Research Article - Archives of Clinical and Experimental Surgery (2023)
Urodynamic Changes in Women Subjected to Gynecological Surgeries
Luiz Henrique Carvalho Simões de Melo1,2*, Salvador Vilar Correia Lima1,2, Leslie Clifford Noronha Araújo3, Fabio de Oliveira Vilar2 and Geraldo de Aguiar Cavalcanti22Department of Urology, Hospital das Clínicas, Federal University of Pernambuco, Pernambuco, Brazil
3Department of Medicine, Catholic University of Pernambuco, Pernambuco, Brazil
Luiz Henrique Carvalho Simões de Melo, Department of Medical Sciences, Federal University of Pernambuco, Pernambuco, Brazil, Tel: +55 (081) 9.8782-2308, Email: luizsimoes99@hotmail.com
Received: 20-Oct-2023, Manuscript No. EJMACES-23-117575; Editor assigned: 23-Oct-2023, Pre QC No. EJMACES-23-117575 (PQ); Reviewed: 07-Nov-2023, QC No. EJMACES-23-117575; Revised: 14-Nov-2023, Manuscript No. EJMACES-23-117575 (R); Published: 21-Nov-2023
Abstract
Introduction: Disorders inherent to aging are increasingly present, with voiding dysfunctions and greater submission to surgeries among them.
Objective: To analyze the influence of gynecological surgeries (HT: Hysterectomy and CPP: Colpoperineoplasty) on urodynamic bladder function parameters of adult women.
Methods: A comparative study of urodynamic data from 706 patients was performed at the Urology Service of HC/UFPE (Hospital das Clínicas, Federal University of Pernambuc). Previously, patients with any known clinical factor which could affect bladder function were excluded. These patients were analyzed in groups according to their history of gynecological surgery and age group (Non-elderly/elderly). The control group was composed by women without any gynecological surgery history.
Results: All urodynamic parameters were worse in the elderly subgroup. The fundamental difference between the groups consisted of senility and past gynecological surgeries (higher in the elderly group). In the general female population, a history of gynecological surgeries was related to several alterations in urodynamic parameters. All urodynamic micturition phase parameters were significantly worse in patients with colpoplasty history. Hysterectomy history was also associated to a deterioration in some micturition parameters. However, no relationship between gynecological surgeries and urodynamic changes was found in the elderly women subgroup.
Conclusion: Gynecological surgeries (HT/CPP) do not alter the prevalence and/or intensity of voiding dysfunctions already expected in the older age group of women from the aging process itself. Functional changes in the lower urinary tract resulting from aging are imposed in elderly women, regardless of their gynecological surgery history.
Keywords
Aging; Elderly; Urodynamics; Bladder disorder; Gynecological surgeries
Abbreviations
BCI: Bladder Contractility Index; BOO: Bladder Outlet Obstruction; BVE: Bladder Voiding Efficiency; MCC: Maximum Cystometric Capacity; CPP: Colpoperineoplasty/Colpoplasty; HC/UFPE: Hospital of the Federal University of Pernambuco; HT: Hysterectomy; ICS: International Continence Society; IUC: Involuntary Uninhibited Contraction; Pabd: Abdominal pressure; Pbla: Bladder pressure; Pdet: Detrusor pressure; PdetQmax: Detrusor pressure at maximum flow; POP: Pelvic Organ Prolapse; PVR: Post Voiding Residue; Qmax: Maximum flow; SUI: Stress Urinary Incontinence; UDS: Urodynamic Study; UUI: Urge Urinary Incontinence.Introduction
It is well known that there is an absolute and relative population growth in the number of elderly and consequently the disorders inherent to the elderly age group become increasingly common in medical practice. Therefore, it is important to study the main biases related to aging, including voiding dysfunctions due to senility itself and also due to submission to surgical procedures; a fact which is increasingly prevalent in the elderly age group.
Few studies have evaluated the effects of age on female bladder function. Some studies indicate that there is a significant increase in detrusor hypocontractility prevalence related to aging. Senility would be associated with muscle wasting and a general decline in muscle contractile function, leading to hypocontractility of the detrusor muscle which tends to trigger subjective, non-specific and non-pathognomonic symptoms, including being confused with complaints of Bladder Outlet Obstruction (BOO) and other dysfunctions [1-4].
In a recent systematic review with meta-analysis aiming to identify reference values for normal bladder function parameters, Wyman et al. concluded by pointing out that future research is necessary to determine what would be normal within specific groups, such as in different age groups [5].
There are also differences in the medical literature regarding the influence of gynecological surgeries (CPP/ HT) on bladder function. The exact incidence of Lower Urinary Tract Dysfunction (LUTD) after gynecological surgery is controversial. Most of the research has been developed based on clinical complaints and symptomatological interrogations, without studying urodynamics. However, the clinical diagnosis of LUTD is difficult and inaccurate as there is a mix of signs and symptoms which can be confused. Therefore, the best way to reliably diagnose LUTD after gynecological surgeries is with Uro Dynamic Studies (UDS), and therefore the importance of researching urodynamic changes in women undergoing gynecological surgeries is apparent [6-12]. In view of the above and the scarce and conflicting literature, we realize the importance of carrying out this study in order to better analyze possible urodynamic changes in bladder function resulting from gynecological surgeries (HT and/or CPP) in young patients and also in elderly patients, in whom bladder dysfunctions are already expected by aging itself.
Patients and Methods
A total of 1,147 urodynamic reports (Anamnesis/UDS) of adult women (>18 years old) were analyzed at the Urology service of the Hospital das Clínicas, Universidade Federal de Pernambuco (HC/UFPE). Adult women who underwent urodynamic study for different clinical indications, including those already submitted to gynecological surgeries, were included in the study. Patients with any known clinical factor which could affect bladder function were excluded from the study, such as: 139-Diabetes mellitus; 61-diseases or previous neurological surgeries/spinal cord trauma or spine malformation; 12-Sling, anti-urinary incontinence surgeries; 9-Urinary tract malformation; 7-Previous pelvic radiotherapy; 108-Use of medications which act on the bladder function-anticholinergics, alpha-blockers, antidepressants; 63-Pelvic organ prolapse; 10-Relevant urinary losses, large volume or continuous during cystometry, by non-inhibited involuntary contractions or low compliance or by little efforts, such as speaking only. After review, 32 incomplete urodynamic reports were also excluded.
All research patients were submitted to an Urodynamic Study (UDS) using the examination technique based on the recommendations of “Good Urodynamic Practices” of the International Continence Society (ICS-2002).
All patients had negative urine culture for the UDS. A detailed anamnesis was performed before the exam in order to determine the main complaint and discuss conditions which could influence the bladder function (diabetes mellitus, neurological diseases, previous surgeries, radiotherapy, medications). This pre-UDS anamnesis is part of the medical report on urodynamics and the patient’s response regarding the discussion of this anamnesis is what guided their exclusion or not in the study. The exams were stored in the electronic medical record online at www.infomed.net.br, where the data was collected from. The UDS encompassed three phases: Free urofluxometry, cystometry and flow-pressure study.
Bladder function can be assessed with the data obtained by the urodynamic study using isolated data such as:
• Maximum Cystometric Capacity (MCC)
• Bladder compliance
• Presence of Uninhibited Involuntary Contractions(UICs), associated or not to urinary losses
• Presence of urinary losses associated with effortmaneuvers
• Voiding volume
• Maximum flow (Qmax)
• Detrusor pressure at maximum flow (PdetQmax)
• Post-Voiding Residue (PVR); and also through formulas developed to have greater accuracy in determining bladder dysfunctions. Among these thereare some formulas [13-15].
Formulas
• Bladder Contractility Index (BCI): PdetQmax+ (5× Qmax).Strong contractility (BCI>150), normal (BCI between 100 and 150) and weak (BCI<100).
• Bladder Voiding Efficiency (BVE): (Voiding volume/Bladder capacity) × 100.
• Detrusor hypocontractility parameters: PdetQmax<30 cm H2O and Qmax<12 ml/sec.
• Bladder outlet obstruction parameters: PdetQmax>20 cm H2O and Qmax<12 ml/sec.
Finally, a comparative study of bladder function (assessed by urodynamic parameters) was carried out with 706 adult women, 185 (26.2%) of whom were elderly (≥ 60 years old). The patients were divided into groups according to their surgical status regarding their past submission or not to gynecological surgeries (HT and/or CPP) and also according to the age group (non-elderly: 18 to 59 years old; and elderly: ≥ 60 years old). The control group was composed of non-operated women, meaning without a surgical history of gyneco logical surgeries (HT and/or CPP).
Excel 2019 software and STATA/SE 12.0 were used for statistical calculations. The maximum acceptable probability of error for rejection of the null hypothesis in all situations was 5% (p-value<0.05)
This study was submitted to the Ethics and Research Committee (CEP) of the Health Sciences Center at UFPE under CAAE no. 73321617.4.0000.5208 and was approved under the opinion no. 2.288.550.
Results
The minimum perceived age among the 706 patients was 18 years and the maximum age was 89 years, with an average age of 50.4 years. The elderly group (≥ 60 years old) consisted of 185 women (26.2%) aged between 60 and 89 years old, with an average age of 69.3 years old.
The submission frequency to gynecological surgery (CPP and/or HT) was only 28% in the younger group (18 to 59 years old), while more than half of the patients (56.8%) had already underwent gynecological surgery in the elderly group, with colpoplasty being more frequent than hysterectomy.
All urodynamic parameters were found to be worse in the elderly subgroup. For example, the detrusor hyperactivity frequency found in the population of women between 18 and 59 years old was 18% with just over a third (38%) of these cases showing urinary losses (urge urinary incontinence/wet overactive bladder), while the detrusor hyperactivity incidence in the elderly subgroup was 21.6%, with 80% of these cases showing urinary losses. The descriptive data and urodynamic parameters of these groups can be seen in Tables (1A-1C), (2A-2C) and (3A-3C).
| All 706 patients | Age | Age groups | Gynecological surgery (CPP and/or HT) | CPP | HT |
|---|---|---|---|---|---|
| N valid | 706 | - | Yes: 251 (35.6%) | Yes: 152 (21.5%) | Yes: 144 (20.4%) |
| N missing | 0 | - | No: 455 (64.4%) | No: 554 (78.5%) | No: 562 (79.6%) |
| Mean | 50.48 | - | - | - | - |
| Median | 49 | - | - | - | - |
| Std. deviation | 13.91 | - | - | - | - |
| Minimum | 18 | <60 years: 521 (73.8%) | - | - | |
| Maximum | 89 | ≥ 60 years: 185 (26.2%) | - | - | - |
| All 706 patients | MCC (ml) | Bladder compliance | Voiding volume (ml) | Maximum flow (ml/sec) | Pdet Qmax (cmH2O) | PVR (ml) (Pdet Qmax+5 × Qmax) | BCI | BVE (voiding vol./MCC) × 100% |
|---|---|---|---|---|---|---|---|---|
| N valid | 706 | 706 | 706 | 706 | 706 | 706 | 706 | 706 |
| N missing | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Mean | 401.84 | 82.08 | 366.06 | 25.83 | 29.64 | 32.9 | 158.79 | 89.42 |
| Median | 385 | 51.25 | 354 | 24 | 27.7 | 0 | 151.5 | 100 |
| Std. deviation | 129.22 | 90.62 | 153.62 | 12.24 | 16.01 | 65.94 | 60.71 | 19.05 |
| Minimum | 106 | 1.4 | 0 | 0 | 0 | 0 | 0 | 0 |
| Maximum | 941 | 695 | 941 | 75 | 128 | 525 | 418.5 | 100 |
| All 706 patients | Involuntary uninhibited contraction (IUC- detrusor hyperactivity) | Losses from IUC (UUI) | Detrusor loss pressure from UUI (cmH2O) | Loss volume from UUI (ml) | Losses from efforts (SUI) | Effort loss pressure from SUI (cmH2O) | Loss volume from SUI (ml) | BOO: Pdet Qmax>20 cmH2O and Qmax<12 ml/sec | Detrusor hypocontractility: Pdet Qmax<30 cmH2O and Qmax<12 ml/sec | BCI categorized: weak (<100) normal (100-150) strong (>150) |
|---|---|---|---|---|---|---|---|---|---|---|
| N valid | 706 | 706 | 706 | 706 | 706 | 706 | 706 | 706 | 706 | 706 |
| N missing | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Yes | 136 (19.3%) | 69 (9.8%/50.7%) | - | - | 146 (20.7%) | - | - | 52 (7.4%) | 32 (4.5%) | Weak: 113 (16%) |
| No | 570 (80.7%) | 637 (90.2%) | - | - | 560 (79.3%) | - | - | 654 (92.6%) | 674 (95.5%) | Normal: 233 (33%) |
| Mean | - | - | 38.27 | 46.71 | - | 85.21 | 20.33 | - | - | Strong: 360 (51%) |
| Median | - | - | 32.5 | 32 | - | 90 | 9 | - | - | - |
| Std. deviation | - | - | 21.02 | 42.07 | - | 33.5 | 26.15 | - | - | - |
| Minimum | - | - | 1 | 1 | - | 20 | 1 | - | - | - |
| Maximum | - | - | 140 | 200 | - | 180 | 150 | - | - | - |
| 521 non-elderly patients (<60 y) | Age | Gynecological surgery (CPP and/or HT) | CPP | HT |
|---|---|---|---|---|
| N valid | 521 | Yes: 146 (28%) | Yes: 81 (15.5%) | Yes: 87 (16.7%) |
| N missing | 0 | No: 375 (72%) | No: 440 (84.5%) | No: 434 (83.3%) |
| Mean | 43.8 | - | - | - |
| Median | 45 | - | - | - |
| Std. deviation | 8.54 | - | - | - |
| Minimum | 18 | - | - | - |
| Maximum | 59 | - | - | - |
| 521 non-elderly patients (<60y) | MCC (ml) | Bladder compliance | Voiding volume (ml) | Maximum flow (ml/sec) | Pdet Qmax (cmH2O) | PVR (ml) | BCI (PdetQmax+5 × Qmax) | BVE (voiding vol/MCC) × 100% |
|---|---|---|---|---|---|---|---|---|
| N valid | 521 | 521 | 521 | 521 | 521 | 521 | 521 | 521 |
| N missing | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Mean | 416.38 | 84.45 | 387.37 | 27.48 | 31.02 | 27.11 | 168.4 | 91.728 |
| Median | 397 | 52.8 | 371 | 25.8 | 29 | 0 | 161.3 | 100 |
| Std. deviation | 129.21 | 90.12 | 150.44 | 12.31 | 16.08 | 61.5 | 60.01 | 17.0719 |
| Minimum | 125 | 2.7 | 0 | 0 | 0 | 0 | 0 | 0 |
| Maximum | 940 | 658 | 922 | 75 | 128 | 525 | 418.5 | 100 |
| 521 non-elderly patients (<60y) | Involuntary uninhibited contraction (IUC-detrusor hyperactivity) | Losses from IUC (UUI) | Detrusor loss pressure from UUI (cm H2O) | Loss volume from UUI (ml) | Losses from efforts (SUI) | Effort loss pressure from SUI (cmH2O) | Loss volume from SUI (ml) | BOO: Pdet Qmax>20 cmH2O and Qmax<12ml/sec | Detrusor Hypocontractility: Pdet Qmax< 30 cmH2O and Qmax<12 ml/sec | BCI categorized: weak (<100) normal (100-150) strong (>150) |
|---|---|---|---|---|---|---|---|---|---|---|
| N valid | 521 | 521 | 521 | 521 | 521 | 521 | 521 | 521 | 521 | 521 |
| N missing | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Yes | 96 (18.4%) | 37 (7.1%/38.5%) | - | - | 101 (19.4%) | - | - | 27 (5.2%) | 11 (2.1%) | Weak: 55 (10.6%) |
| No | 425 (81.6%) | 484 (92.9%) | - | - | 420 (80.6%) | - | - | 494 (94.8%) | 510 (97.9%) | Normal: 166 (31.9%) |
| Mean | - | - | 37.18 | 41.22 | - | 86.68 | 19.38 | - | - | Strong: 300 (57.6%) |
| Median | - | - | 34 | 31 | - | 90 | 8 | - | - | - |
| Std. deviation | - | - | 15.97 | 40.38 | - | 32.94 | 24.1 | - | - | - |
| Minimum | - | - | 1 | 2 | - | 20 | 1 | - | - | - |
| Maximum | - | - | 77 | 200 | - | 180 | 130 | - | - | - |
| 185 elderly patients (≥ 60 y) | Age | Gynecological surgery (CPP and/or HT) | CPP | HT |
|---|---|---|---|---|
| N valid | 185 | Yes: 105 (56.8%) | Yes: 71 (38.4%) | Yes: 57 (30.8%) |
| N missing | 0 | No: 80 (43.2%) | No: 114 (61.6%) | No: 128 (69.2%) |
| Mean | 69.29 | - | - | - |
| Median | 67 | - | - | - |
| Std. deviation | 7.29 | - | - | - |
| Minimum | 60 | - | - | - |
| Maximum | 89 | - | - | - |
| 185 elderly patients(≥ 60 y) | MCC (ml) | Bladder compliance | Voiding volume (ml) | Maximum flow (ml/sec) | Pdet Qmax(cmH2O) | PVR (ml) | BCI (PdetQmax+5 × Qmax) | BVE (voiding vol/MCC) × 100% |
|---|---|---|---|---|---|---|---|---|
| N valid | 185 | 185 | 185 | 185 | 185 | 185 | 185 | 185 |
| missing | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Mean | 360.89 | 75.41 | 306.04 | 21.19 | 25.76 | 49.19 | 131.72 | 82.93 |
| Median | 338 | 48.4 | 306 | 20 | 23.8 | 14 | 125 | 93.21 |
| Std. deviation | 120.45 | 91.93 | 146.8 | 10.82 | 15.21 | 74.88 | 54.26 | 22.56 |
| Minimum | 106 | 1.4 | 47 | 3 | 1 | 0 | 17 | 14.5 |
| Maximum | 941 | 695 | 941 | 64 | 108 | 430 | 338.1 | 100 |
| 185 elderly patients (≥ 60 y) | Involuntaryuninhibited contraction (IUC-detrusor hyperactivity) | Losses fromIUC (UUI) | Detrusor losspressure from UUI (cmH2O) | Loss volumefrom UUI (ml) | Losses fromefforts (SUI) | Effort losspressure from SUI (cmH2O) | Loss volumefrom SUI (ml) | BOO: PdetQmax>20 cmH2O and Qmax<12ml/sec | Detrusor hypocontractility:Pdet Qmax<30 cmH2O and Qmax<12 ml/sec | BCIcategorized: weak (<100) normal (100-150) strong(>150) |
|---|---|---|---|---|---|---|---|---|---|---|
| N valid | 185 | 185 | 185 | 185 | 185 | 185 | 185 | 185 | 185 | 185 |
| N missing | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Yes | 40 (21.6%) | 32 (17.3%/80%) | - | - | 45 (24.3%) | - | - | 25 (13.5%) | 21 (11.4%) | Weak: 58 (31.4%) |
| No | 145 (78.4%) | 153 (82.7%) | - | - | 140 (75.7%) | - | - | 160 (86.5%) | 164 (88.6%) | Normal: 67 (36.2%) |
| Mean | - | - | 39.56 | 53.06 | - | 81.84 | 22.47 | - | - | Strong: 60 (32.4%) |
| Median | - | - | 30.50 | 44.00 | - | 80.00 | 13.00 | - | - | - |
| Std. deviation | - | - | 26.00 | 43.72 | - | 34.90 | 28.79 | - | - | - |
| Minimum | - | - | 10 | 1 | - | 20 | 1 | - | - | - |
| Maximum | - | - | 140 | 150 | - | 140 | 180 | - | - | - |
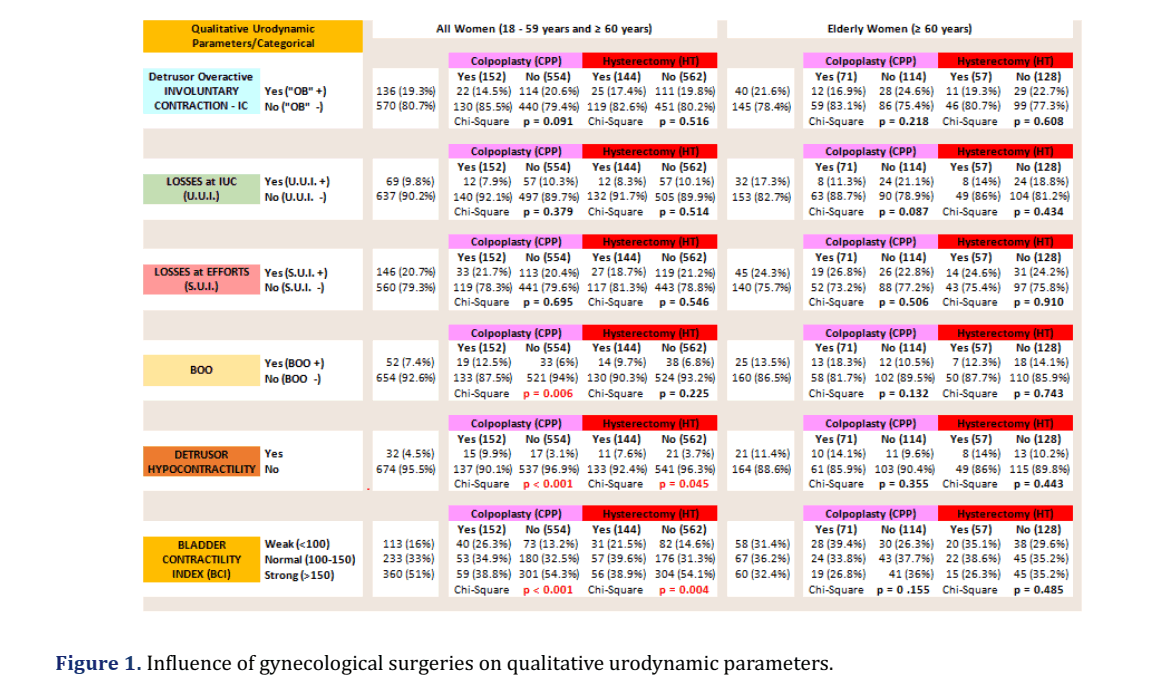
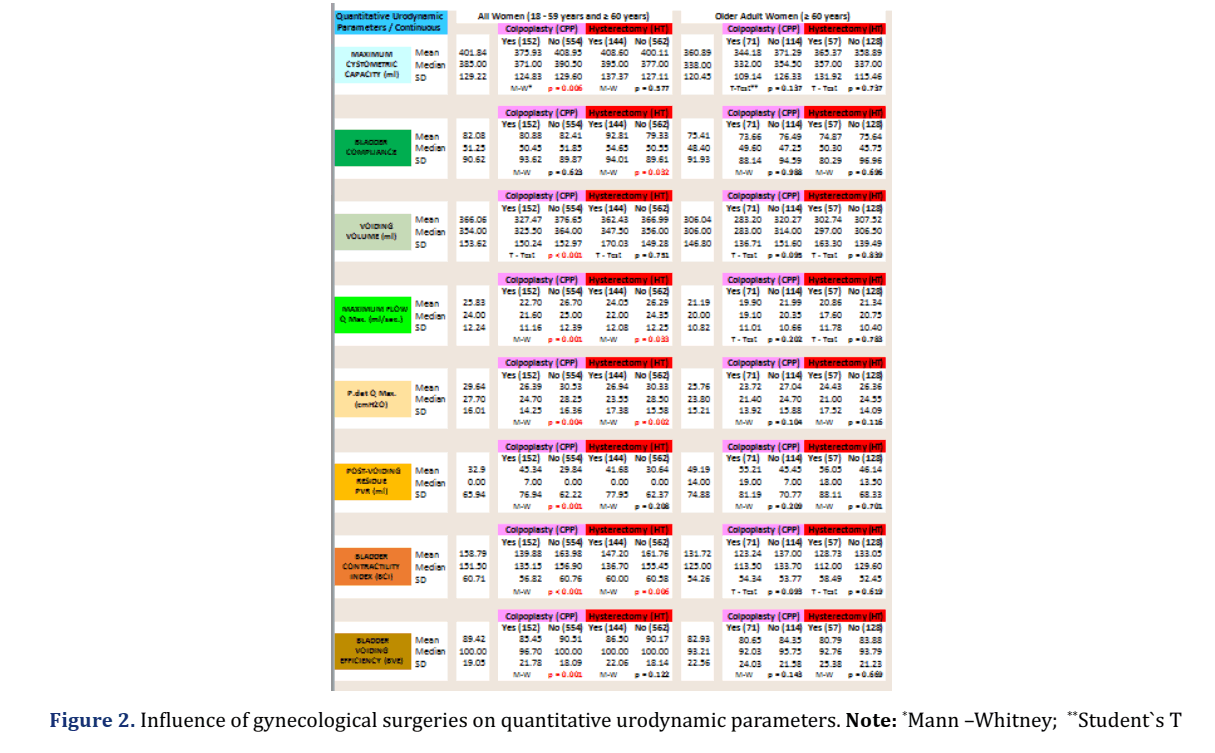
Since the difference perceived between the age groups of the study is primarily related to senility and the submission frequency to gynecological surgeries (greater in the elderly group), we analyzed the data regardingthe influence of gynecological surgeries on bladder function using urodynamic parameters detailed in Figures 1 and 2.
In the general group of adult women (18 to 89 years old), the previous history of gynecological surgeries was not associated with changes in the detrusor hyperactivity prevalence, nor in the prevalence of urinary losses in cystometry, whether UUI or SUI. However, a relevant association with worse voiding parameters was noted. All of the voiding phase parameters of the UDS (Flow × Pressure study) were significantly worse in patients with a past colpoplasty. Still regarding this general group of all patients, those with a preserved uterus (not submitted to hysterectomy) had better urination parameters.
In the analysis of the subgroup of elderly women (60 to 89 years), neither CCP nor HT history were associated with any change in the studied urodynamic parameters (detrusor hyperactivity, urge urinary incontinence, stress urinary incontinence, bladder outlet obstruction, detrusor hypocontractility, maximum cystometric capacity, bladder compliance, voiding volume, maximum flow, detrusor pressure at maximum flow, post-voiding residue, bladder contractility index, bladder voiding efficiency index).
Discussion
It is important to highlight the use of urodynamic parameters as the only objective and realistic definers of bladder dysfunctions, since reporting symptoms without urodynamic confirmation is something very relative and that is why indications for surgical treatment should not only be based on subjective complaints without urodynamic confirmation. The dissociation between reported symptoms and confirmatory urodynamic parameters has been noticed by different authors [16-17].
In our study, it was noticed that there was no change in the detrusor hyperactivity prevalence, nor in the prevalence of urinary losses in cystometry, whether UUI or SUI, among patients who underwent (or not) hysterectomy and/or colpoplasty, in both the general group of all women as well as in the subgroup of elderly women, corroborating the knowledge that colpoplasty is a failure as an option for surgically treating SUI [18-20].
In our analysis of the general group of all adult women, it can be seen that there were proportionally more patients with past gynecological surgery (both colpoplasty and hysterectomy) among the cases of detrusor hypocontractility/weak BCI. This statistically significant finding was not evidenced in the analysis of the subgroup of elderly women.
Women aged 18 to 89 years who underwent colpoplasty had worse urinary parameters. All voiding phase parameters of the UDS (Flow × Pressure study) were worse in these patients with a past colpoplasty. One of the possible explanations for this is the damage to vascularization, innervation and detrusor musculature which can occur in the dissection inherent to surgical corrections of genital prolapses. Thus, patients operated on for colpoplasty may present compromised musculature and detrusor muscle innervation and then worse urodynamic parameters in urination. Still regarding this general group of women, those who had their uterus preserved (without a past surgical hysterectomy) had some better urination parameters than patients who underwent hysterectomy, probably because their musculature and detrusor innervation were more preserved without the damage caused by dissection of a hysterectomy, such as iatrogenic denervations and/or changes in anatomy which cause loss of vesicourethral support [6-12].
There is no consensus in the medical literature on the relationship between prolapsed compartment, prolapse stage, symptoms and urodynamic findings. Some studies have shown that bladder outlet obstruction is frequent in women with severe genital prolapses and that surgical repair of these prolapses can lead to an improvement in obstructive complaints and urodynamic findings [21-23]. However, other studies indicate that no significant change in the urodynamic findings of bladder dysfunction is noticed even after Pelvic Organ Prolapse (POP) surgery and that unsatisfactory results after surgical repair of POP can be seen in patients with impaired detrusor contractility, which can result from the aging of patients and/or from a persistent longterm obstructive status period, as occurs in women with accentuated POP for many years. Thus, the simple anatomical correction of the prolapse would no longer be able to improve the symptoms or the urodynamic changes [24-27]. Dietz-Itza et al. indicated that bladder dysfunction symptoms may remain even after surgical treatment of POP due to causes such as tissue ischemia and other changes produced by aging and even the appearance of new symptoms may occur in 20% of women undergoing surgeries to correct POP [28].
In our study, unlike the general population of women aged 18 to 89 years, in which colpoplasty and/or hysterectomy surgical past showed an association with several changes in urodynamic parameters, in the analysis of the elderly women subgroup (60 to 89 years), the past gynecological surgeries were not shown to be associated with any changes in the studied urodynamic parameters.
One explanation for this would be the fact that these gynecological surgeries can lead to functional impairment of the detrusor muscle, possibly due to damage to the innervation and/or detrusor musculature which occurs during the dissection inherent in these surgeries (surgical correction of genital prolapses/hysterectomy). However, this tends to show itself in a more symptomatic and evident way in young women, since elderly women are already subject to present deficits in innervation and/or detrusor musculature resulting from their senility, causing the functional changes of the lower urinary tract due to aging to impose themselves regardless of the gynecological surgery history.
All of this exposed, allows us to question whether the influence of gynecological surgeries on bladder function would not happen in women operated on at an older age, when bladder dysfunctions tend to be already installed by the natural aging process itself and/ or whether there is a decrease in the influence of gynecological surgeries on bladder function as women get older and the bladder dysfunctions of senility gradually install themselves.
It has been found that clinical morbidities related to aging, including impaired bladder function, tend to adversely affect the management and outcomes of elderly women with POP. Aging is associated with increased detrusor hyperactivity incidence and a large number of elderly women have urgent urinary incontinence. On the other hand, aging is also associated with detrusor hypocontractility and therefore impaired bladder emptying. These factors, accompanied by reduced adherence to conservative therapies, negatively affect the outcomes of gynecological surgeries in elderly patients [29-30].
It is important to highlight the fact that the elderly population has greater surgical risks and that the indication for a surgical procedure must always go through the “balance” of risk × benefit. The benefits must outweigh the risks. Therefore, we are faced with a difficult equation -an indication of surgeries with uncertain benefits in an elderly population at higher surgical risk. However, the management, procedures and surgical techniques adopted in current medical practice for elderly women with POP have been the same as those used in young women. This situation needs to be reviewed. There should be greater consideration in indicating gynecological surgeries in elderly women solely due to subjective complaints of bladder function, without evidence of significant genital prolapse which is provoking bladder outlet obstruction confirmed by urodynamic study. This perception should guide preoperative counseling in elderly women with genital prolapse. More studies should be done to shed light on the influence of gynecological surgeries, particularly in elderly women.
The main limitations of this study were restricted to the study design which was retrospective, and to the fact that we do not have information to analyze possible differences of other variables between the groups such as parity, Body Mass Index (BMI), prolapse degree and surgical technique employed.
Conclusion
The gynecological surgeries (HT/CPP) are associated with bladder dysfunctions in the general population of women, in which worse voiding urodynamic parameters were perceived among women with a past history of gynecological surgeries (HT/CPP).
However, in the elderly women subgroup, these gynecological surgeries do not alter the prevalence and/or intensity of urodynamic voiding dysfunction already expected in this age group, due to the aging process itself. Among elderly women, functional changes in the lower urinary tract resulting from aging occur regardless of past gynecological surgery. This evidence should guide the preoperative counseling of elderly women.
Declarations
Author contributions
All authors have contributed to the information and material submitted for publication and all authors have read and approved the manuscript.
Conflict of interest
The authors have no conflict of interest.
Funding
The authors have no direct or indirect commercial financial incentive associated with publishing the manuscript and we did not receive any source of extra-institutional funding.
Institutional review board approval
This study was reviewed and approved by a certified Ethical Committee. The number of the approval document was 2.288.550 in 21/09/2017.
Ethical statement
We declare that all material in this assignment is our own work and does not constitute plagiarism. The authors allow reproduction in both print and electronic formats for worldwide distribution.
References
- Jeong SJ, Lee JK, Kim KM, Kook H, Cho SY, Oh SJ. How do we diagnose detrusor underactivity? Comparison of diagnostic criteria based on an urodynamic measure. Investig Clin Urol 2017;58(4):247-254.
- Zimmern P, Litman HJ, Nager CW, Lemack GE, Richter HE, Sirls L, et al. Effect of aging on storage and voiding function in women with stress predominant urinary incontinence. J Urol 2014;192(2):464-468.
[Crossref] [Google Scholar] [Pubmed]
- Rosier PF, Ten DCS, de Kort LM. Clinical epidemiology: Detrusor voiding contraction maximum power, related to ageing. Urology 2019;124:72-77.
[Crossref] [Google Scholar] [Pubmed]
- Neto MCA, Araujo LCN, Junior TDPB, Amaro JL, Pinto FCM, Vilar FO, et al. The aging bladder in females evaluated by urodynamics. Open J Urol 2017;7(3):54-64.
- Wyman JF, Zhou J, LaCoursiere DY, Markland AD, Mueller ER, Simon L, et al. Normative noninvasive bladder function measurements in healthy women: A systematic review and meta‐analysis. Neurourol Urodyn 2020;39(2):507-522.
[Crossref] [Google Scholar] [Pubmed]
- Abdullah B, Nomura J, Moriyama S, Huang T, Tokiwa S, Togo M. Clinical and urodynamic assessment in patients with pelvic organ prolapse before and after laparoscopic sacrocolpopexy. Int Urogynecol J 2017;28(10):1543-1549.
[Crossref] [Google Scholar] [Pubmed]
- Lo TS, Shailaja N, Hsieh WC, Uy-Patrimonio MC, Yusoff FM, Ibrahim R, et al. Predictors of voiding dysfunction following extensive vaginal pelvic reconstructive surgery. Int Urogynecol J 2017;28:575-582.
[Crossref] [Google Scholar] [Pubmed]
- Frigerio M, Manodoro S, Cola A, Palmieri S, Spelzini F, Milani R, et al. Risk factors for persistent, de novo and overall overactive bladder syndrome after surgical prolapse repair. Eur J Obstet Gynecol Reprod Biol 2019;233:141-145.
[Crossref] [Google Scholar] [Pubmed]
- Zhang L, Zhu L, Liang S, Xu T, Lang J. Short-term effects on voiding function after mesh-related surgical repair of advanced pelvic organ prolapse. Menopause 2015;22(9):993-999.
[Crossref] [Google Scholar] [Pubmed]
- Atallah D, Kassis N, Ghanameh W, Moukarzel M. Urinary functional complications following radical uterine surgery. J Med Liban 2014;62(3):156-167.
- Kruppa J, Kavvadias T, Amann S, Baessler K, Schuessler B. Short and long-term urodynamic and quality of life assessment after nerve sparing radical hysterectomy: A prospective pilot study. Eur J Obstet Gynecol Reprod Biol 2016;201:131-134.
[Crossref] [Google Scholar] [Pubmed]
- Li L, Ma S, Tan X, Zhong S, Wu M. The urodynamics and survival outcomes of different methods of dissecting the inferior hypogastric plexus in laparoscopic nerve-sparing radical hysterectomy of type C: A randomized controlled study. Ann Surg Oncol 2019;26:1560-1568.
[Crossref] [Google Scholar] [Pubmed]
- Rosier PFWM, Kuo HC, Gennaro M, Kakizaki H, Hashim H, van Meel TD, et al. Urodynamic testing. In Abrams P, Cardozo L, Khoury S, Wein A. Incontinence. 5th edition, Paris, 2013; 429-506.
- Abrams P. Bladder outlet obstruction index, bladder contractility index and bladder voiding efficiency: Three simple indices to define bladder voiding function. BJU Int 1999;84:14-15.
[Crossref] [Google Scholar] [Pubmed]
- Blaivas JG, Groutz A. Bladder outlet obstruction nomogram for women with lower urinary tract symptomatology. Neurourol Urodyn 2000;19(5):553-564.
[Crossref] [Google Scholar] [Pubmed]
- Dain L, Auslander R, Rosen T, Segev Y, Goldschmidt E, Abramov Y, et al. Urodynamic findings in women with pelvic organ prolapse and obstructive voiding symptoms. Int J Gynaecol Obstet 2010;111(2):119-121.
[Crossref] [Google Scholar] [Pubmed]
- Serati M, Salvatore S, Siesto G, Cattoni E, Braga A, Sorice P, et al. Urinary symptoms and urodynamic findings in women with pelvic organ prolapse: Is there a correlation? Results of an artificial neural network analysis. Eur Urol 2011;60(2):253-260.
[Crossref] [Google Scholar] [Pubmed]
- Lukacz ES, Santiago-Lastra Y, Albo ME, Brubaker L. Urinary incontinence in women: A review. JAMA 2017;318(16):1592-1604.
[Crossref] [Google Scholar] [Pubmed]
- Fusco F, Abdel-Fattah M, Chapple CR, Creta M, La Falce S, Waltregny D, et al. Updated systematic review and meta-analysis of the comparative data on colposuspensions, pubovaginal slings and midurethral tapes in the surgical treatment of female stress urinary incontinence. Euro Urol 2017;72(4):567-591.
[Crossref] [Google Scholar] [Pubmed]
- Capobianco G, Madonia M, Morelli S, Dessole F, de Vita D, Cherchi PL, et al. Management of female stress urinary incontinence: A care pathway and update. Maturitas 2018;109:32-38.
[Crossref] [Google Scholar] [Pubmed]
- Romanzi LJ, Chaikin DC, Blaivas JG. The effect of genital prolapse on voiding. J Urol 1999;161(2):581-586.
[Crossref] [Google Scholar] [Pubmed]
- Groutz A, Blaivas JG, Chaikin DC. Bladder outlet obstruction in women: Definition and characteristics. Neurourol Urodyn 2000;19(3):213-220.
[Crossref] [Google Scholar] [Pubmed]
- Nguyen JK, Bhatia NN. Resolution of motor urge incontinence after surgical repair of pelvic organ prolapse. J Urol 2001;166(6):2263-2266.
[Crossref] [Google Scholar] [Pubmed]
- Stanton SL, Hilton P, Norton C, Cardozo L. Clinical and urodynamic effects of anterior colporrhaphy and vaginal hysterectomy for prolapse with and without incontinence. Br J Obstet Gynaecol 1982;89(6):459-463.
[Crossref] [Google Scholar] [Pubmed]
- Rosenzweig BA, Soffici AR, Thomas S, Bhatia NN. Urodynamic evaluation of voiding in women with cystocele. J Reprod Med 1992;37(2):162-166.
[Google Scholar] [Pubmed]
- Liang CC, Chang YL, Lin YH, Chang SD. Significance of bladder trabeculation in postmenopausal women with severe pelvic organ prolapse: Clinical and urodynamic assessments. Menopause 2013;20(8):813-817.
[Crossref] [Google Scholar] [Pubmed]
- Basu M, Duckett J. The association of changes in opening detrusor pressure with the resolution of overactive bladder symptoms after repair of pelvic organ prolapse. Neurourol Urodyn 2011;30(4):595-598.
[Crossref] [Google Scholar] [Pubmed]
- Diez-Itza I, Aizpitarte I, Becerro A, Sarasqueta C. Incidence of overactive bladder after vaginal hysterectomy and associated repairs for pelvic organ prolapse. Gynecol Obstet Invest 2009;68(1):65-70.
[Crossref] [Google Scholar] [Pubmed]
- Hannestad YS, Rortveit G, Sandvik H, Hunskaar S. A community-based epidemiological survey of female urinary incontinence: The Norwegian EPINCONT study. J Clin Epidemiol 2000;53(11):1150-1157.
[Crossref] [Google Scholar] [Pubmed]
- Diokno AC, Brock BM, Brown MB, Herzog AR. Prevalence of urinary incontinence and other urological symptoms in the noninstitutionalized elderly. J Urol 1986;136(5):1021-1025.
[Crossref] [Google Scholar] [Pubmed]