Research Article - Archives of Clinical and Experimental Surgery (2022)
System Improvements for Both Elective and Emergency Cholecystectomy Patients after the Introduction of an Acute Surgical Unit
Marang Makepe1*, Yuchen Luo1, Arthur Yim1, Mark Tacey2,3, David Leigh Bird1 and Russell Hodgson42Department of Surgery, Northern Health, Epping, Australia
3Department of Research, Northern Health, Epping, Australia
4Department of Medicine, Dentistry and Health Sciences, University of Melbourne, Parkville, Australia
5Department of Surgery, University of Melbourne, Epping, Australia
Marang Makepe, Department of Surgery, Northern Health, Epping, Australia, Tel: +61433082825, Email: marang.makepe@gmail.com
Received: 08-Sep-2022, Manuscript No. EJMACES-22-74126; Editor assigned: 12-Sep-2022, Pre QC No. EJMACES-22-74126 (PQ); Reviewed: 28-Sep-2022, QC No. EJMACES-22-74126; Revised: 04-Oct-2022, Manuscript No. EJMACES-22-74126 (R); Published: 11-Oct-2022
Abstract
Objective: Gallbladder pathology represents a significant proportion of general surgical workload. Pressures of theatre access, bed availability, and an elderly, co-morbid population may be alleviated by an Acute General Surgical Unit (ASU) model. The impact on elective cholecystectomy workload is unknown.
Methods: A retrospective audit was performed between February 2012 and February 2014 on 1289 patients undergoing emergency or elective cholecystectomy at a single institution, a year either side of an ASU introduction in February 2013.
Results: 642 patients that underwent cholecystectomy in the 12 months prior to ASU implementation were compared with 647 patient’s post-ASU. Demographic data was comparable in both groups. Comparing pre-ASU to post-ASU, in-hours cases increased (82.9% vs. 86.6%, p<0.001) with more consultant involvement (29.9% vs. 39.9%, p<0.001). Wait times improved for emergency cases (<2 days 42% vs. 58%, p=0.050). Interestingly, elective wait times also improved (<90 days 23% vs. 42%, p<0.001). Patients presented to emergency prior to cholecystectomy more frequently pre-ASU (31.6% vs. 27.2%, p=0.033). Post-ASU, higher acuity patients were seen, with an increase in suspected acute cholecystitis (25.5% vs. 34.8%, p<0.001), and more common bile duct stones were found (6.4% vs. 9.1%, p=0.064). There was no significant difference in morbidity post- ASU (13.4% vs. 18.4%, p=0.17).
Conclusion: The ASU model has contributed to improvements including theatre access, increased consultant involvement and also coincided with higher patient acuity. Interestingly, improved efficiency in emergency cholecystectomy has improved wait times for elective cholecystectomy.
Keywords
Acute surgical unit; Elective surgery; Cholecystectomy; Gallstones
Introduction
The Acute Surgical Unit (ASU) model, a model for care of emergency surgical care, is now commonly used throughout Australia and New Zealand [1]. It was initially implemented in Australia in 2005 at Prince of Wales Hospital and modified in 2006 at Nepean Hospital [1]. With the traditional method of care, surgeons are on-call for the hospital but often have competing obligations and are not always onsite. Emergency surgery is completed as and when possible, often after elective work is completed, and primarily occurring after hours (1-3). The ASU model addressed many of these issues with the main principles being: a) ASU is a consultant led unit, with one consultant being on-call for the unit for 24 hours with no competing obligations and ready availability; b) the unit runs independently of elective general surgical units with its own 24-hour staff; and c) there is a dedicated ASU operating theatre.
The benefits of an ASU model are well documented for non-trauma patients presenting with common acute general surgical conditions, with reduced conversion rates and better outcomes [1]. There are also improvements in efficiency with increased in-hours operating, reduction in time from emergency to theatre with improvements in patient flow and better training opportunities for surgical trainees [2-7]. Additionally, there are economic benefits in having an ASU [2,8]. This model has been shown to be effective in common acute surgical presentations including appendicitis and small bowel obstruction [9]. It has also been demonstrated to improve several parameters including effective use of scarce theatre time especially during daylight hours, shorter hospital stays and more efficient use of limited hospital resources [2,10-12].
There is only a small body of literature that examines operative management of gallstone disease in the setting of an Australian ASU, with most of the advancements found to be improved service delivery in terms of faster time to theatre, more judicious use of investigations, faster discharge times and more in- hours operating [5,6,12-14]. There does not appear to be much, if any, decrease in operative morbidity with the only gains appearing to be economic, as well as patient and staff satisfaction5. The published improvements relate to emergency patients within the ASU only, and with resource re-allocation directed to the ASU, it seems pertinent to also examine the effects of areas where resources were taken from. There is limited available literature in this area, with any potential advantages or disadvantages to elective or non-general surgery units largely unknown.
The aim of this project was to assess outcomes for both emergency and elective patients with gallstone disease following the introduction of an ASU model.
Methodology
A retrospective audit was performed on all cholecystectomies performed between February 2012 and February 2014 (the 12 months before and after the introduction of an ASU model) at a single institution, Northern Health, Melbourne, Australia. Data was gathered and tabulated from electronic medical records. Patients who had a cholecystectomy as part of another operation (e.g. liver resection or pancreaticoduodenectomy) were excluded. Data for both elective and emergency presentations was collected. Demographic data, time to theatre, operative details as well as outcomes including morbidity, mortality were analysed. The Clavien-Dindo classification was used to classify the complications [15,16].
The Northern Health ASU is a stand-alone unit with dedicated 24-hour staff that includes consultants and fellows who are on call for 24 hours from 1830, present on site from 0730 to 1830, and have no competing obligations. The ASU is responsible for the care of acute general surgical patients referred from emergency, other medical disciplines and surgical units. For the period of the study, the unit was staffed by one accredited surgical trainee, four unaccredited surgical trainees, a resident and four interns who shared a rotating roster with staggered start times. Overnight there was one unaccredited surgical trainee on-site, with the fellow and consultant available as required. Handover was conducted twice daily with the consultant, fellow and other rostered staff present at 0730 and again at 1830 when the new consultant and fellow took over on call duties. The handovers were conducted free of distractions in a dedicated ASU office. Following the morning handover, a consultant-led round was conducted. There was a daily protected ASU operating list during business hours either all- day or half day depending on a rotating timetable. Most of this operating time was requisitioned from general surgery elective lists or emergency lists. After hours and on weekends, ASU shared a 24-hour emergency operating list with other specialities.
Descriptive statistics were prepared to test for differences between the pre and post ASU periods. Student’s t-tests or Mann-Whitney (ranksum) tests were used to test for differences in normally and non-normally distributed variables respectively. Non-normally distributed variables were presented as median and Inter-Quartile Range (IQR), while chi-squared or Fisher’s exact tests were applied for categorical variables. Stata v15.1 (StataCorp, College Station, Texas, USA) was used for the statistical analysis, with a two-sided p-value of less than 0.05 indicating statistical significance.
This study was approved by the Northern Health Ethics and Governance Office (ALR 04.2017).
Results
642 patients underwent cholecystectomy in the 12 month period prior to the implementation of the ASU (pre-ASU) and 647 in the 12 months following implementation (post-ASU). Patient demographics were comparable between the two groups with respect to age and gender (Table 1). There was a significant reduction post-ASU in number of presentations prior to definitive management, particularly in the patients requiring emergency cholecystectomy with an approximately 25% reduction in the number of patients presenting multiple times (29.1% vs. 22.0%, p=0.042). Access to imaging was assessed and compared in both periods, with ultrasound used in more than 90% of cases and with a small but significant overall increase in the post-ASU period (90.7% vs. 93.8%, p=0.037) (Table 1). Small increases in the use of MRI (5.3% to 7.3%) and CT (10.9% to 15.1%) were also noted, although only CT use confined to the emergency group was significantly increased. The number of patients with suspected cholecystitis increased significantly in the post-ASU period with a commensurate decrease in those with biliary colic.
| All Patients | Elective Patients | Emergency Patients | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Pre-ASU | Post-ASU | p value | Pre-ASU | Post-ASU | p value | Pre-ASU | Post-ASU | p value | ||
| N | 642 | 647 | 357 | 340 | 285 | 307 | ||||
| Age at admission (years), median (IQR) | 44 (34-60) | 45 (34-58) | 0.94 | 45 (35-58) | 44 (33-55) | 0.44 | 43 (32-61) | 45 (34-61) | 0.38 | |
| Gender - male | 180 (28.0) | 205 (31.7) | 0.16 | 87 (24.4) | 91 (26.8) | 0.49 | 93 (32.6) | 114 (37.1) | 0.26 | |
| Number of ED Presentations prior to index admission | 0.03 | 0.81 | 0.02 | |||||||
| 0 | 439 (68.4) | 471 (72.8) | 238 (66.7) | 232 (68.2) | 201 (70.5) | 239 (77.9) | ||||
| 1 | 144 (22.4) | 139 (21.5) | 90 (25.2) | 84 (24.7) | 54 (18.9) | 55 (17.9) | ||||
| 2 | 40 (6.2) | 32 (4.9) | 22 (6.2) | 21 (6.2) | 18 (6.3) | 11 (3.6) | ||||
| 3 | 9 (1.4) | 3 (0.5) | 3 (0.8) | 2 (0.6) | 6 (2.1) | 1 (0.3) | ||||
| 4+ | 10 (1.6) | 2 (0.3) | 4 (1.1) | 1 (0.3) | 6 (2.1) | 1 (0.3) | ||||
| Length of Stay, median (IQR) | 1 (1-4) | 1 (1-3) | 0.88 | 1 (1, 1) | 1 (1, 1) | 0.65 | 4 (2, 5) | 3 (2, 5) | 0.13 | |
| Reason for Operation | <0.001 | 0.2 | <0.001 | |||||||
| Biliary colic | 375 (58.4) | 320 (49.5) | 311 (87.1) | 284 (83.5) | 64 (22.5) | 36 (11.7) | ||||
| Suspected Cholecystitis | 164 (25.5) | 225 (34.8) | 16 (4.5) | 11 (3.2) | 148 (51.9) | 214 (69.7) | ||||
| Pancreatitis | 49 (7.6) | 41 (6.3) | 11 (3.1) | 18 (5.3) | 38 (13.3) | 23 (7.5) | ||||
| Acalculous Cholecystitis | 10 (1.6) | 8 (1.2) | 3 (0.8) | 1 (0.3) | 7 (2.5) | 7 (2.3) | ||||
| Polyps/Suspected Cancer | 13 (2.0) | 24 (3.7) | 12 (3.4) | 22 (6.5) | 1 (0.4) | 2 (0.7) | ||||
| Suspected CBD stone/cholangitis | 25 (3.9) | 29 (4.5) | 3 (0.8) | 4 (1.2) | 22 (7.8) | 25 (8.1) | ||||
| Other | 6 (0.9) | 0 (0.0) | 1 (0.3) | 0 | 5 (1.8) | 0 | ||||
| Time of Emergency Presentation | 0.12 | |||||||||
| 8:00 to 17:00 | 104 (36.5) | 132 (43.0) | ||||||||
| 17:00 to 22:00 | 59 (20.7) | 64 (20.8) | ||||||||
| 22:00 to 8:00 | 106 (37.2) | 90 (29.3) | ||||||||
| Time not recorded | 16 (5.6) | 21 (6.8) | ||||||||
| Pre-Operative imaging modality | ||||||||||
| Ultrasound | 582 (90.7) | 607 (93.8) | 0.04 | 324 (90.8) | 320 (94.1) | 0.12 | 258 (90.5) | 287 (93.5) | 0.22 | |
| CT | 70 (10.9) | 98 (15.1) | 0.03 | 34 (9.5) | 41 (12.1) | 0.33 | 36 (12.6) | 57 (18.6) | 0.06 | |
| MRI/MRCP | 34 (5.3) | 47 (7.3) | 0.17 | 14 (3.9) | 19 (5.6) | 0.37 | 20 (7.0) | 28 (9.1) | 0.37 | |
| Times between diagnostic imaging and proceeding to theatre for emergency gallstone disease patients, Median (IQR) | 2.48 (1.46-4.38) | 1.69 (1.46-3.52) | 0.01 | |||||||
| Note: ASU: Acute Surgical Unit; IQR: Inter Quartile Ratio; ED: Emergency Department; CBD: Common Bile Duct; CT: Computed Topography; MR: Magnetic Resonance Imaging; MRCP: Magnetic Resonance Cholangioc Pancreatography | ||||||||||
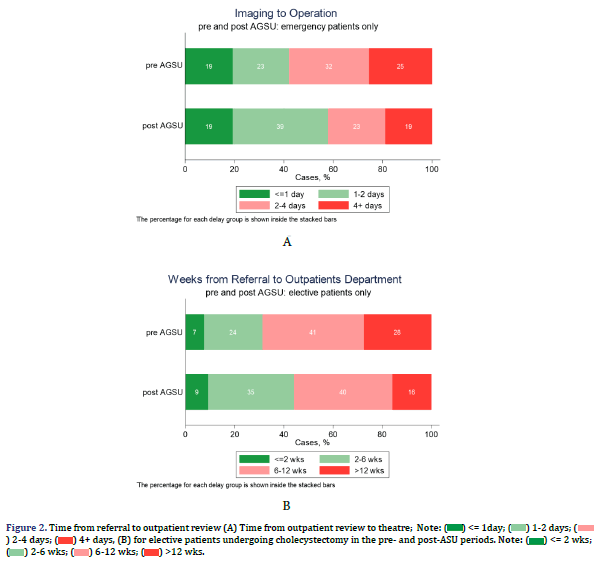
For patients who presented with gallstone disease through the emergency department there was an appreciable decrease in times between diagnostic imaging and proceeding to theatre when the two periods were compared (2.48 vs. 1.69 days, p=0.012) (Table 1). When using 2 days as a relevant clinical cut off for waiting for an emergency operation, 42% in the pre- ASU period waited less than 2 days to undergo cholecystectomy, compared with 58% of patients in the post-ASU period (Figure 1).
In the post-ASU period, there was an overall increase in the number of emergency operations being performed during business hours and a compensatory reduction in the number of operationss being performed after hours (Table 2). Operating time was slightly prolonged post-ASU compared to pre-ASU (85 minutes vs. 75 minutes, p<0.001). In the elective setting, the use of Intra Operative Cholangiography (IOC) increased from 83.2% to 91.2% (p=0.002), as well as the use of drains (23.4% to 41.3%, p<0.001), with a small increase in Common Bile Duct Exploration (CBDE) (1.1% to 3.5%) although this was not statistically significant. In the emergency setting, the use of drains also increased from 48.6% to 59.7% (p=0.007), while the use of IOC and CBDE was similar. Bile duct injuries increased from 0.0% pre-ASU to 0.6% post- ASU but this was not statistically significant.
| All Patients | Elective Patients | Emergency Patients | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Pre-ASU | Post-ASU | p value | Pre-ASU | Post-ASU | p value | Pre-ASU | Post-ASU | p value | |
| N | 642 | 647 | 357 | 340 | 285 | 307 | |||
| Time of Operation | <0.001 | 0.26 | <0.001 | ||||||
| 8:00 to 17:00 | 527 (82.9) | 559 (86.8) | 351 (98.3) | 329 (96.8) | 176 (63.1) | 230 (75.7) | |||
| 17:00 to 22:00 | 64 (10.1) | 29 (4.5) | 0 | 1 (0.3) | 64 (22.9) | 28 (9.2) | |||
| 22:00 to 8:00 | 45 (7.1) | 56 (8.7) | 6 (1.7) | 10 (2.9) | 39 (14.0) | 46 (15.1) | |||
| Operating Time (min), median (IQR) | 75 (60-97) | 85 (69-110) | <0.001 | 71 (60-89) | 76 (65-95) | <0.001 | 85 (60-115) | 93 (70-121) | 0.013 |
| ASA | 0.22 | 0.26 | 0.54 | ||||||
| 0 | 0 (0.0) | 1 (0.3) | 0 | 1 (0.5) | 0 | 0 | |||
| 1 | 145 (35.5) | 116 (30.6) | 91 (42.5) | 67 (34.9) | 54 (27.7) | 49 (26.2) | |||
| 2 | 200 (48.9) | 193 (50.9) | 100 (46.7) | 96 (50.0) | 100 (51.3) | 97 (51.9) | |||
| 3 | 54 (13.2) | 64 (16.9) | 23 (10.7) | 28 (14.6) | 31 (15.9) | 36 (19.3) | |||
| 4 | 10 (2.4) | 5 (1.3) | 0 | 0 | 10 (5.1) | 5 (2.7) | |||
| Operative Technique | |||||||||
| Access | 0.3 | 0.099 | 0.89 | ||||||
| Laparoscopic | 632 (98.4) | 629 (97.2) | 356 (99.7) | 334 (98.2) | 276 (96.8) | 295 (96.1) | |||
| Open | 4 (0.6) | 6 (0.9%) | 1 (0.3) | 2 (0.6) | 3 (1.1) | 4 (1.3) | |||
| Laparoscopic converted to Open | 6 (0.9) | 12 (1.9%) | 0 | 4 (1.2) | 6 (2.1) | 8 (2.6) | |||
| IOC | 541 (84.3) | 572 (88.4) | 0.03 | 297 (83.2) | 310 (91.2) | 0.002 | 244 (85.6) | 262 (85.3) | 0.93 |
| CBDE | 41 (6.4) | 59 (9.1) | 0.064 | 4 (1.1) | 12 (3.5) | 0.034 | 37 (13.0) | 47 (15.4) | 0.4 |
| Drain | 221 (34.6) | 322 (50.0) | <0.001 | 83 (23.4) | 140 (41.3) | <0.001 | 138 (48.6) | 182 (59.7) | 0.007 |
| Note: ASU: Acute Surgical Unit; IQR: Inter Quartile Ratio; ASA: American Society of Anaesthesiologists; IOC: Intra-Operative Cholangiography; CBDE: Common Bile Duct Exploration. | |||||||||
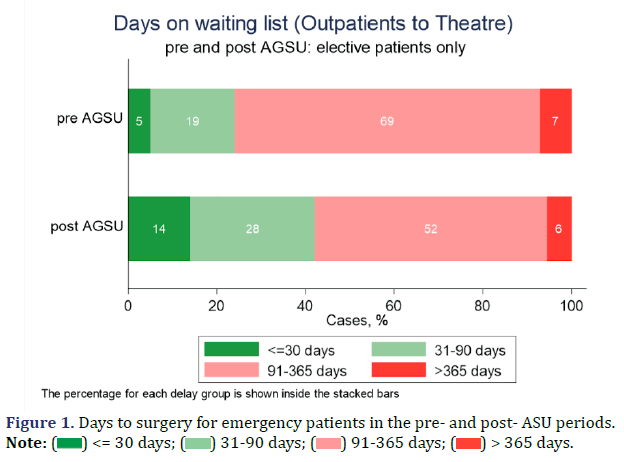
The effect of the introduction of the ASU on outpatient/ elective management of gallstone disease was explored. There was a reduction in time for referrals to be seen in outpatients in the post-ASU period, regardless of referral source. In the pre-ASU period 31% of patients were seen within 6 weeks of referral compared to 44% post-ASU (p=0.001) (Figure 2A). Prior to ASU, 76% of patients were waiting over 90 days after being placed on the waiting list which decreased significantly post-ASU with patients almost twice as likely to have their procedures within 90 days (42% vs. 24%, p<0.001) (Figure 2B).
When the two periods were compared, there was no statistical difference in complication rate between groups, or with the emergency or elective subgroups (Table 3).
| All Patients | Elective Patients | Emergency Patients | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Pre-ASU | Post-ASU | p value | Pre-ASU | Post-ASU | p value | Pre-ASU | Post-ASU | p value | |
| N | 642 | 647 | 357 | 340 | 285 | 307 | |||
| Complication Status | 0.29 | 0.52 | 0.43 | ||||||
| No complication | 578 (90.0) | 575 (88.9) | 327 (91.6) | 305 (89.7) | 251 (88.1) | 270 (87.9) | |||
| Clavien-Dindo 1 or 2 | 52 (8.1) | 51 (7.9) | 26 (7.3) | 28 (8.2) | 26 (9.1) | 23 (7.5) | |||
| Clavien-Dindo 3 or 4 | 12 (1.9) | 21 (3.3) | 4 (1.1) | 7 (2.1) | 8 (2.8) | 14 (4.6) | |||
| Specific complications: | |||||||||
| Bile Leak | 5 (0.8%) | 8 (1.2%) | 0.58 | 3 (0.8) | 4 (1.2) | 0.72 | 2 (0.7) | 4 (1.3) | 0.69 |
| Bleeding | 7 (1.1) | 5 (0.8) | 0.58 | 2 (0.6) | 3 (0.9) | 0.68 | 5 (1.8) | 2 (0.7) | 0.27 |
| Stricture | 0 (0.0) | 2 (0.3) | 0.5 | 0 | 1 (0.3) | 0.49 | 0 | 1 (0.3) | 1 |
| Re-operation/Bile Duct Injury | 8 (1.2) | 14 (2.2) | 0.28 | 4 (1.1) | 5 (1.5) | 0.75 | 4 (1.4) | 9 (2.9) | 0.27 |
|
Note: ASU: Acute Surgical Unit |
|||||||||
Discussion
Acute cholecystitis is a common general surgical problem. Internationally, it is accepted that the gold standard of care for acute cholecystitis and symptomatic gallstone disease is operative management as soon as is practicable [17-20]. System changes such as an ASU model have been developed to improve adherence to these guidelines.
Outcomes following cholecystectomy have been reviewed in the setting of an ASU with benefits including faster times to operation and median hospital stay reduced, although post-operative complications do not appear to be as significantly improved [2,8,9,12- 14,19,21]. This study of emergency cholecystectomy patients is one of the largest Australian series published to date and the results support these previous results. The major improvements appear to be related to the important area of patient flow, while the theoretical advantages of a reduction in complication rates are not statistically realised. Similar to some studies, this study has also shown that with an ASU model there is increased in-hours operating, with some evidence that this improves surgeons’ satisfaction [11,21,22]. Lower conversion rates and less readmissions may also lead to reduced hospital costs, although to our knowledge a proper economic analysis in Australian conditions has not been published [6,12,23].
Time to theatre following radiological diagnosis was also shorter (2.48 days vs. 1.69 days, p=0.012) in this study despite the volume of patients and use of imaging modalities being relatively unaltered between the two periods. In previous studies, easier access to timely radiology has been an important determinant in increased access to theatre [23]. Shakerian, et al., showed that there was reduction in use of multiple imaging modalities with the ASU model, although our data suggests, if anything, an increase in the use of radiology [13].
Currently, there is a paucity of data regarding how the institution of the ASU model affects elective surgery. Anantha, et al., found that after introduction of an ASU model, elective general surgery cases declined by 6.1%, but this had no statistical significance [24]. One could assume that by increasing resources in establishing one unit (ASU), that there would be a decrease in resources including theatre availability for other elective units; however this has not been sufficiently investigated. In the current study, the ASU has had a positive effect on the management of elective cholecystectomy patients. Patients were seen earlier in outpatient clinics with a higher number of patients seen within 2 weeks of referral and a larger proportion of patients having their cholecystectomies within 90 days. It is possible that the decrease in waiting time to be seen in outpatients was due to increased outpatient appointment availability, possibly explained by a reduction in patients referred to clinic for booking a delayed cholecystectomy after initial conservative management for acute cholecystitis. This study showed an increase in patients with acute cholecystitis as the operative indication post-ASU which could support this explanation, with more acute patients being operated on at initial presentation.
There is some evidence that a reduction in patients waiting for elective cholecystectomies after the introduction of an ASU model may relate to a reduction in the identification of new urgent elective cholecystectomies identified in clinic rather than previously identified patients awaiting delayed cholecystectomy [23]. In the current study, re-presentations to emergency also decreased post-ASU, supporting the notion that patient’s post-ASU are being treated at first presentation to the emergency department rather than being referred on to clinic with the danger of repeated attacks leading to further presentations.
Prior to ASUs, many units had adopted models whereby there was flexible space at the end of elective lists to add emergency patients. Theatre efficiency for emergency patients is known to be reduced when compared to elective patients, so it is possible that by quarantining emergency cases in their own list the result is an increased efficiency in elective lists [25]. Further studies will be required to ascertain the mechanisms in order to replicate the positive effects in other health systems.
There are further benefits to the health system in providing efficient care at first presentation. This study has shown a reduction in multiple presentations to emergency prior to emergency surgery (29.1% vs. 22.0%, p=0.048). If these findings are replicated across multiple pathologies, this would represent a significant decrease in volume for already stretched emergency departments. This has a flow on effect, reducing pathology and radiology requests, and a decrease in bed requirements. We have not, nor are we are aware of others, calculated length of stay including prior presentations for biliary symptoms; however this may be useful in justifying an ASU economically.
One of the theoretical benefits of an ASU is that there will be a decrease in complications with more timely surgical treatment of pathology, and there have been trends to this effect in other studies [4]. Similar rates of complications were observed in this study following the introduction of ASU, with no statistically significant differences observed. The non-significant increase in emergency patients with Clavien-Dindo Grade III and IV complications may be a result of an increase in co-morbid patients reflected by a greater proportion of patients having a higher ASA score, as well as more advanced pathology with a higher percentage of patients having acute cholecystitis rather than biliary colic. The increase in drain use may also reflect conservatism in surgeons who think post-operative complications are more likely in increased severity patients. A prospective study would be required to confirm these findings. This difference in patients in the post-ASU cohort may also explain the increase in operation time between the two groups. This probably reflects the success of the ASU in terms of treating sicker cholecystitis patients operatively, rather than non-operatively. However further studies looking at non-operative patients would be required to confirm this.
Conclusion
An ASU can lead to significant improvements in access to theatre in both elective and emergency patients with reduction in wait times for radiology, theatre, and a decreased length of stay. There is no statistical improvement in complication rate although this may be mitigated by the fact that ASU allows more timely access to theatre for more acute and sicker patients. There may be unforeseen improvements in access for elective patients and decreased pre-operative emergency presentations, thus improving efficiency across the health system.
Declarations
Funding
None of the authors are recipients of scholarships or grants.
Conflicts of interest
Authors have no conflicts of interest to declare.
Ethics statement
Aspects of this paper were presented as oral/poster presentations at RACS ASC 2019 and the World Society of Emergency Surgery 2020 (online).
Consent for publication
This study was a retrospective cohort study performed by reviewing de-identified medical records. It was approved by the Northern Hospital Ethics Committee and has been performed in accordance with the ethical standards of the 1964 Declaration of Helsinki. This work has not been published before, but the data has been presented at international conferences as a verbal and poster presentation. It has been approved for submission by all the co-authors and the appropriate authorities at Northern Hospital. All the figures and tables are original to this work.
References
- Nagaraja V, Eslick GD, Cox MR. The acute surgical unit model verses the traditional “on call” model: A systematic review and meta-analysis. World J Surg 2014;38(6):1381-7.
[Crossref] [Google Scholar] [Pubmed]
- Kinnear N, Britten-Jones P, Hennessey D, Lin D, Lituri D, Prasannan S, et al. Impact of an acute surgical unit on patient outcomes in South Australia. ANZ J Surg 2017;87(10):825-9.
[Crossref] [Google Scholar] [Pubmed]
- Page DE, Dooreemeah D, Thiruchelvam D. Acute surgical unit: The A ustralasian experience. ANZ J Surg 2014 ;84(1-2):25-30.
[Crossref] [Google Scholar] [Pubmed]
- Britt RC, Weireter LJ, Novosel TJ, Reed SF, Collins JN, Britt LD, et al. QS433. Initial Implementation of an Acute Care Surgery Model: Implications for Timeliness of Care. J Surg Res 2009;151(2):302.
- Pritchard N, Newbold R, Robinson K, Ooi WM. Effect of the acute general surgical unit: A regional perspective. ANZ J Surg 2017;87(7-8):595-9.
[Crossref] [Google Scholar] [Pubmed]
- Lehane CW, Jootun RN, Bennett M, Wong S, Truskett P. Does an acute care surgical model improve the management and outcome of acute cholecystitis? ANZ J Surg 2010;80(6):438-42. [Crossref]
[Google Scholar] [Pubmed]
- Chana P, Burns EM, Arora S, Darzi AW, Faiz OD. A systematic review of the impact of dedicated emergency surgical services on patient outcomes. Ann Surg 2016;263(1):20-7.
[Crossref] [Google Scholar] [Pubmed]
- Cubas RF, Gómez NR, Rodriguez S, Wanis M, Sivanandam A, Garberoglio CA, et al. Outcomes in the management of appendicitis and cholecystitis in the setting of a new acute care surgery service model: Impact on timing and cost. J Am Coll Surg 2012;215(5):715-21.
[Crossref] [Google Scholar] [Pubmed]
- Bazzi ZT, Kinnear N, Bazzi CS, Hennessey D, Henneberg M, Otto G, et al. Impact of an acute surgical unit on outcomes in acute cholecystitis. ANZ J Surg 2018;88(12):E835-9.
[Crossref] [Google Scholar] [Pubmed]
- Cox MR, Cook L, Dobson J, Lambrakis P, Ganesh S, Cregan P, et al. Acute surgical unit: A new model of care. ANZ J Surg 2010;80(6):419-24.
[Crossref] [Google Scholar] [Pubmed]
- Von Conrady D, Hamza S, Weber D, Kalani K, Epari K, Wallace M, et al. The acute surgical unit: Improving emergency care. ANZ J Surg 2010;80(12):933-6.
[Crossref] [Google Scholar] [Pubmed]
- Pepingco L, Eslick GD, Cox MR. The acute surgical unit as a novel model of care for patients presenting with acute cholecystitis. Med J Aust 2012;196(8):509-10.
[Crossref] [Google Scholar] [Pubmed]
- Shakerian R, Skandarajah A, Gorelik A, Thomson B. Emergency management of gallbladder disease: Are acute surgical units the new gold standard?. World J Surg 2015;39(11):2636-40.
[Crossref] [Google Scholar] [Pubmed]
- Suhardja TS, Bae L, Seah EZ, Cashin P, Croagh DG. Acute surgical unit safely reduces unnecessary after-hours cholecystectomy. Ann R Coll Surg Engl 2015;97(8):568-73.
[Crossref] [Google Scholar] [Pubmed]
- Dindo D, Demartines N, Clavien PA. Classification of surgical complications: A new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 2004;240(2):205-13.
[Crossref] [Google Scholar] [Pubmed]
- Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, et al. The Clavien-Dindo classification of surgical complications: Five-year experience. Ann Surg 2009;250(2):187-96.
[Crossref] [Google Scholar] [Pubmed]
- Okamoto K, Suzuki K, Takada T, Strasberg SM, Asbun HJ, Endo I, et al. Tokyo Guidelines 2018: Flowchart for the management of acute cholecystitis. J Hepatobiliary Pancreat Sci 2018;25(1):55-72.
[Crossref] [Google Scholar] [Pubmed]
- Warttig S, Ward S, Rogers G. Diagnosis and management of gallstone disease: Summary of NICE guidance. BMJ 2014;349.
[Crossref] [Google Scholar] [Pubmed]
- Lau B, Difronzo LA. An acute care surgery model improves timeliness of care and reduces hospital stay for patients with acute cholecystitis. Am Surg 2011;77(10):1318-21.
[Crossref] [Google Scholar] [Pubmed]
- Gurusamy K, Samraj K, Gluud C, Wilson E, Davidson BR. Meta-analysis of randomized controlled trials on the safety and effectiveness of early versus delayed laparoscopic cholecystectomy for acute cholecystitis. Br J Surg 2010; 97:141-50.
[Crossref] [Google Scholar] [Pubmed]
- Faryniuk AM, Hochman DJ. Effect of an acute care surgical service on the timeliness of care. Can J Surg 2013;56(3):187.
[Crossref] [Google Scholar] [Pubmed]
- Stupart DA, Watters DA, Guest GD, Cuthbert V, Ryan S. Dedicated emergency theatres improve service delivery and surgeons' job satisfaction. ANZ J Surg 2013;83(7-8):549-53.
[Crossref] [Google Scholar] [Pubmed]
- Mercer SJ, Knight JS, Toh SK, Walters AM, Sadek SA, Somers SS, et al. Implementation of a specialist-led service for the management of acute gallstone disease. Br J Surg 2004;91(4):504-8.
[Crossref] [Google Scholar] [Pubmed]
- Anantha RV, Parry N, Vogt K, Jain V, Crawford S, Leslie K, et al. Implementation of an acute care emergency surgical service: a cost analysis from the surgeon’s perspective. Can J Surg 2014;57(2):E9-14.
[Crossref] [Google Scholar] [Pubmed]
- Wallace L, Muir M, Romano L, Wyllie T, Gyomber D, Hodgson R. Assessing operating theatre efficiency: A prospective cohort study to identify intervention targets to improve efficiency. ANZ J Surg 2021;91(11):2382-8.
[Crossref] [Google Scholar] [Pubmed]
Copyright: © 2022 The Authors. This is an open access article under the terms of the Creative Commons Attribution NonCommercial ShareAlike 4.0 (https://creativecommons.org/licenses/by-nc-sa/4.0/). This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.








 ) <= 30 days; (
) <= 30 days; ( ) 31-90 days; (
) 31-90 days; ( ) 91-365 days; (
) 91-365 days; ( ) > 365 days.
) > 365 days.