Research Article - Archives of Clinical and Experimental Surgery (2023)
Randomised Control Study to Assess the Effect of Methylene Blue and Lignocaine as Analgesic in Perianal Surgery in M.Y. Hospital
Srashti Shah*, Ankur Maheshwari and Avinash GautamSrashti Shah, Department of General Surgery, M.G.M. Medical College and M.Y. Hospital, Madhya Pradesh, India, Email: srashiq380@gmail.com
Received: 25-Jan-2023, Manuscript No. EJMACES-23-87885; Editor assigned: 27-Jan-2023, Pre QC No. EJMACES-23-87885 (PQ); Reviewed: 13-Feb-2023, QC No. EJMACES-23-87885; Revised: 20-Feb-2023, Manuscript No. EJMACES-23-87885 (R); Published: 28-Feb-2023
Abstract
Background: Perianal surgeries have been associated with considerable postoperative pain and discomfort. Perianal intradermal injection of methylene blue has been shown to ablate perianal nerve endings and bring about temporary pain relief.
Method: A randomized, prospective, single-blind placebo-controlled trial was conducted. Patients were randomized to intradermal injection at perianal surgeries of either 6 ml of 1% methylene blue and 6 ml of 1% lignocaine or 12 ml of 1% lignocaine. Thus, a total of 12 ml was injected into the perianal skin of each patient prior to surgical dissection. Patients were asked to fill in a pain diary with a visual analogue scale. The primary outcome measure was pain score and analgesic use. Secondary outcomes were complications.
Results: There were 25 patients in the methylene blue arm and 25 patients in the placebo arm. There were no statistically significant differences in the sex, type of hemorrhoid, number of hemorrhoids excised, duration of surgery or hospital stay. The mean pain scores were significantly lower and the use of paracetamol was also significantly less in the methylene blue group during the first three postoperative days. Other complication rates were not significantly different.
Conclusion: Perianal intradermal injection of methylene blue was useful in reducing the initial postoperative pain of perianal surgeries.
Keywords
Intradermal methylene blue; Milligan Morgan hemorrhoidectomy; Open hemorrhoidectomy; Cardiac functional prognosis; Post- operative pain
Introduction
Painful conditions of the anal and perianal region are not only the frequently encountered problems in surgical practice but also form the most distressing symptoms to the suffering. Patient with conditions such as bleeding, mass, discharge and pruritus and incapacitate the day to day life of the sufferer [1]. Proper clinical assessment and appropriate management of these conditions definitely alleviates the pain, anxiety and distress of the patient. Hemorrhoids are the most common benign anal disease encountered by physicians and surgeons [2]. A lifetime risk of hemorrhoids could be as high as 75% in the general population [3-5].
A systematic review and network meta-analysis of various operations for Hemorrhoids demonstrated that non-excisional surgeries, such as doppler-guided hemorrhoidal artery ligation and stapled hemorrhoidopexy, were less painful than excisional hemorrhoidectomy [6].
However, the latter had less recurrence and was associated with a lower cost of surgical instruments. Moreover, both internal and external components of hemorrhoids can be effectively removed by hemorrhoidectomy. As a result, hemorrhoidectomy with Milligan-Morgan hemorrhoidectomy operation considered as the gold standard classic hemorrhoid resection procedure, which is still regarded as the mainstay operation for advanced and/or complicated hemorrhoids with a persistent problem of postoperative pain post-hemorrhoidectomy [7,8]. The incidence moderate to severe pain following conventional hemorrhoidectomy reported in the anecdotal literature could be as high as 65% [9]. Methods including oral administration or intramuscular injection of analgesic drugs, local application of nitroglycerin ointment, and injection of kreotoxin have been commonly used to alleviate postoperative pain [10].
Clinical observations have shown that subcutaneous injection of methylene blue plus ropivacaine around the incision could achieve relatively long analgesic effect. Methylene Blue (MB) is commonly used as biologic stain but it also possesses nerve disruption quality. Pain and itch receptors are nerve endings that are not myelinated, located in the papillary layer of the skin with the highest numbers being in the epidermis and dermis. When this receptor is stimulated, excitatory neurons transmitted impulses to the dorsal horn of spinal cord and then continued to central nervous system to create pain or itch sensation. This mechanism explains the efficacy of MB to reduce pain.
Mechanism of action of methylene blue as analgesia
Methods including oral administration or intramuscular injection of analgesic drugs, local application of nitroglycerin ointment, and injection of kreotoxin have been commonly used to alleviate postoperative pain. The local use of anaesthetic drug to control postoperative pain at the wound site has been popular because of its convenience and remarkable efficacy.
Methylene blue is a nontoxic dye agent that inhibits the soluble guanylate cyclase and nitric oxide synthase. Nitric oxide regulates physiological functions such as pain and analgesia by activating soluble guanylate cyclase to increase intracellular cyclic guanosine monophosphate. Methylene blue, as an oxidizing-reducing agent, demonstrates a strong affinity to nerve tissues when applied locally, which can directly block the electrical conductivity of nerve fibres, thereby affecting the neural excitability and impulse conductivity.
Recent studies have shown that a low dose (0.5% or 1%) of methylene blue may block peripheral nerve fibres at the incision. A local injection of methylene blue could cause reversible damage to the incision and its surrounding subcutaneous nerve terminal medulla, thus achieving a long-acting postoperative analgesic effect.
However, the damage will cause a burning sensation between 2 to 4 hours after injection. To eliminate this burning sensation, methylene blue is combined with local anaesthetic drugs.
Aims and objectives
• To study importance of methylene blue and lignocaine as analgesic in perianal surgeries.
• Evaluate analgesic effects of methylene blue and lignocaine by measuring the level of pain using visual analogue scale.
• To assess complications.
Materials and Methods
The present study entitled “A randomised control study to assess the effect of methylene blue and lignocaine as analgesic in perianal surgery in M.Y. Hospital” was under taken in the Department of General Surgery, M.G.M Medical College and M.Y Hospital after valid approval of ethics committee of the institution.
Study design
The design of present research study was Randomised control study.
Study centre
Department of General Surgery, MGM Medical College and M.Y. Hospital, Indore
Study was undertaken for a period of 12 months after the approval from the ethical committee i.e., March 2021 to February 2022.
Duration of the study:
• Group 1 (case group): 25 Patients who received 5 ml lignocaine + 5 ml bupivacaine and 2 ml methylene blue (Total solution 12 ml) as block in perianal sur- geries.
• Group 2 (case group ): 25 patients who received 6 ml lignocaine and 6 ml bupivacaine (Total solution 12 ml) as block in perianal surgeries.
The results of this research are expected to identify the current state of research and provide evidences to sup- port further clinical and review investigations on the use of Methylene blue as analgesic in perianal surgery.
Inclusion criteria• All patients of age more than 18 years who are un- dergoing open methods for Hemorrhoids, Peri-anal fistula, Fissure in ano, Anal abscess in department of surgery, MGM Medical College and M Y Hospital.
• Consent given by patient and care taker are included in the study
Exclusion criteria
• Following class of patients were excluded
• Patient who are sensitive for methylene blue injection excluded from study to avoid anaphylaxis reactionsImmuno compromised patients.
Method
After taking pre-informed written consent from the patient, a prestructured proforma was used to collect the desired baseline data.
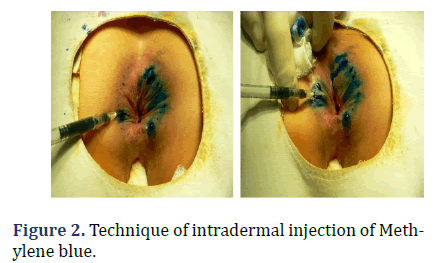
The Methylene blue intradermal-injection therapy consisted of 2 ml of 1% methylene blue and 5 ml of 1% lignocaine and 5 ml of bupivacaine. Thus, a total of 12 ml was injected into the perianal skin of each patient .
Injection method for the treatment Group 1: after the operation was completed, the compound solution was hypodermically injected with a skin test needle around all incisions. The needlepoint was approximately 1 cm away from the incision edge. The needle orientation was approximately 45 degrees from the skin. Uniform injections were given at each injection point in the upper, lower, left and right directions with 0.5 mL of injection drug per injection point. The distance between every two injection points was 1 cm. After the injection, the drug solution was spread evenly by gently rubbing the area with gauze.
The control Group 2: 6 ml of 1% lignocaine and 6 ml bupivacaine intra dermal injection twice a day for 5 days after the surgery. For patients in both groups, if the Visual Analogue Scale (VAS) pain score was equal to or greater than 5, an additional lignocaine injection was provided. If the pain still could not be alleviated, an extra intramuscular injection of pethidine hydrochloride was offered.
Follow-up with VAS pain scores for two groups of patients between days 1 and 14 after the surgery, on a scale between 0 and 10 (VAS, 0=no pain, 10=severe pain) (Figures 1 and 2).
Results and Discussion
Table 1 shows the association between Post-op Wound Infection and Study Group.
| Post-op wound infection | Group | Total | ||
|---|---|---|---|---|
| Group1 | Group 2 | |||
| NO | Count | 21 | 21 | 42 |
| % | 84.00% | 84.00% | 84.00% | |
| YES | Count | 4 | 4 | 8 |
| % | 16.00% | 16.00% | 16.00% | |
| TOTAL | Count | 25 | 25 | 50 |
| % | 100.00% | 100.00% | 100.00% | |
| Pearson Chi-Square | Value | df | P Value | Result |
| .000a | 1 | 1 | Non Sig | |
Chi square test for association between two variables was applied, which shows that there was non-significant association between Post-op Wound Infection and Study Group (P>0.05). For Group 1, the highest proportion 84.0% was for No Status and lowest value 16.0% was for Yes Status. Similarly for Group 2, the highest proportion 84.0% was for No Status and lowest value 16.0% was for Yes Status.
Table 2 shows the association between Post-op Incontinence and Study Group. As there was 100% for not having any post-operative incontinence in both study groups, hence no further statistical analysis was performed.
| Post op incontinence | Group | Total | ||
|---|---|---|---|---|
| Group 1 | Group 2 | |||
| NO | Count | 25 | 25 | 50 |
| % | 100.00% | 100.00% | 100.00% | |
| TOTAL | Count | 25 | 25 | 50 |
| % | 100.00% | 100.00% | 100.00% | |
| Pearson Chi-Square | Value | df | P Value | Result |
| NA | 0 | 0 | 0 | |
Table 3 shows the association between Post-op Recurrence and Study Group.
| Post op recurrence | Group | Total | ||
|---|---|---|---|---|
| Group1 | Group 2 | |||
| NO | Count | 21 | 24 | 45 |
| % | 84.00% | 96.00% | 90.00% | |
| YES | Count | 4 | 1 | 5 |
| % | 16.00% | 4.00% | 10.00% | |
| TOTAL | Count | 25 | 25 | 50 |
| % | 100.00% | 100.00% | 100.00% | |
| Pearson Chi-Square | Value | df | P Value | Result |
| 2.000a | 1 | 0.157 | Non Sig | |
Chi square test for association between two variables was applied, which shows that there was non-significant association between Post-op Recurrence and Study Group (P>0.05). For Group 1, the highest proportion 84.0% was for No Status and lowest value 16.0% was for Yes Status. Whereas for Group 2, the highest proportion 96.0% was for No Status and lowest value 4.0% was for Yes Status.
Table 4 shows the association between Follow up Day-1 and Study Group.
| Follow up day 1 | Group | Total | ||
|---|---|---|---|---|
| Group1 | Group 2 | |||
| None | Count | 23 | 22 | 45 |
| % | 92.00% | 88.00% | 90.00% | |
| Wound infection | Count | 2 | 3 | 5 |
| % | 8.00% | 12.00% | 10.00% | |
| TOTAL | Count | 25 | 25 | 50 |
| % | 100.00% | 100.00% | 100.00% | |
| Pearson Chi-Square | Value | df | P Value | Result |
| .222a | 1 | 0.637 | Non Sig | |
Chi square test for association between two variables was applied, which shows that there was non-significant association between Follow up Day-1 and Study Group (P>0.05). For Group 1, the highest proportion 92.0% was for No infection and lowest value 8.0% was for Wound Infection. Whereas for Group 2, the highest proportion 88.0% was for No infection and lowest value 12.0% was for Wound Infection.
Table 5 shows the association between Follow up Day-3 and Study Group.
| Follow up day 3 | Group | Total | ||
|---|---|---|---|---|
| Group1 | Group 2 | |||
| None | Count | 20 | 23 | 43 |
| % | 80.00% | 92.00% | 86.00% | |
| Wound infection | Count | 5 | 2 | 7 |
| % | 20.00% | 8.00% | 14.00% | |
| TOTAL | Count | 25 | 25 | 50 |
| % | 100.00% | 100.00% | 100.00% | |
| Pearson Chi-Square | Value | df | P Value | Result |
| 1.495a | 1 | 0.221 | Non Sig | |
Chi square test for association between two variables was applied, which shows that there was non-significant association between Follow up Day-3 and Study Group (P>0.05). For Group 1, the highest proportion 80.0% was for No infection and lowest value 20.0% was for Wound Infection. Whereas for Group 2, the highest proportion 92.0% was for No infection and lowest value 8.0% was for Wound Infection.
Table 6 shows the association between Follow up Day- 14 and Study Group.
| Follow up day 14 | Group | Total | ||
|---|---|---|---|---|
| Group1 | Group 2 | |||
| None | Count | 24 | 24 | 48 |
| % | 96.00% | 96.00% | 96.00% | |
| Wound infection | Count | 1 | 1 | 2 |
| % | 4.00% | 4.00% | 4.00% | |
| TOTAL | Count | 25 | 25 | 50 |
| % | 100.00% | 100.00% | 100.00% | |
| Pearson Chi-Square | Value | df | P Value | Result |
| .000a | 1 | 1 | Non Sig | |
Chi square test for association between two variables was applied, which shows that there was non-significant association between Follow up Day-14 and Study Group (P>0.05). For Group 1, the highest proportion 96.0% was for No infection and lowest value 4.0% was for Wound Infection. Whereas for Group 2, the highest proportion 96.0% was for No infection and lowest value 4.0% was for Wound Infection.
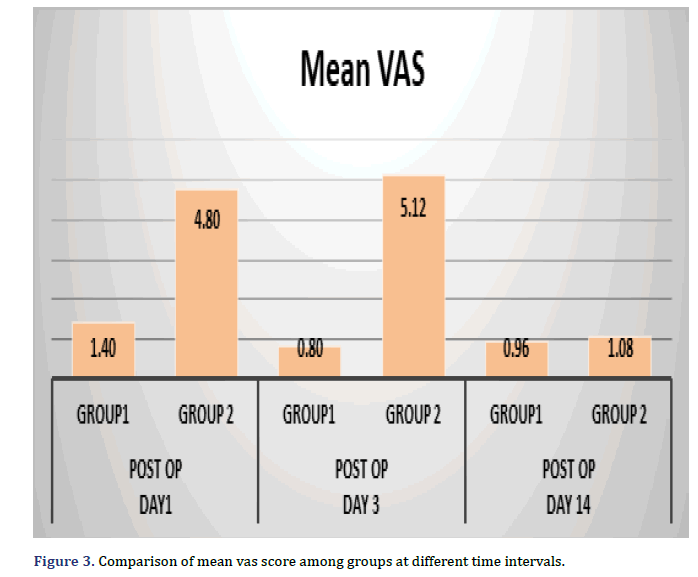
Table 7 shows the comparison of mean VAS score among two study groups at different Time Intervals.
| Time interval | Group | N | Mean VAS | Std. Deviation | T Test | P Value | Result |
|---|---|---|---|---|---|---|---|
| Post OP | Group1 | 25 | 1.4 | 0.957 | -8.981 | 0 | Sig |
| Day1 | Group 2 | 25 | 4.8 | 1.633 | |||
| Post OP | Group1 | 25 | 0.8 | 0.866 | -15.173 | 0 | Sig |
| Day 3 | Group 2 | 25 | 5.12 | 1.13 | |||
| Post OP | Group1 | 25 | 0.96 | 0.79 | -0.498 | 0.621 | Non Sig |
| Day 14 | Group 2 | 25 | 1.08 | 0.909 |
At Post-Op Day-1, the mean value 1.40 was for group-1 which was significantly lower than the mean value 4.80 was for group-2. At Post-Op Day-3, the mean value 0.80 was for group-1 which was significantly lower than the mean value 5.12 was for group-2. At Post-Op Day-14, the mean value 0.96 was for group-1 which was non-significantly lower than the mean value 1.08 was for group-2. Comparison of Mean VAS score Among Groups at Different Time Intervals shown in Figure 3.
Methylene Blue (MB) has been found to have unique analgesic property through temporary disruption of sensory nerve conduction. In anorectal surgery, MB is widely used as a biologic stain but the analgesic effect has never been studied. In advent of same, the present study was planned and purposed to assess the effect of methylene blue and lignocaine as analgesic in perianal surgery and to assess the efficacy and analgesic potential of the combination when used together. Further, an assessment of complications, if any was also done.
The followings results were obtained:
1. Out of 50 total patients, maximum patients were operated via Fistulectomy i.e., 21 (42%) followed by 10 (20%) for Sinus excision, 6 (12%) for Open hemorrhoidectomy, 5 for Stapler Hemorrhoidectomy. And 2 each of fissurectomy, Lateral internal Sphincterotomy, Open hemorrhoidectomy and minimum 1 patient was incidence for Fistulotomy.
2. Non-significant association between Post-op Wound Infection and Study Group (P>0.05)
3. For post op complications, 100% (50) for not having any post-operative incontinence in both study groups, hence no further statistical analysis was performed.
4. Non-significant association between Post-op Recurrence and Study Group (P>0.05).
5. A non-significant association (P>0.05) was observed between follow up Day 1, Day 3 and Day 14 and Study groups.
6. Though pain scores fell significantly in both groups (p<0.01), mean VAS Score was significantly lower in methylene blue group as compared to controls with conventional analgesics through the period of 3 post-operative days (p<0.01).
i. At Post-Op Day-1, the mean value 1.40 ± 0.957 was for group-1 which was significantly lower than the mean value 4.80 ± 1.633 was for group-2.
ii. At Post-Op Day-3, the mean value 0.80 ± 0.866 was for group-1 which was significantly lower than the mean value 5.12 ± 1.130 was for group-2.
st-Op Day-14, the mean value 0.96 ± 0.790 was for group-1 which was non-significantly lower than the mean value 1.08 ± 0.909 was for group-2.7. The comparison of mean VAS value at different time duration within Group-1 showed statistically significant correlation (P<0.05) for Day 1 and 3 while others were non-significant. The mean value 1.40 ± 0.957 at Day 1 has reduces significantly to the mean value 0.80 ± 0.866 at Day 3.
8. For Group 2, comparison of mean VAS value at different time duration within Group-2 was statistically significant for Day 1 and Day 3 when compared with Day 14. The mean value 4.80 ± 1.633 at Day 1 has reduces significantly to the mean value 1.08 ± 0.909 at Day 14. Similarly, the mean value 5.12 ± 1.130 at Day 3 has reduces significantly to the mean value 1.08 ± 0.909 at Day 14.
Conclusion
Present study concludes that injection of methylene blue can effectively alleviate pain after various anorectal surgeries. The application can achieve a long-acting analgesic effect with minimal complications and adverse reactions. Present study thus recommends use of methylene blue as local analgesic in anorectal surgeries in all cases.
Declarations
Sponsorship
None
Conflict of Interest
Authors have no Conflict of Interest.
Source of funding
No funding required.
References
- Gardner IH, Siddharthan RV, Tsikitis VL. Benign anorectal disease: Hemorrhoids, fissures, and fistulas. Ann Gastroenterol 2020;33(1):9-18.
[Crossref] [Google Scholar] [PubMed]
- Nelson RL, Abcarian H, Davis FG, Persky V. Prevalence of benign anorectal disease in a randomly selected population. Dis Colon Rectum 1995;38: 341-344.
[Crossref] [Google Scholar] [PubMed]
- Godeberge P, Sheikh P, Zagriadskiĭ E, Lohsiriwat V, Montaño AJ, Košorok P, et al. Hemorrhoidal disease and chronic venous insufficiency: Concomitance or coincidence; results of the CHORUS study (Chronic venous and HemORrhoidal diseases evaluation and Scientific research). J Gastroenterol Hepatol 2020;35(4):577-585.
- Lohsiriwat V. Approach to hemorrhoids. Curr Gastroenterol Rep 2013;15:1-4.
[Crossref] [Google Scholar] [PubMed]
- Picciariello A, Tsarkov PV, Papagni V, Efetov S, Markaryan DR, Tulina I, et al. Classifications and clinical assessment of haemorrhoids: The proctologist’s corner. Rev Recent Clin Trials 2021;16(1):10-16.
[Crossref] [Google Scholar] [PubMed]
- Simillis C, Thoukididou SN, Slesser AA, Rasheed S, Tan E, Tekkis PP, et al. Systematic review and network meta-analysis comparing clinical outcomes and effectiveness of surgical treatments for haemorrhoids. Br J Surg 2015;102(13):1603-1618.
[Crossref] [Google Scholar] [PubMed]
- Lohsiriwat V. Hemorrhoids: From basic pathophysiology to clinical management. World J Gastroenterol 2012;18(17): 2009–2017.
[Crossref] [Google Scholar] [PubMed]
- Gallo G, Martellucci J, Sturiale AE, Clerico G, Milito G, Marino F, et al. Consensus statement of the Italian society of colorectal surgery (SICCR): management and treatment of hemorrhoidal disease. Tech Coloproctol 2020;24:145-164.
[Crossref] [Google Scholar] [PubMed]
- Lohsiriwat D, Lohsiriwat V. Outpatient hemorrhoidectomy under perianal anesthetics infiltration. J Med Assoc Thai 2005;88(12):1821.
[Crossref] [Google Scholar] [PubMed]
- Patti R, Luigi AP, Matteo A, Sergio S, Pietro R, Calogero F, et al. Botulinum toxin vs. topical glyceryl trinitrate ointment for pain control in patients undergoing hemorrhoidectomy: a randomized trial. Dis Colon Rectum 2006;49:1741-1748.
[Crossref] [Google Scholar] [PubMed]
Copyright: © 2023 The Authors. This is an open access article under the terms of the Creative Commons Attribution Non Commercial Share Alike 4.0 (https://creativecommons.org/licenses/by-nc-sa/4.0/). This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.