Research Article - Archives of Clinical and Experimental Surgery (2023)
Surgical Outcome of Takayasu Arteritis: Postoperative Cardiovascular Events Study
Hiroshi Furuhata1,2, Manabu Shiraishi1*, Kenichiro Sato1,2 and Atsushi Yamaguchi12Department of Cardiovascular Surgery, Cardiac Division, Kasukabe Chuo Medical Center, Saitama, Japan
Manabu Shiraishi, Department of Cardiovascular Surgery, Saitama Medical Center, Jichi Medical University, Saitama, Japan, Tel: +81-48-647-2111, Email: manabu@omiya.jichi.ac.jp
Received: 14-Apr-2023, Manuscript No. EJMACES-23-95922; Editor assigned: 17-Apr-2023, Pre QC No. EJMACES-23-95922 (PQ); Reviewed: 02-May-2023, QC No. EJMACES-23-95922; Revised: 09-May-2023, Manuscript No. EJMACES-23-95922 (R); Published: 17-May-2023
Abstract
Objective: Takayasu’s arteritis develops at a younger age than other vascular diseases secondary to atherosclerosis. It was associated with more reoperations and cardiovascular events in the late postoperative period. This study aimed to clarify the surgical and late postoperative outcomes of Takayasu’s arteritis.
Methods: Twenty-seven patients, who underwent surgery for Takayasu’s arteritis at the Saitama Medical Center, Jichi Medical University, between February 1996 and November 2021, were included. The patient’s ages ranged from 27 to 80 years. There were four males and 23 females. There were four patients with type I disease, ten with type II a disease, four with type II b disease, zero with type III disease, six with type IV disease, and three with type V disease. The surgical outcomes, survival rates, and late postoperative cardiovascular events were evaluated.
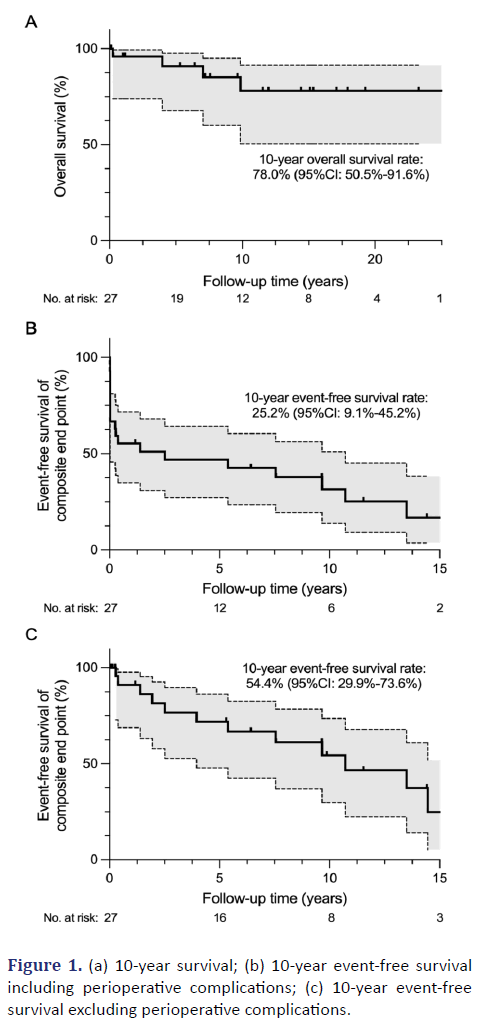
Results: Five patients underwent coronary artery bypass surgery, 16 underwent valvuloplasty and valve replacement, five underwent thoracic aortic replacement, three underwent abdominal aortic replacement, five underwent thoracic aortic replacement, three underwent abdominal aortic replacement, and six underwent peripheral arterial bypass surgery. The mean follow-up period was 9.1 ± 7.6 years. There was one inhospital death and three remote deaths. Late postoperative cardiovascular events occurred in 14 patients. In particular, there were four patients with coronary lesions requiring percutaneous coronary intervention, five with heart failure, two who suffered a stroke, one with a cerebral aneurysm, one with arrhythmia requiring ablation, and two with pacemaker implantation. The 10-year survival rate was 78.0%, while the 10-year event-free survival was 25.2%. The 10-year event-free survival, excluding perioperative complications, was 54.4%.
Conclusion: Late postoperative cardiovascular events occurred in approximately half of the patients during the follow-up period. Patients, suspected of Takayasu’s arteritis, should be monitored for the development of new vascular lesions to establish an accurate postoperative diagnosis.
Keywords
Takayasu’s Arteritis; Cardiovascular event; Survival rate; Complication
Abbreviations
AR-Aortic Regurgitation; AVRAortic Valve Replacement; CABGCoronary Artery Bypass Grafting; CAD-Coronary Artery Disease; CRPC- Reactive Protein; PAD-Peripheral Arterial Disease; PCI- Percutaneous Coronary Intervention; PMI-Pace Maker Implantation
Introduction
Takayasu arteritis is a chronic disease, characterized by nonspecific arterial inflammation. It more commonly involves young female patients. This disease causes occlusive or aneurysmal changes in vessels. It produces aortic aneurysms, Aortic Regurgitation (AR) with basal dilatation, and aortic dissection due to vascular degeneration in the major branches of the aorta, coronary arteries, and pulmonary arteries [1]. Coronary Artery Disease (CAD) develops in approximately 5-20% of patients, and ischemic heart disease is one of the leading causes of death [2]. In addition to steroid therapy, other immunosuppressive drugs and biological agents such as tumor necrosis factor-α inhibitors and anti-interleukin-6 receptor antibodies have been used to treat Takayasu arteritis. Some patients do not develop clinically problematic stenosis or dilation. Most patients respond to medication, but symptomatic patients, who are refractory to treatment, require surgical intervention to improve their prognosis [3]. Takayasu arteritis is likely to have recurrent and spontaneous remission, resulting in postoperative recurrent cardiovascular events [4]. This study investigated the early complications and late postoperative cardiovascular events among patients, who underwent surgery for Takayasu’s arteritis. Moreover, the significance of postoperative follow-up over time was determined.
Materials and Methods
Patient selection and data collection
From February 1996 to November 2021, 27 patients (four males and 23 females) with Takayasu’s arteritis (including patients who were diagnosed postoperatively) underwent surgical treatment at the Saitama Medical Center, Jichi Medical University. The mean age of the patients was 55.7 (27-80) years. Takayasu arteritis was diagnosed according to the JCS 2017 Guideline [2]. Twenty patients (74.1%) were preoperatively diagnosed with Takayasu arteritis. The clinical classification, preoperative C-Reactive Protein (CRP) levels, preoperative steroid medications, disease activity, major cardiovascular lesions, surgical treatment, early complications, and late postoperative cardiovascular events were retrospectively investigated. The mean observation period was 9 ± 7.5 years.
Statistical analysis
Continuous variables are shown as a mean ± standard deviation. Categorical variables are expressed as the number and percentage of patients. The Kaplan–Meier analysis was used to analyze the survival rate and is presented with 95% confidence intervals (95% CI). GraphPad Prism software version 9 (GraphPad Software, LLC) was used for all statistical analyses, and a p value less than or equal to 0.05 was considered significant.
Results
Preoperative steroid therapy was administered in 11 patients (40.7%). Prednisolone was administered at 12.6 ± 11.3 mg (2.5-40 mg). The preoperative CRP value was 1.86 ± 2.77 mg/d (0.01-13.6 mg/d). Concomitant diseases included AR in 12 patients (44%), Peripheral Arterial Disease (PAD) in six patients (22%), aortic aneurysm in 10 patients (37%), and CAD in five patients (19%). There were four patients with type I arteritis (14.8%), 10 with type II a arteritis (37.0%), four with type II b arteritis (14.8%), zero with type III arteritis (0%), six with type IV arteritis (22.2%), and three with type V arteritis (11.1%) (Table 1).
| Age (years) | 55.7 ± 14.8 |
|---|---|
| Sex, male, n (%) | 4 (14.8) |
| Preoperative definitive diagnosis of TAK, n (%) | 20 (74.1) |
| Classification | |
| Type I, n (%) | 4 (14.8) |
| Type IIA, n (%) | 10 (37.0) |
| Type IIB, n (%) | 4 (14.8) |
| Type III, n (%) | 0 (0.0) |
| Type IV, n (%) | 6 (22.2) |
| Type V, n (%) | 3 (11.1) |
| Preoperative CRP (mg/dL) | 1.86 ± 2.77 |
| Preoperative steroid medication, n (%) | 11 (40.7) |
| Steroid dose (mg) | 12.6 ± 11.3 |
| Preoperative clinical remission, n (%) | 5 (18.5) |
| Concomitant cardiovascular disease | |
| Coronary artery disease, n (%) | 5 (18.5) |
| Aortic valve regurgitation, n (%) | 12 (44.4) |
| Peripheral arterial disease, n (%) | 6 (22.2) |
| Aortic aneurysm, n (%) | 10 (37.0) |
Note: Mean ± SD values are shown unless otherwise indicated.
Abbreviations: TAK-Takayasu's Arteritis; CRP-C-Reactive Protein
There were four patients who underwent off-pump Coronary Artery Bypass Grafting (CABG; 15%), 13 who underwent Aortic Valve Replacement (AVR) (including aortic root reconstruction) (48.1%), three who underwent mitral valve plasty or mitral valve replacement (11.1%), five who underwent thoracic aortic replacement (18.5%), three who underwent abdominal aortic replacement (11.1%), and six who underwent peripheral arterial bypass (22.2%). There were no deaths within 30 days, but there was one in-hospital death (3.7%) due to gastrointestinal tract perforation on postoperative day 94. The postoperative hospital stay was 24.3 ± 17.7 days. Perioperative cardiovascular complications included micro cerebral infarction after aortic root reconstruction in one case (3.7%), myocardial infarction in the left anterior descending branch requiring Percutaneous Coronary Intervention (PCI) after thoracic aortic replacement in one case (3.7%), cardiac tamponade after AVR in one case (3.7%), angina pectoris requiring PCI after peripheral arterial bypass in one case (3.7%), atrial fibrillation in six cases (22.2%), arrhythmia requiring Pace Maker Implantation (PMI) after peripheral arterial bypass in one case (3.7%), and intestinal ischemia after thoracic aortic replacement in one case (3.7%) (Table 2).
| Surgical procedure | Variables |
|---|---|
| Off-pump CABG, n (%) | 5 (18.5) |
| AVR (incl. aortic root reconstruction), n (%) | 13 (48.1) |
| MVR or MVP, n (%) | 3 (11.1) |
| Thoracic aortic replacement, n (%) | 5 (18.5) |
| Abdominal aortic replacement, n (%) | 3 (11.1) |
| Peripheral arterial bypass, n (%) | 6 (22.2) |
| Postoperative hospital stay (days) | 24.3 ± 17.7 |
| 30-days mortality, n (%) | 0 (0.0) |
| In-hospital mortality, n (%) | 1 (3.7) |
| Complications | |
| Cerebral infarction, n (%) | 1 (3.7) |
| Perioperative myocardial infarction, n (%) | 1 (3.7) |
| Cardiac tamponade, n (%) | 1 (3.7) |
| Atrial fibrillation, n (%) | 6 (22.2) |
| Angina pectoris, n (%) | 1 (3.7) |
| PMI for arrhythmia, n (%) | 1 (3.7) |
| Intestinal ischemia, n (%) | 1 (3.7) |
Note: Mean ± SD values are shown unless otherwise indicated. Combined surgeries were counted separately.
Abbreviations: AVR-Aortic Valve Replacement; CABG-Coronary Artery Bypass Grafting; CAD-Coronary Artery Disease; MVP-Mitral Valve Plasty; MVR-Mitral Valve Replacement; PMI-Pace Maker Implantation
There were three late postoperative deaths (11.1%). Among these, two (7.4%) were caused by heart failure, and one (3.7%) had an unknown cause. Late postoperative cardiovascular events occurred in 14 patients (51.9%). In particular, there were four cases of CAD requiring PCI (14.8%; two after off-pump CABG and two after peripheral arterial bypass), five cases of heart failure (18.5%; two after off-pump CABG, two after AVR, and one after thoracic aortic replacement), two cases of cerebral infarction (7.4%; one after AVR and one after aortic root reconstruction), one cerebral aneurysm (3.7%; after AVR), one arrhythmia requiring ablation (3.7%; after off-pump CABG), two cases of arrhythmia requiring PMI (7.4%; one after thoracic aortic replacement and one after off-pump CABG), two cases of PAD (7.4%; one after peripheral arterial bypass and one after off-pump CABG), two cases of valvular disease (7.4%; one case of recurrent mitral valve regurgitation after mitral valve plasty and one case of aortic stenosis after abdominal aortic replacement), and two cases of aortic aneurysm (7.4%; one case of thoracic aortic aneurysm after abdominal aortic replacement and one case of abdomen aortic aneurysm after off-pump CABG) (Table 3).
| Late death, n (%) | 3 (11.1) |
|---|---|
| Heart failure, n (%) | 2 (7.4) |
| Unknown cause of death, n (%) | 1 (3.7) |
| Cardiovascular event, n (%) | 14 (51.9) |
| PCI for CAD, n (%) | 4 (14.8) |
| Heart failure, n (%) | 5 (18.5) |
| Cerebral infarction, n (%) | 2 (7.4) |
| Cerebral aneurysm, n (%) | 1 (3.7) |
| Ablation for arrhythmia, n (%) | 2 (7.4) |
| PMI for arrhythmia, n (%) | 1 (3.7) |
| Peripheral arterial disease, n (%) | 2 (7.4) |
| Valvular disease, n (%) | 2 (7.4) |
| Aneurysm, n (%) | 2 (7.4) |
Abbreviations: CAD-Coronary Artery Disease; PCI-Percutaneous Coronary Intervention; PMI-Pace Maker Implantation
Figure 1 shows the 10-year survival rate, using the Kaplan–Meier method, was 78.0% (95% CI: 50.5%- 91.6%) (Figure 1a), while the 10-year event-free survival, including perioperative complications, was 25.2% (95% CI: 9.1%-45.2%) (Figure 1b). The 10-year event-free survival, excluding perioperative complications, was 54.4% (95% CI: 29.9%-73.6%) (Figure 1c).
Discussion
Takayasu arteritis is characterized by lesions in the aorta and its major branches. Patients typically present with cardiac symptoms, such as dyspnea, palpitations, angina, myocardial infarction, heart failure, and sudden death. Approximately 10-30% of patients with Takayasu arteritis develop coronary artery stenosis [5, 6]. It also causes aortic valve dilation and AR due to persistently high vascular resistance [7, 8]. In the present study, AR was the leading cause of surgery, accounting for nearly half of all cases (44%). This was followed by aneurysms (37%) and CAD (19%). Robbs et al. reported a surgical mortality rate of 3-4% for Takayasu arteritis [3], and Kieffer et al. obtained a similar mortality rate [9]. There were no 30-day postoperative deaths in this study. However, one in-hospital death was observed. Although there were fewer perioperative deaths, compared to previous reports, this study experienced a higher frequency of perioperative cardiovascular events, such as stroke, perioperative myocardial infarction, cardiac tamponade, atrial fibrillation, angina pectoris, and arrhythmia requiring PMI.
The main cause of death from Takayasu arteritis in Japan is congestive heart failure [10]. According to a study of 94 surgical Takayasu arteritis cases by Miyata, et al., 14 of 31 patients died in the late postoperative period due to congestive heart failure [11]. In this study, two of the three late postoperative deaths were due to heart failure. Fourteen patients (51.9%) required additional treatment during the late postoperative period. Even in the late postoperative period, CAD requiring PCI, heart failure, stroke, cerebral aneurysm, arrhythmia requiring ablation, PMI, PAD, valvular disease, and aortic aneurysm were characterized as cardiovascular events requiring additional treatment. Anastomotic aneurysms were reported as serious long-term complications in previous studies [11]. Robbs, et al. indicated that aneurysmal rupture was a major cause of death [3]. There were no anastomotic aneurysms in this study, but two patients (7.4%) required additional treatment due to the development of aneurysms in the late postoperative period. Patients, who underwent surgery for heart and great vessel diseases, tended to have a higher complication rate of cardiovascular events than patients who underwent surgery for obstructive diseases. The development of cardiovascular diseases, even during the late postoperative period, among patients undergoing heart and great vessel surgery for Takayasu’s arteritis, is a concern.
Disease activity in Takayasu arteritis reportedly depended on steroid use [12]. Fields, et al. reported that reported that the rate of revision or progression of Takayasu arteritis at another site within five years was 0% in patients with quiescent disease not requiring steroids, 10% in patients with quiescent disease on steroids, 57% in patients with active disease on steroids, and 67% in patients with active disease without long-term steroids [4].
Conclusion
In this study, the rate of late postoperative cardiovascular events during the entire observation period was 30% in patients with active disease on steroids and 67% in patients with active disease not on long-term steroids. Therefore, controlling disease activity is critical for preventing reoperation and disease progression. Due to the small number of patients in this study, independent factors affecting perioperative and late postoperative cardiovascular events and survival were not identified. Further studies are required to extend the observation period and increase the number of enrolled patients.
In conclusion, among Takayasu arteritis patients undergoing cardiovascular surgery, there is a high complication rate of cardiovascular events. Therefore, careful follow-up is required.
Disclosure Statement
The authors declare there are no conflicts of interest. No external funding was obtained for the work presented here.
References
- Watanabe Y, Miyata T, Tanemoto K. Current clinical features of new patients with Takayasu arteritis observed from cross-country research in Japan: Age and sex specificity. Circulation 2015;132(18):1701-1709.
[Crossref] [Google Scholar] [Pubmed]
- Isobe M, Amano K, Arimura Y, Ishizu A, Ito S, Kaname S, et al. JCS 2017 guideline on management of vasculitis syndrome-digest version. Circ J 2020;84(2):299-359.
[Crossref] [Google Scholar] [Pubmed]
- Robbs JV, Abdool-Carrim AT, Kadwa AM. Arterial reconstruction for non-specific arteritis (Takayasu's disease): medium to long term results. Eur J Vasc Surg 1994;8(4):401-407.
[Crossref] [Google Scholar] [Pubmed]
- Fields CE, Bower TC, Cooper LT, Hoskin T, Noel AA, Panneton JM, et al. Takayasu’s arteritis: Operative results and influence of disease activity. J Vasc Surg 2006;43(1):64-71.
[Crossref] [Google Scholar] [Pubmed]
- Amano J, Suzuki A. Coronary artery involvement in Takayasu's arteritis: Collective review and guideline for surgical treatment. J Thorac Cardiovasc Surg 1991;102(4):554-560.
[Crossref] [Google Scholar] [Pubmed]
- Endo M, Tomizawa Y, Nishida H, Aomi S, Nakazawa M, Tsurumi Y, et al. Angiographic findings and surgical treatments of coronary artery involvement in Takayasu arteritis. J Thorac Cardiovasc Surg 2003;125(3):570-577.
[Crossref] [Google Scholar] [Pubmed]
- Subramanyan R, Joy J, Balakrishnan KG. Natural history of aortoarteritis (Takayasu's disease). Circulation 1989;80(3):429-437.
[Crossref] [Google Scholar] [Pubmed]
- Park YB, Hong SK, Choi KJ, Sohn DW, Oh BH, Lee MM, et al. Takayasu arteritis in Korea: Clinical and angiographic features. Heart Vessels Suppl 1992;7:55-59.
[Crossref] [Google Scholar] [Pubmed]
- Kieffer E, Piquois A, Bertal A, Blétry O, Godeau P. Reconstructive surgery of the renal arteries in Takayasu's disease. Ann Vasc Surg 1990;4(2):156-165.
[Crossref] [Google Scholar] [Pubmed]
- Numano F. Differences in clinical presentation and outcome in different countries for Takayasu's arteritis. Curr Opin Rheumatol 1997;9(1):12-15.
[Crossref] [Google Scholar] [Pubmed]
- Miyata T, Sato O, Koyama H, Shigematsu H, Tada Y. Long-term survival after surgical treatment of patients with Takayasu’s arteritis. Circulation 2003;108(12):1474-1480.
[Crossref] [Google Scholar] [Pubmed]
- Weaver FA, Kumar SR, Yellin AE, Anderson S, Hood DB, Rowe VL, et al. Renal revascularization in Takayasu arteritis–induced renal artery stenosis. J Vasc Surg 2004;39(4):749-757.
[Crossref] [Google Scholar] [Pubmed]
Copyright: © 2023 The Authors. This is an open access article under the terms of the Creative Commons Attribution Non Commercial Share Alike 4.0 (https://creativecommons.org/licenses/by-nc-sa/4.0/). This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.