubmed]
- Chi IC, Farr G, Dominik R, Robinson N. Do retroverted uteri adversely affect insertions and performance of IUDs?. Contraception 1990;41(5):495-506.
[Crossref] [Google Scholar] [Pubmed]
- Sosa-Stanley JN, Peterson DC, Ameer MA, Fagan SE. Anatomy, Abdomen and Pelvis, Uterus.
- Margarit LM, Griffiths AN, Vine SJ. Management of levonorgestrel-releasing intrauterine system (LNG-IUS) uterine perforation. J Obstet Gynaecol 2004;24(5):586-587.
[Crossref] [Google Scholar] [Pubmed]
- Uçar MG, Şanlıkan F, Ilhan TT, Göçmen A, Çelik Ç. Management of intra-abdominally translocated contraceptive devices, is surgery the only way to treat this problem?. J Obstet Gynaecol 2017;37(4):480-486.
[Crossref] [Google Scholar] [Pubmed]
- Kaislasuo J, Suhonen S, Gissler M, Lähteenmäki P, Heikinheimo O. Uterine perforation caused by intrauterine devices: Clinical course and treatment. Hum Reprod 2013;28(6):1546-1551.
[Crossref] [Google Scholar] [Pubmed]
- Adoni A, Chetrit AB. The management of intrauterine devices following uterine perforation. Contraception 1991;43(1):77-81.
[Crossref] [Google Scholar] [Pubmed]
- World Health Organization. Mechanism of action, safety and efficacy of intrauterine devices. Report of a WHO scientific group. World Health Organ Tech Rep Ser 1987;753:1-91.
[Google Scholar] [Pubmed]