Case Report - Archives of Clinical and Experimental Surgery (2022)
Prepyloric Perforation Following Blunt Trauma Abdomen
Sarvagya Jain*, Prakhar Chaudhary, Lavanya Kelam, Arvind Ghanghoria and Hemant ThannaSarvagya Jain, Department of General Surgery, M.Y. Hopsital, Indore, India, Email: sarvagyajain25@gmail.com
Received: 07-Mar-2022, Manuscript No. EJMACES-22-61084; Editor assigned: 09-Mar-2022, Pre QC No. EJMACES-22-61084 (PQ); Reviewed: 23-Mar-2022, QC No. EJMACES-22-61084; Revised: 28-Mar-2022, Manuscript No. EJMACES-22-61084 (R); Published: 04-Apr-2022
Abstract
Introduction: Gastric perforation following blunt trauma abdomen is a very rare presentation.
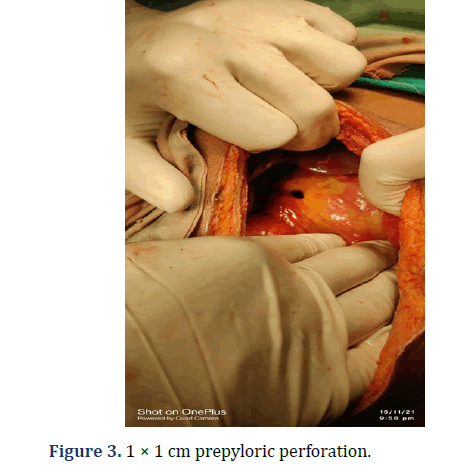
Case Report: 35 year male presented with acute abdomen following road traffic accident, which had undergone exploratory laprotomy, and there was prepyloric perforation, with no solid organ injury which was repaired.
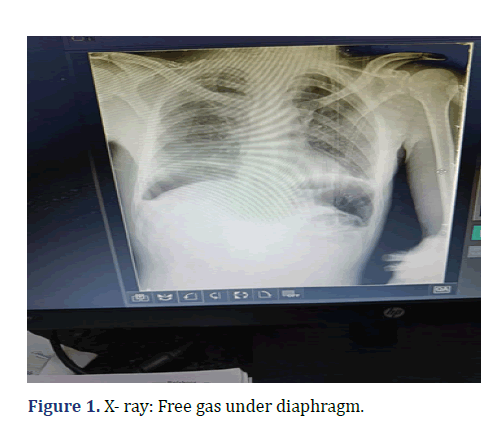
Discussion: Mainly gastric perforation is associated with other solid organ injuries like liver, spleen, pancreas, lungs. Diagnosis by x-ray and CT scan, free gas under diaphragm and the repair can be done as routine. Mortality is due to sepsis.
Conclusion: Gastric rupture is a rare presentation following blunt injury abdomen. Commonly traumatic gastric rupture is associated with other injuries like splenic injury and fractures.
https://matadorbet-giris.com https://grandpashabeti.com https://betiste.com https://bahsegelgirisi.com https://klasbahisgirisi.com https://jasminbeti.com https://hepsibahise.com https://dinamobetgirisi.com https://betvolegirisi.com https://betpark-girisi.com https://betlikegiris.com https://betboogirisi.com https://sultanbetegiris.com https://tulipbetgir.com https://padisahbetegir.com https://savoybettinge.com https://goldenbahisegiris.com https://maksibetgirise.com https://fenomengiris.com https://jojobetgiris.xyz https://tarafgiris.com
Keywords
Blunt trauma abdomen; Gastric perforation; solid organ injury
Introduction
Blunt abdominal trauma due to Road Traffic Accident is one of the leading causes of death from pediatric age group to old age. The abdomen is the third most commonly injured anatomic region after Head and Extremities. In blunt trauma abdomen solid organ (liver, spleen and kidney), diaphragmatic, pancreatic and retroperitoneal injury are mainly injured. Hollow viscera injuries to duodenum, jejunum, urinary bladder and the colo-rectum are also common with an incidence that varies between 4%-15% [1,2]. However, by contrast, gastric perforations following BAT have an incidence of between 0.02%-1.7% only. A multicentre retrospective analysis of blunt gastric injuries from four trauma centers in Brazil over a 14 year period yielded only 33 cases of gastric perforation [3]. The rarity of gastric perforation developing following BAT in civilian practice together with the inconsistent diagnostic yield from standard investigations has led to this condition being invariably recognized at laparotomy. In this case report we describe an anterior gastric perforation following BAT due a motor vehicle accident.
Case Report
35 year male, referred from District Hospital presented in our emergency with Allied history of trauma due to road traffic accident 2 wheeler versus truck 3 days back. Patient had a chief complaint of abdominal pain since then, fever and decreased appetite since 2 days. There was no history of vomiting, bleeding per rectal. Patient was passing motion and flatus normally. There was no Nervous System involved.
On Examination, patient was vitally stable. On auscultation of chest there was bilateral decrease in basal lungs. On per abdomen examination, there was distension, generalized tenderness, guarding was present. Per rectal Examination was normal.
Investigation
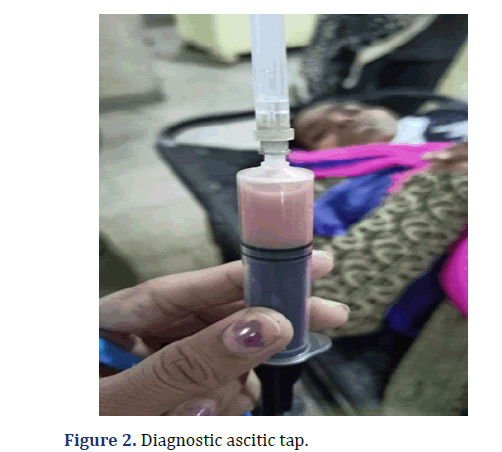
WBC count was raised to 18600. X-ray Showed, Free Gas Under diaphragm (Figure 1). USG showed, Mild to moderate amount of ascites with moving echoes. On aspiration, there was Pus (Figure 2). Intervention, Exploratory Laprotomy was performed. There was 1000 ml pyoperitonium and a 1 × 1 cm prepyloric perforation. There was no solid organ injury. Modiefied Graham’s patch repair with Ryle’s tube insertion was done with bilateral drain placement (Figure 3).
Post op and Recovery: Patient was vitally stable and active RT suctioning Patient accidently pulled out RT on POD 3 Patient was kept NBM for 7 days. Then slowly oral diet was allowed, and then on POD 14 patient was discharged.
Discussion
Traumatic stomach rupture following blunt injury abdomen is a very rare presentation. Stomach being mobile with strong walls and being protected by ribs usually escapes injury in blunt trauma, however if the stomach is distended due to food, liquid or gas it is more likely to get injured than when it is empty [4]. Grading of gastric injuries is shown in Table 1.
| Grade I | Intramural hematoma b 3 cm Partial thickness laceration |
|
|---|---|---|
| Grade II | Laceration |
2 cm in GE junction/pylorus |
| Grade III | Laceration |
2 cm in GE junction/pylorus |
| Grade IV | Vascular |
Tissue loss/devascularisation ≤ two-third stomach |
| Grade V | Vascular |
Tissue loss/devascularisation ≥ two-third stomach |
Gastric perforations due to BAT may develop in any location of the stomach. The most common location for gastric perforation is the anterior wall (40%) followed by the greater curvature (23%), lesser curvature (15%) and posterior wall (15%). Such perforations are invariably solitary; to date only 3 cases of a double gastric perforation following BAT have been described [3].
In blunt trauma abdomen, there are three different mechanisms of causing injury to gastrointestinal organs are described. Firstly, the burst injury, which occurs, when rapid compressive forces are applied to a filled and distended hollow viscous, without direct mechanical compression. Second, is the crush injury that occurs when an organ is compressed violently against the spine? Third is the shear injury, caused by rapid acceleration-deceleration of an organ at one point of fixation [5].
Studies show that rise in intraluminal pressure can cause a sequential rupture of the wall of the stomach, firstly the seromuscular coat, then the mucosa, and finally the submucosa [6]. Partial rupture of the stomach wall can occur and it may progress to full thickness rupture at a later stage. The anterior gastric wall is the most common site of rupture, followed by the greater curvature, the lesser curvature and the posterior wall [7]. Gastric rupture is usually associated with solid organ injuries like liver, pancreas, spleen and lungs [8].
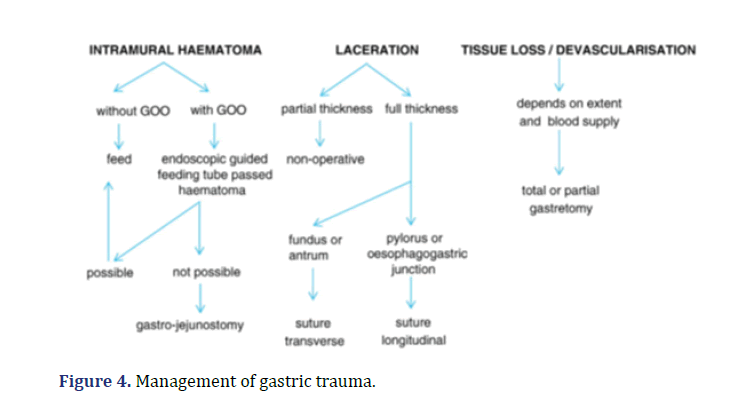
Gastric perforations can be diagnosed with x-ray and CT scan by identifying free gas. Mortality is mainly due to sepsis. Morbidity and mortality increases parallel with time to operative intervention (intervention within 8 h is associated with a 2% mortality, intervention within 8 to 16 h with a 9% mortality, intervention within 16 to 25 h, a 17% mortality and intervention after 24 h over 30% mortality). The overall reported mortality ranges from 0%–66%. Management of gastric trauma shown in Figure 4.
At laparotomy it is mandatory to exclude a separate gastric laceration (for example, along the posterior gastric wall). Grades 1to 3 gastric injuries (the majority of gastric injuries) are amenable to primary repair; a 2 layer closure is advocated to effect haemostasis. Grade 4 (tissue loss with devascularisation affecting b50% of stomach) and Grade 5 (tissue loss with devascularisation affecting N50% of stomach) gastric injuries are uncommon, associated with other organ and major vascular injuries; affected patients rarely reach hospital alive.
In the light of the extent of the injuries, primary repair will not be feasible in patients with Grades 4 and 5 gastric injuries Depending on the location of the tissue loss (proximal vs. distal stomach) and extent of devascularisation, sub-total or rarely total gastrectomy may have to be undertaken. The options to restore gastrointestinal continuity will be influenced by the presence of associated injuries (to duodenum, bile duct and pancreas) and include a gastro-duodenostomy, gastro-jejunostomy or a Rouxen-Y reconstruction.
Conclusion
Gastric rupture is a rare presentation following blunt injury abdomen. Commonly traumatic gastric rupture is associated with other injuries like splenic injury and fractures. Prompt diagnosis and early intervention reduces mortality and morbidity. Hollow viscus injuries after blunt trauma, though uncommon, can have serious consequences if the diagnosis is missed or delayed.
References
- Isenhour JL, Marx J. Advances in abdominal trauma. Emerg Med Clin North Am 2007; 25(3):713-33.
[Crossref] [Google Scholar] [Pubmed]
- Talton DS, Craig MH, Hauser CJ, Poole GV. Major gastroenteric injuries from blunt trauma. Am Surg 1995; 61(1):69-73.
[Google Scholar] [Pubmed]
- Aboobakar MR, Singh JP, Maharaj K, Kinoo SM, Singh B. Gastric perforation following blunt abdominal trauma. Trauma Case Rep 2017;10:12-5.
[Crossref] [Google Scholar] [Pubmed]
- Deshpande AD, Sivapragasam S. Isolated posterior gastric injury due to blunt abdominal trauma. Emerg Med J 2003; 20(6):566.
[Crossref] [Google Scholar] [Pubmed]
- Steven S, Pearl RH. Abdominal trauma. In: Grosfeld JL, O'Neal SA Jr, Fonkalsrud EW, Coran AG, editors. Pediatric Surgery. 6th ed 2006. 295–316.
- Silbergleit A, Berkas EM. Neonatal gastric rupture. Minn Med 1966; 49: 65-8. [Crossref]
[Google Scholar] [Pubmed]
- Nanji SA, Mock C. Gastric rupture resulting from blunt abdominal trauma and requiring gastric resection. J Trauma 1999; 47(2): 410-2.
[Crossref] [Google Scholar] [Pubmed]
- Shinkawa H, Yasuhara H, Naka S, Morikane K, Furuya Y, Niwa H, et al. Characteristic features of abdominal organ injuries associated with gastric rupture in blunt abdominal trauma. Am J of Surgery 2004; 187(3):394-7.
[Crossref] [Google Scholar] [Pubmed]
Copyright: © 2022 The Authors. This is an open access article under the terms of the Creative Commons Attribution NonCommercial ShareAlike 4.0 (https://creativecommons.org/licenses/by-nc-sa/4.0/). This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.